Ventricular tachyarrhythmias commonly occur in trained athletes during ambulatory Holter electrocardiography and are usually associated with a benign course. Such arrhythmias have been demonstrated to be sensitive to short periods of athletic deconditioning; however, their response to retraining is not known. Twenty-four hour Holter electrocardiographic monitoring was performed at peak training and after 3 to 6 months of deconditioning and was repeated in the present study after 2, 6, and 12 months of retraining in 37 athletes with frequent and complex ventricular tachyarrhythmias and without cardiovascular abnormalities. These subjects showed partial (101 to 500 ventricular premature complexes [VPCs]/24 hours) or marked (<100 VPCs) reversibility of arrhythmias after deconditioning. Retraining initially resulted in a significant increase in arrhythmia frequency compared with deconditioning (from 280 ± 475 to 1,542 ± 2,186 VPCs; p = 0.005), couplets (0.14 ± 0.42 to 4.4 ± 8.2; p = 0.005), and nonsustained ventricular tachycardia (from 0 to 0.8 ± 1.8; p = 0.02). Subsequently, a progressive reduction was seen in the frequency of all ventricular arrhythmias during the 1 year of training to well below that at the peak training levels (VPCs 917 ± 1,630, couplets 1.8 ± 4.2, and nonsustained ventricular tachycardia 0.4 ± 1.2). Such annual arrhythmia reduction was significantly greater statistically in those athletes with marked reversibility after deconditioning than in the athletes with partial reversibility (69 ± 139 vs 1,496 ± 1,917 VPCs/24 hours, respectively; p = 0.007). No cardiac events or symptoms occurred during 1 year of follow-up. In conclusion, in elite athletes without cardiovascular disease, a resumption in intense training after deconditioning was associated with variable, but prolonged, suppression of ventricular ectopy. The absence of adverse clinical events or symptoms associated with the resumption of training supports the continued eligibility in competitive sports for such athletes and is also consistent with the benign nature of physiologic athlete’s heart syndrome.
Ventricular tachyarrhythmias are not uncommon findings on ambulatory Holter electrocardiogram (ECG) in trained athletes and have usually been associated with benign outcomes in the absence of cardiovascular abnormalities. Such arrhythmias have been demonstrated to be sensitive to short periods of athletic deconditioning and largely independent of training-related physiologic left ventricular (LV) remodeling. However, the course of the ventricular tachyarrhythmias after the resumption of physical training and competition (occurring after a period of complete deconditioning) is unknown. This becomes a relevant issue in clinical practice, because athletes with frequent and complex ventricular arrhythmias in the absence of structural heart disease often represent clinical management dilemmas, including the decisions regarding sports disqualification versus eligibility. The aim of the present study was to assess, in a unique subset of elite athletes, the response and clinical significance of ventricular tachyarrhythmias on resumption of exercise and competition after a forced period of deconditioning.
Methods
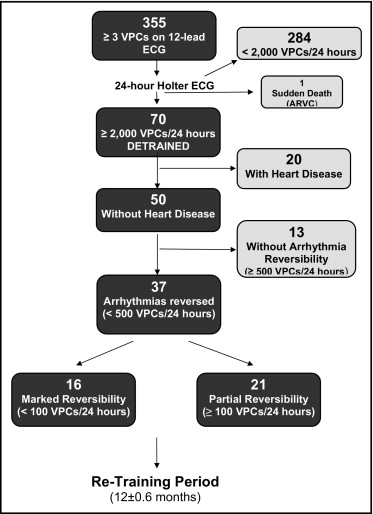
The case records of the Institute of Sports Medicine and Science were reviewed, and 355 athletes who had met the following criteria were selected with 24-hour ambulatory (Holter) ECG: (1) ≥3 ventricular premature complexes (VPCs) on the at rest 12-lead ECG (n = 337); and/or (2) a history of palpitations (n = 18). Of the 355 athletes, 284 with <2,000 VPCs/24 hours, who were allowed to continue in competition and training, were excluded from the present analysis. The remaining 71 athletes with frequent and/or complex ventricular arrhythmias (arbitrarily defined as ≥2,000 VPCs and/or ≥1 burst of nonsustained ventricular tachycardia [NSVT]) were considered for inclusion in the present study. One of these athletes died suddenly from arrhythmogenic right ventricular cardiomyopathy (ARVC) and was excluded because he had not undergone detraining. Of the remaining 70 athletes, 50 were without detectable cardiovascular abnormalities, and the other 20 had structural cardiac diseases, including ARVC (n = 6), mitral valve prolapse (n = 6), myocarditis (n = 4), and dilated cardiomyopathy (n = 4). These latter athletes with cardiac disease were excluded from sports activity (and from the present study) in accordance with the current Italian guidelines. Of the 50 athletes with no cardiovascular abnormalities, 37 (75%) had shown a partial (101 to 500 VPCs/24 hours; n = 21) or marked (<100 VPCs; n = 16) reversibility of the ventricular arrhythmias within the 3- to 6-month period of deconditioning. These 37 athletes resumed training and competition (after deconditioning) for a 1-year period (mean 12 ± 0.6 months) and represent the present study group. The inclusion and exclusion criteria, which have taken into account the criteria of the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement, are presented in Figure 1 .
The study athletes were engaged in a variety of sports disciplines, most commonly soccer (n = 10 [27%]), basketball (n = 6 [16%]), and volleyball (n = 4 [10%]). They also presented a broad spectrum of athletic achievement, with 13 (35%) participating at an elite level, including 9 who had competed in the Olympic Games or World Championships. The mean age of the athletes was 24 ± 10 years (range 18 to 33), and 28 (75%) were men. All athletes were asymptomatic. At the subsequent Holter electrocardiographic monitoring, no athlete was taking antiarrhythmic or other cardioactive medications. The operators who analyzed the Holter ECGs were unaware of the phase of deconditioning or retraining.
The 24-hour ambulatory (Holter) ECGs were initially recorded during the periods of peak training, including conditioning sessions (average 1 hour in duration), similar to that generally performed by the athlete; the remaining time was occupied by the usual daily activities, which could have involved recreational physical activity. The data related to 24-hour Holter ECGs during peak training in the 37 athletes constituting the study group have been previously reported.
The athletes underwent a complete deconditioning period of ≥3 consecutive months (mean 19 ± 6 weeks, range 12 to 24). This period was selected, because it has been previously shown to be sufficient to reverse the cardiovascular adaptations induced by physical training, including LV hypertrophy. After deconditioning, each athlete underwent a second cardiovascular assessment that also included a 24-hour Holter ECG performed under the same conditions as at peak training. The data relative to this deconditioning period have been previously reported. After the period of deconditioning, each athlete resumed competitive sports without restriction, according to the usual program and intensity of their athletic training. Each athlete underwent additional cardiovascular assessments, including 24-hour ambulatory [Holter] ECGs performed under the same conditions as previously, at 2, 6, and 12 months of retraining. These latter 24-hour Holter ECGs included conditioning sessions similar to that performed at the initial (peak training) and second (deconditioning) 24-hour Holter ECGs. The data obtained from the athletes at 2, 6, and 12 months of retraining were compared to those obtained at peak conditioning and at deconditioning.
In the previous study of deconditioning, we assembled as a control group, 148 athletes without structural heart disease, of similar age to the study subjects (26 ± 10 years), with less frequent ventricular arrhythmias (<2,000 VPCs/24 hours, mean 1,211 ± 850, and without NSVT). The 148 controls underwent a second Holter ECG 3 to 6 months after peak training, maintaining the same level of training, and without previous deconditioning. The period between these 2 Holter recordings obtained during training (19 ± 4 weeks, range 12 to 24) was the same as between the active training and deconditioned phases in the 37 athletes of our study group.
The echocardiographic studies were performed at peak training, after deconditioning, and 2.6 and 12 months of retraining using commercially available instruments (Sonos 5500, Philips, Cleveland, Ohio). Images of the heart were obtained in multiple cross-sectional planes using standard transducer positions. The LV cavity dimensions, anterior, ventricular, septal, and posterior free wall thicknesses and left atrial dimensions were obtained from the M-mode echocardiograms, in accordance with previous recommendations. The LV mass was calculated using the formula of Devereux et al and normalized to the body surface area.
The mean, median, and SDs for VPCs, couplets, and NSVT were computed at different points (peak conditioning, deconditioning, and retraining at 2, 6, and 12 months). Comparisons between the mean values were performed using the paired t test or Mann-Whitney U test, as appropriate. The same analyses were performed in the 2 subgroups of athletes with either partial (≥100 VPCs/24 hours) or marked (<100 VPCs/24 hours) reversibility of arrhythmias after deconditioning. The data were then log transformed (to achieve approximately normal distributions), and the differences in VPCs at retraining (2, 6, and 12 months) were compared with those at deconditioning. Finally, we applied a linear regression model (to avoid the problem of multiple testing) to assess the relation of VPC frequency with retraining at 2, 6, and 12 months and at deconditioning.
Results
At the initial assessment, during the peak training period, the frequency of VPCs/24 hours was 2,140 to 43,221 (mean 10,405 ± 9,605; Table 1 and Figure 2 ). Of the 37 athletes, 23 (62%) had ≥1 couplet (mean 35.2 ± 73, range 1 to 321); 21 (57%) also had 1 to 179 bursts of NSVT (mean 7.7 ± 29.5), consisting of 3 to 28 consecutive beats, at a heart rate of 130 to 270 beats/min.
| Variable | Peak Conditioning | Deconditioning | Retraining (months) | ||
|---|---|---|---|---|---|
| 2 | 6 | 12 | |||
| Ventricular premature complexes | 10,405 ± 9,605 (2,140–43,221) | 280 ± 475 ⁎ (0–2,342) | 1,542 ± 2,186 † (0–9,069) | 1,087 ± 1,830 † (0–7,780) | 917 ± 1,630 ‡ (0–8,029) |
| Couplets | 35.2 ± 73 (1–321) | 0.14 ± 0.42 ⁎ (0–2) | 4.4 ± 8.2 † (0–34) | 3.0 ± 5.6 † (0–22) | 1.8 ± 4.2 ‡ (0–20) |
| Nonsustained ventricular tachycardia | 7.7 ± 29.5 (1–179) | 0.08 ± 0.5 ⁎ (0–3) | 0.8 ± 1.8 ‡ (0–10) | 0.6 ± 1.6 (0–8) | 0.4 ± 1.2 (0–7) |
⁎ p <0.005 deconditioning versus peak conditioning;
† p <0.005 retraining at 2 and 6 months versus deconditioning;
‡ p <0.02 retraining at 2, 6, and 12 months versus deconditioning.
After the deconditioning period, the study group showed a significant reduction in VPCs (98%), couplets (98%), and NSVT (100%; p <0.005 with respect to peak training). The individual subject analysis showed that after deconditioning, all 37 athletes had either partial (≥100 to 500 VPCs/24 hours; n = 21) or marked (<100 VPCs; n = 16) reversibility of ventricular tachyarrhythmias ( Figure 2 ). Only 4 of 23 athletes showed the persistence of ventricular couplets after deconditioning (3 athletes had 1 couplet/24 hours and 1 athlete had 2 couplets/24 hours). None of the 21 athletes with NSVT at peak training had NSVT after deconditioning. After deconditioning, the athletes resumed their training programs and participated in competitive sports events without restriction.
After 2 months of retraining, the number of VPCs significantly increased compared to that at deconditioning to 1,542 ± 2,186 (p <0.005; 80% change). The number of couplets increased to 4.4 ± 8.2 (p <0.005; 95% change) and NSVT to 0.8 ± 1.8 (p <0.02; 90% change). Nevertheless, the VPC, couplet, and NSVT frequency remained at significantly less than that peak training levels (p <0.01; Table 1 ). Individual subject analysis showed a significant increase in ventricular tachyarrhythmias within 2 months of retraining in 18 athletes (49% change; to 500 to 2,000 VPCs/24 hours; p <0.001 compared with deconditioning), including 9 with a marked increase in this arrhythmia (to >2,000 VPCs/24 hours). The remaining 19 athletes showed nonsignificant change in VPCs with respect to the deconditioning period (to 0 to 500 VPCs/24 hours; p = 0.78; Figure 2 ). Couplets significantly reappeared compared to the deconditioning levels after 2 months of retraining in 18 athletes (48% change; from 1 to 34 couplets/24 hours; p = 0.002) and NSVT in 13 athletes (35% change; from 1 to 10 episodes of NSVT/24 hours; p = 0.0001). Increased arrhythmia frequency at 2 months of retraining was greater in the athletes with previous partial reversibility of VPC frequency than in those with marked reversibility (2,054.6 ± 2,446 vs 790.2 ± 1,514 VBCs/24 hours; p = 0.084; Table 2 ).
| Variable | VPCs | p Value | |
|---|---|---|---|
| Athletes With Marked Reversibility (<100 VPCs/24 hours; n = 16) | Athletes With Partial Reversibility (≥100 VPCs/24 hours; n = 21) | ||
| Peak training | 12,470 ± 12,193 (2,140–43,221) | 8,996.4 ± 7,343 (2,235–25,580) | 0.28 |
| Deconditioning | 14.6 ± 24 (0–63) | 281.4 ± 109 (120–498) | 0.0001 |
| Retraining (months) | |||
| 2 | 790.2 ± 1,514 (0–5,032) | 2,054.6 ± 2,446 (65–9,069) | 0.084 |
| 6 | 139.4 ± 216 (0–785) | 1,734.4 ± 2,152 (4–7) | 0.007 |
| 12 | 69.3 ± 139 (0–552) | 1,496.0 ± 1,917 (11–8,029) | 0.007 |
After 6 months of retraining, the VPCs showed a decrease to 1,087 ± 1,830 (i.e., 30% change with respect to that at 2 months of retraining; Figure 2 ). A similar trend was evident for complex arrhythmias, with couplets decreasing to 3.0 ± 5.6 (32% change compared with at 2 months of retraining) and NSVT to 0.6 ± 1.6 (25% change). After 6 months of retraining, the VPC, couplet, and NSVT frequency remained at significantly less than peak training levels (p <0.01). Individual subject analysis showed no significant changes from 2 to 6 months in the number of athletes with 500 to 2,000 VPCs/24 hours (from 19 to 15 athletes; p = 0.53). No difference was also found in those athletes who showed a marked increase of arrhythmia at 2 months of retraining (to >2,000 VPCs/24 hours) (from 9 athletes at 2 months to 8 athletes at 6 months of retraining; p = 0.94). Athletes with less-frequent ventricular arrhythmias (0 to 500 VPCs/24 hours) remained substantially unchanged from 2 to 6 months of retraining (18 vs 22 athletes, respectively; p = 0.52; Figure 2 ). The number of athletes with couplets and NSVT showed no significant variation from 2 to 6 months of retraining (from 18 to 16 athletes, p = 0.91; and from 13 to 11 athletes, p = 0.83, respectively). Furthermore, individual subject analysis showed that the 16 athletes with marked reversibility of ventricular tachyarrhythmias after deconditioning had a significantly greater decrease in arrhythmias at 6 months of retraining (to 139.4 ± 216 VPCs/24 hours) compared to that of the 21 athletes with only partial reversibility, for whom this arrhythmia remained consistent (1,734.4 ± 2,152 VPCs; p = 0.007; Table 2 ).
After 1 year of retraining, VPCs continued to decrease to 917 ± 1,630 (i.e., 16% change with respect to 6 months of retraining; Figure 2 ). Couplets and NSVT also showed an additional decrease to 1.8 ± 4.2 (40% change compared to that at 6 months of retraining) and to 0.4 ± 1.2 (35% change), respectively. VPCs, couplets, and NSVT continued to remain at significantly less than the peak training levels (p <0.01; Table 1 ). Individual subject analysis showed no significant changes from 6 to 12 months in athletes with 500 to 2,000 VPCs/24 hours (from 15 to 14 athletes; p = 0.97). A not significant reduction was found in the athletes who showed a marked increase of arrhythmia at 2 months of retraining (to >2,000 VPCs/24 hours; from 8 athletes at 6 months to 4 athletes at 12 months of retraining; p = 0.21). The athletes with less-frequent ventricular arrhythmias (0 to 500 VPCs/24 hours) remained substantially unvaried from 6 to 12 months of retraining (22 vs 23 athletes, respectively; p = 0.97; Figure 2 ). Also, the athletes with couplets and NSVT did not show a significant variation from 6 to 12 months (from 16 to 11 athletes, p = 0.36; and from 11 to 7 athletes, p = 0.40, respectively). Furthermore, individual subject analysis showed that athletes with marked reversibility of arrhythmias with deconditioning continued to have a more prolonged suppression of VPCs at 1 year of retraining compared to athletes with partial reversibility (69 ± 139 vs 1,496 ± 1,917 VPCs; p = 0.007; Table 2 ). Linear regression analysis applied to the differences in VPC frequency between deconditioning and the 3 phases of retraining showed a statistically significant association between retraining at 6 and 12 months compared to that at deconditioning.
Of the 37 athletes, 30 (81%) showed a pattern of VPC morphology consistent with a right ventricular outflow tract origin and 7 a fascicular origin (19%). Of the 30 athletes with a right ventricular origin of VPCs, 28 had an inferior axis and 2 showed an indeterminate axis. Ventricular arrhythmias with marked reversibility showed a right ventricular outflow tract origin, with an inferior axis in all 16 athletes.
At peak training, the LV mass index was 114 ± 23 g/m 2 . After deconditioning, it had decreased to 94 ± 19 g/m 2 (p <0.001). During retraining, the LV mass index had increased to 96 ± 18 g/m 2 at 2 months (p = 0.61), 101 ± 21 g/m 2 at 6 months (p = 0.27), and 110 ± 19 g/m 2 at 12 months (p <0.05). The changes in LV mass index with training did not differ between the 18 athletes who experienced a reappearance of ventricular tachyarrhythmias with retraining and the 19 athletes without a reappearance of arrhythmias (95 ± 11 vs 96 ± 10 g/m 2 at 2 months of retraining, p = 0.55). No significant structural or functional abnormality of the right ventricle was identified in any athlete.
No cardiac events or symptoms occurred in the athletes with or without a reappearance of ventricular tachyarrhythmias during the 1-year follow-up period, during which training and competition had been resumed.
The cardiovascular evaluations with at rest and exercise ECGs and 2-dimensional echocardiography at 2, 6, and 12 months of retraining in all athletes and selectively with cardiac magnetic resonance (n = 30), signal-averaged electrocardiography (n = 37), programmed ventricular stimulation (n = 13), and myocardial biopsy (n = 2) did not detect previously unrecognized cardiovascular abnormalities in any athlete. Only 2 of the 37 athletes incurred ventricular tachyarrhythmias during exercise testing; the remaining 35 athletes had a complete disappearance of arrhythmia during exercise. No athlete experienced cardiac symptoms during exercise testing. In the 13 athletes who underwent an electrophysiologic study, either no arrhythmia or only a nonsustained ventricular response (3 to 5 consecutive ectopic beats) was induced by programmed ventricular stimulation. None of the athletes underwent radiofrequency catheter ablation.
In the 148 control athletes, who had not modified their physical conditioning, no significant variability in ventricular arrhythmias was found between the 2 ambulatory Holter ECGs obtained during training (19 ± 4 weeks apart during the training period). The mean number of VPCs on the first Holter ECG was 1,211 ± 850 and was 1,050 ± 648 on the second (p = 0.28). Also, no significant difference was found with regard to couplets and NSVT (0 vs 0).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


