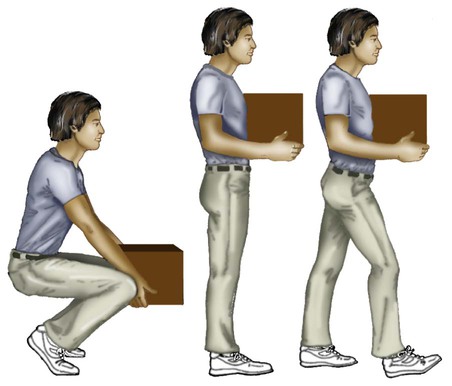
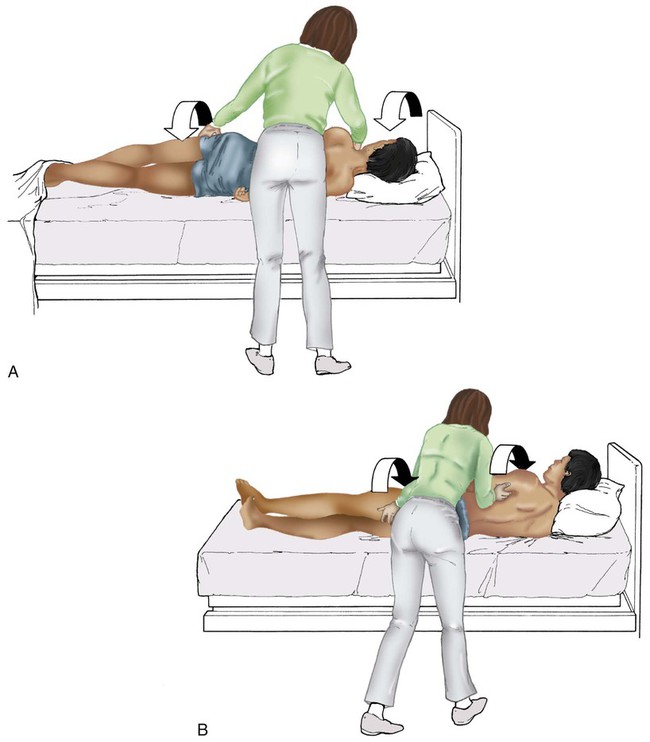
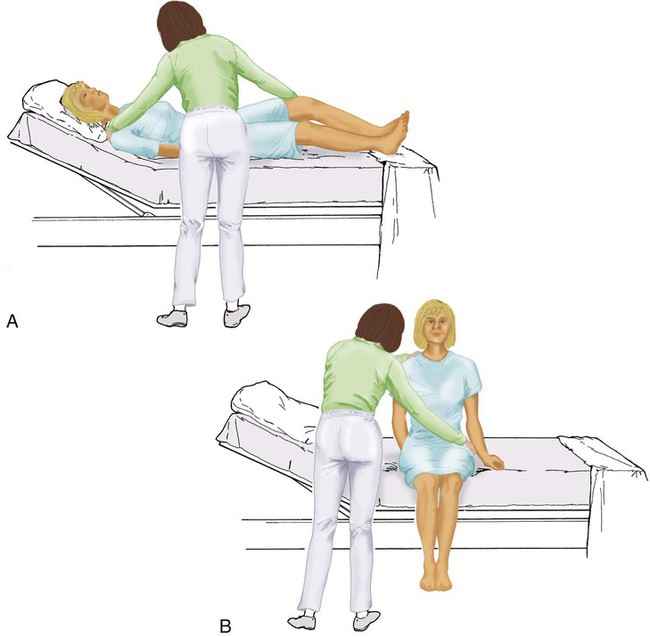
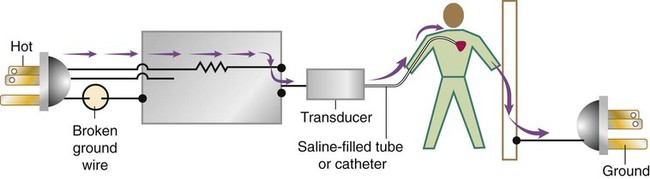
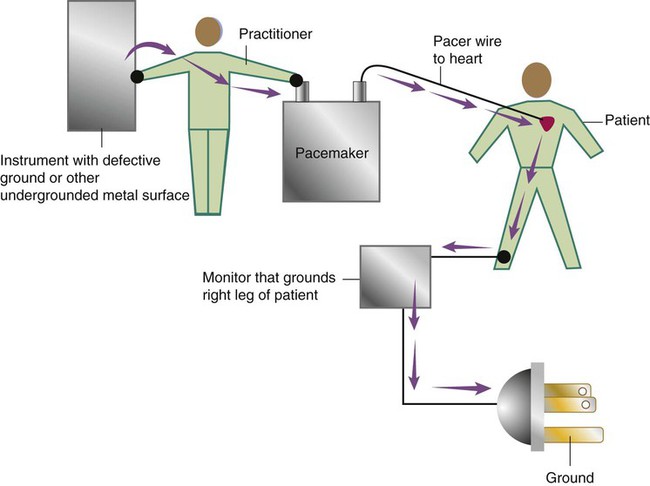
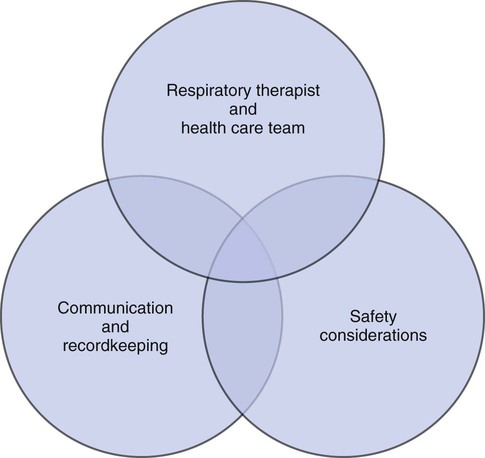
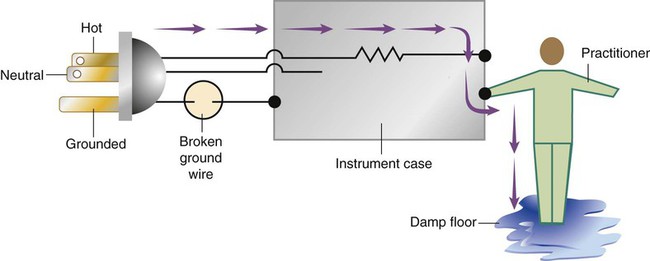
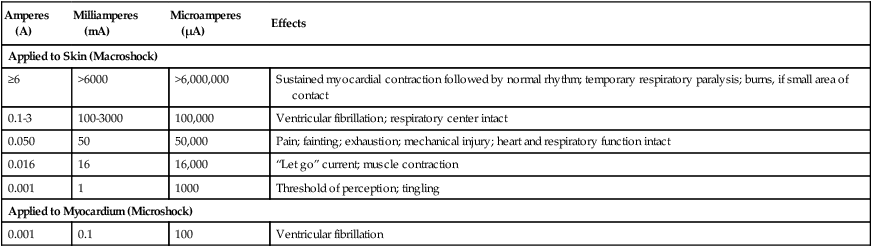
After reading this chapter you will be able to: Respiratory therapists (RTs) share the general responsibilities for providing a safe and effective health care environment with nurses and other members of the health care team. The continuum of patient safety requires that the RT have specific technical knowledge of the environment of direct patient care. In addition to technical skills, all health care professionals must be able to communicate effectively with each other and with patients and patients’ families and to document pertinent information. Figure 3-1 shows this relationship for patient safety. This chapter provides the foundation knowledge needed to assume these general aspects of patient care effectively. Posture involves the relationship of the body parts to each other. A person needs good posture to reduce the risk of injury when lifting patients or heavy equipment. Poor posture may place inappropriate stress on joints and related muscles and tendons. Figure 3-2 illustrates the correct body mechanics for lifting a heavy object. The correct technique calls for a straight spine and use of the leg muscles to lift the object. Figure 3-3 shows the correct technique for lateral movement of a bed-bound patient. Figure 3-4 illustrates the ideal method for moving a conscious patient toward the head of a bed. Figure 3-5 shows the proper technique for assisting a patient to the bedside position for dangling his or her legs or transfer to a chair. Ambulation (walking) helps maintain normal body function. Extended bed rest can cause numerous problems, including bed sores and atelectasis (low lung volumes). Ambulation should begin as soon as the patient is physiologically stable and free of severe pain. Ambulation has been shown to reduce the length of hospital stay after surgery and in patients recovering from community-acquired pneumonia.1,2 Safe patient movement includes the following steps: 1. Place the bed in a low position and lock its wheels. 2. Place all equipment (e.g., intravenous [IV] equipment, nasogastric tube, surgical drainage tubes) close to the patient to prevent dislodgment during ambulation. 3. Move the patient toward the nearest side of bed. 4. Assist the patient to sit up in bed (i.e., arm under nearest shoulder and one under farthest armpit). 5. Place one hand under the patient’s farthest knee, and gradually rotate the patient so that his or her legs are dangling off the bed. 6. Let the patient remain in this position until dizziness or lightheadedness lessens (encouraging the patient to look forward rather than at the floor may help). 7. Assist the patient to a standing position. 8. Encourage the patient to breathe easily and unhurriedly during this initial change to a standing posture. 9. Walk with the patient using no, minimal, or moderate support (moderate support requires the assistance of two practitioners, one on each side of the patient). 10. Limit walking to 5 to 10 minutes for the first exercise. Because current is most important, you should be familiar with the equation used to calculate it: Currents of 12 mA would cause a tingling sensation but no physical damage. Figure 3-6 shows how current can flow through the body. In this case, a piece of electrical equipment is connected to AC line power via a standard three-prong plug. However, unknown to the practitioner, the cord has a broken ground wire. Normally, current leakage from the equipment would flow back to the ground through the ground wire. However, this pathway is unavailable. Instead, the leakage current finds a path of low resistance through the practitioner to the damp floor (an ideal ground). Current can readily flow into the body, causing damage to vital organs when the skin is bypassed via conductors such as pacemaker wires or saline-filled intravascular catheters (Figures 3-7 and 3-8). Even urinary catheters can provide a path for current flow. The heart is particularly sensitive to electrical shock. Ventricular fibrillation can occur when currents of 20 µA (20 microamperes, or 20 millionths of 1 ampere) are applied directly to the heart. Electrical shocks are classified into two types: macroshock and microshock. A macroshock exists when a high current (usually >1 mA) is applied externally to the skin. A microshock exists when a small, usually imperceptible current (<1 mA) bypasses the skin and follows a direct, low-resistance path into the body. Patients susceptible to microshock hazards are termed electrically sensitive or electrically susceptible. Table 3-1 summarizes the different effects of these two types of electrical shock. TABLE 3-1 *Physiologic effects of AC shocks applied for 1 second to the trunk or directly to the myocardium. In 1980, approximately 13,000 health care facility fires were officially reported in the United States.3 During the period 2004-2006, the average annual number of fires in health care facilities was 6400.4 This significant reduction in health care facility fires is primarily due to education and enforcement of strict fire codes. About 23% of fires in health care facilities occur in hospitals, and 44% occur in nursing homes; the most common site of origin of the fire is the kitchen.3 About 15% of hospital fires start in patient care rooms and are usually due to patients or visitors smoking or using open flames to light tobacco products. Medical facility fires cause an annual average of five civilian deaths and approximately $34 million in damage.4
Patient Safety, Communication, and Recordkeeping
 Describe how to apply good body mechanics and posture to moving patients.
Describe how to apply good body mechanics and posture to moving patients.
 Describe how to ambulate a patient and the potential benefits of ambulation.
Describe how to ambulate a patient and the potential benefits of ambulation.
 Write definitions of key terms associated with electricity, including voltage, current, and resistance.
Write definitions of key terms associated with electricity, including voltage, current, and resistance.
 Identify the potential physiologic effects that electrical current can have on the body.
Identify the potential physiologic effects that electrical current can have on the body.
 State how to reduce the risk of electrical shock to patients and yourself.
State how to reduce the risk of electrical shock to patients and yourself.
 Identify key statistics related to the incidence and origin of hospital fires.
Identify key statistics related to the incidence and origin of hospital fires.
 List the conditions needed for fire and how to minimize fire hazards.
List the conditions needed for fire and how to minimize fire hazards.
 Identify impediments to care and risk in the direct patient environment.
Identify impediments to care and risk in the direct patient environment.
 State how communication can affect patient care.
State how communication can affect patient care.
 Describe the two patient identifier system.
Describe the two patient identifier system.
 List the factors associated with the communication process.
List the factors associated with the communication process.
 Describe how to improve your communication effectiveness.
Describe how to improve your communication effectiveness.
 Describe how to recognize and help resolve interpersonal or organizational sources of conflict.
Describe how to recognize and help resolve interpersonal or organizational sources of conflict.
 List the common components of a medical record.
List the common components of a medical record.
 State the legal and practical obligations involved in recordkeeping.
State the legal and practical obligations involved in recordkeeping.
Safety Considerations
Patient Movement and Ambulation
Basic Body Mechanics
Moving the Patient in Bed
Ambulation
Electrical Safety
Fundamentals of Electricity
Amperes (A)
Milliamperes (mA)
Microamperes (µA)
Effects
Applied to Skin (Macroshock)
≥6
>6000
>6,000,000
Sustained myocardial contraction followed by normal rhythm; temporary respiratory paralysis; burns, if small area of contact
0.1-3
100-3000
100,000
Ventricular fibrillation; respiratory center intact
0.050
50
50,000
Pain; fainting; exhaustion; mechanical injury; heart and respiratory function intact
0.016
16
16,000
“Let go” current; muscle contraction
0.001
1
1000
Threshold of perception; tingling
Applied to Myocardium (Microshock)
0.001
0.1
100
Ventricular fibrillation
Fire Hazards
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Patient Safety, Communication, and Recordkeeping