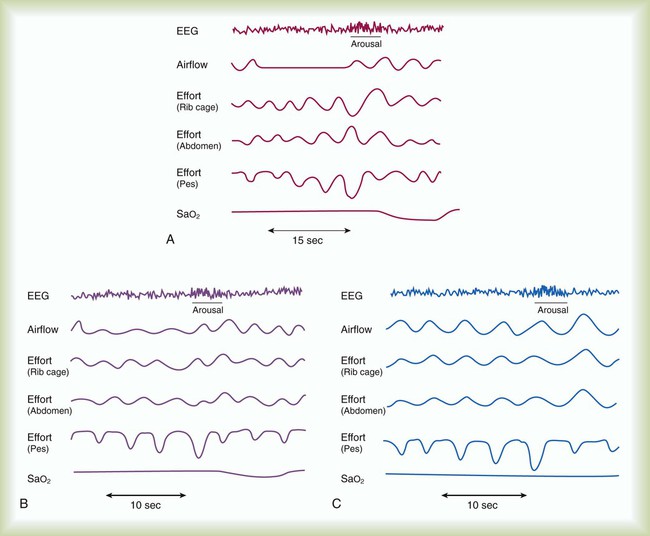
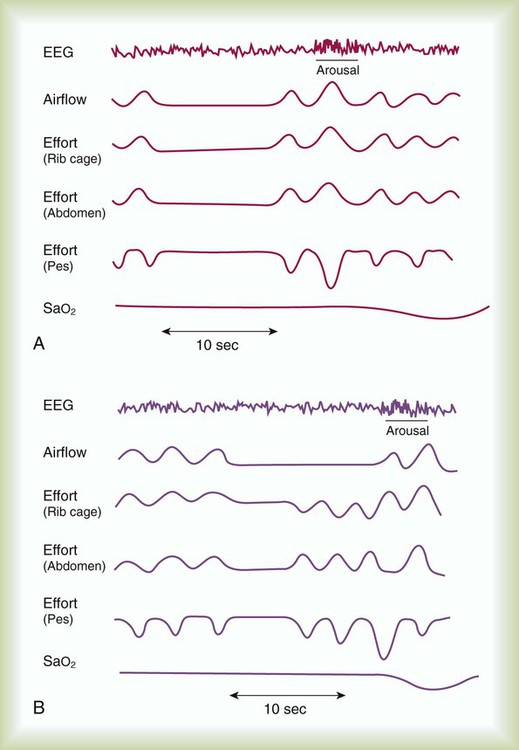
After reading this chapter you will be able to: Obstructive sleep apnea (OSA) syndrome is a common clinical problem that is underdiagnosed.1 It is estimated that approximately 2% to 4% of adults have OSA.2 This prevalence is equivalent to asthma and diabetes in the general population. The spectrum of disease ranges from sleep disruption related to increased airway resistance to profound daytime sleepiness in conjunction with severe oxyhemoglobin desaturation, pulmonary hypertension, and right heart failure. The common feature in all variants of OSA syndrome is sleep disruption secondary to increased ventilatory effort that results in daytime hypersomnolence (Figure 30-1).3 Treatment decreases morbidity and mortality. Sleep apnea is defined as repeated episodes of complete cessation of airflow for 10 seconds or longer. The events can be obstructive (caused by upper airway closure) or central (caused by lack of ventilatory effort). Primary central nervous system lesions, stroke, congestive heart failure, and high-altitude hypoxemia can diminish respiratory control and cause central apnea events.3 Central sleep apnea (CSA) is not as common as OSA. Only 10% to 15% of patients with sleep-disordered breathing are classified as having CSA.4 Mixed sleep apnea has an initial central component followed by an obstructive component (Figure 30-2). Hypopnea is a significant decrease in breathing without complete cessation of airflow.5 Hypopnea is defined as a 30% decrease in airflow in conjunction with 4% oxygen (O2) desaturation.6 Most investigators agree that physiologically significant hypopnea is associated with a decrease in O2 saturation or arousal from sleep.7 The primary cause of OSA is a small or unstable pharyngeal airway. This condition can be caused by soft tissue factors, such as upper body obesity or tonsillar hypertrophy (rare in adults), and skeletal factors, such as a small or recessed chin.8 During the waking state, pharyngeal patency is maintained by increased activity of the upper airway dilator muscles. Sleep onset is associated with a decrease in the activity of these muscles. The result is airway narrowing or closure of airways that are at risk.9 In an unstable upper airway, narrowing and closure during sleep may involve multiple sites.10 Partial or complete closure of the upper airway during sleep has many serious neurobehavioral, metabolic, and cardiopulmonary consequences (Box 30-1). Compared with the general population, patients with untreated OSA have an increased risk of systemic and pulmonary hypertension, stroke, nocturnal arrhythmia, heart failure, and myocardial infarction.11,12 The repetitive cycle of upper airway closure and opening during sleep is believed to have effects on the autonomic nervous system, specifically, an increase in sympathetic tone.13 These effects are caused in part by episodes of hypoxemia and hypercapnia that are due to airway closure and hypoventilation that can occur throughout the night in patients with OSA. The arousals and microarousals during sleep also play an important role in the increase in sympathetic tone.13 Over time, increased sympathetic tone may result in systemic and modest pulmonary hypertension.14 Patients with OSA may have right ventricular hypertrophy and right heart failure if they are not treated.15,16 Obesity, especially of the upper body, has been found to correlate positively with the presence of OSA. In most instances, patients with OSA are obese with a large amount of peripharyngeal tissue and adipose tissue in the neck.17 A body mass index greater than 28 (>120% of ideal body weight normalized for height) should alert the practitioner to the possibility of OSA, particularly if the patient has excessive daytime sleepiness (EDS).2 Patients who are of normal body weight can be predisposed to OSA if they have an abnormal craniofacial configuration. Men often grow a beard to disguise such a craniofacial abnormality. If the chin is recessed (retrognathic) or small (micrognathic), the upper airway space may be narrow, and the risk of airway closure during sleep increases.2,8,14 Patients with a deviated nasal septum or trauma to the nasal passages may be predisposed to upper airway closure during sleep as a result of the increased resistive load to the upper airway. An isolated nasal abnormality is an unusual cause of OSA. OSA may have a genetic predisposition.18 There have been reports of families in which obesity alone does not explain the increased prevalence of OSA.19 It has been postulated that craniofacial abnormalities and defects in ventilatory control explain the increased frequency of OSA in these families. Although a detailed discussion of the pathophysiology of CSA is beyond the scope of this chapter, several concepts are important to RTs. In contrast to OSA, which represents a spectrum of the same disease, CSA is a heterogeneous group of disorders. Patients have a ventilatory pattern known as periodic breathing, in which there is a waxing and waning of respiratory drive, which is reflected clinically as an increase and then a decrease in respiratory rate and tidal volume (VT). Cheyne-Stokes respiration, which often occurs in patients with congestive heart failure or stroke, is a severe type of periodic breathing characterized by a crescendo-decrescendo pattern of hyperpnea alternating with apnea. After apnea occurs, there may be an increase in central ventilatory drive and an increase in VT.3 Some patients with chronic obstructive pulmonary disease (COPD) have coexisting OSA. This combination is referred to as overlap syndrome.20 Patients are usually obese and have a history of smoking. They have moderate to severe nocturnal oxyhemoglobin desaturation secondary to both OSA and COPD. The worst desaturation values occur during rapid eye movement (REM) sleep and are related to the loss of accessory muscle use encountered in this physiologic state. Patients with overlap syndrome tend to have a worse prognosis and more severe blood gas abnormalities than patients with the same degree of OSA but without COPD.20 They may arrive in the intensive care unit with a “COPD exacerbation” and decompensated right heart failure. Undiagnosed OSA complicates the course at night with arousals, increased dyspnea, and O2 desaturation values resistant to supplemental O2.20 Patients with sleep apnea are more commonly men (three times greater frequency than among women), are older than 40 years, and have hypertension (Box 30-2). Most patients with sleep apnea report habitual snoring that has become progressively worse.2,21 Sensations of nocturnal choking, gasping, or resuscitative snorting are frequently reported. If a bed partner observes periods of apnea, the diagnosis of OSA is highly likely. Patients with OSA have arousals from sleep and sleep fragmentation, which can lead to fatigue, EDS, and irritability.22 Patients who have an increased frequency of awakenings and microarousals have more daytime sleepiness and greater difficulty with daytime functioning than the general population.23 Patients with OSA may have neuropsychologic deficits and impairment in vigilance.24 Compared with the general population, untreated OSA patients are at increased risk of motor vehicle accidents because of EDS.25–27 The physical examination of most patients reveals evidence of obesity, particularly in the upper body. Upper body obesity can be quantitated with neck size. A neck circumference of 42 cm (16.5 in) increases the likelihood of the diagnosis of sleep apnea.14 Examination of the oropharynx frequently reveals a long soft palate. Although tonsillar hypertrophy is common in children with sleep apnea, it is seldom found in adults. Large palatine tonsils may increase the risk of airway closure during sleep. A retrognathic or micrognathic mandible can narrow the pharyngeal airway, placing a patient of normal weight at risk of airway closure during sleep.8 The cardiovascular examination may reveal evidence of pulmonary hypertension or right heart failure (lower extremity edema).28,29 These findings are determined primarily by the hypoxic burden experienced by the patient. Pulmonary hypertension or right heart failure is more commonly encountered in patients with concomitant daytime hypoxemia. Patients with OSA and COPD or severe obesity (body mass index greater than 40) appear to be at particular risk of this complication.30 Recurrent moderate to severe oxyhemoglobin desaturation and resaturation secondary to OSA can be associated with an increased incidence of cardiac arrhythmia.31,32 Repeated nocturnal desaturation can be a cause of secondary polycythemia.14,33 OSA and poor sleep quality are also associated with metabolic syndrome independent of obesity.34,35 Metabolic syndrome includes three of the following: waist circumference 102 cm or greater in men or 88 cm or greater in women, hypertension, impaired glucose tolerance, insulin resistance, and elevated triglycerides.36,37 These interactions can also increase the patient’s cardiac risks and increased morbidity and mortality from cardiovascular disease.12,38 In the acute care setting, patients frequently present with previously undiagnosed OSA and can pose a particular challenge for diagnosis and management.39–41 A high clinical suspicion for OSA in the hospital setting is necessary because untreated or unrecognized OSA can complicate recovery from acute illness, trauma, heart failure, and recent surgery.42–45 Patients with known OSA are frequently not placed on continuous positive airway pressure (CPAP) while in the hospital or may require a temporary adjustment in pressure settings.46 Patients who are unstable for testing in a sleep laboratory can undergo portable bedside testing or empiric treatment with positive pressure if the diagnosis cannot be confirmed.47 Outpatient follow-up with confirmatory sleep evaluation is important for long-term treatment and compliance. In obstructive apnea or hypopnea, airflow is absent or decreased in the presence of continued ventilatory effort. Asynchronous (paradoxical) movement of the abdomen and rib cage can be observed. O2 desaturation may or may not occur. The degree of the O2 desaturation depends on the length of the apneic event or the patient’s baseline saturation (see Figure 30-1). Respiratory effort–related arousals are characterized by increased respiratory effort, leading to arousal from sleep that does not meet the criteria of an apneic or a hypopneic event (see Figure 30-1).48,49 Measuring devices that are adequate for assessing hypopnea also are adequate for assessing apnea; however, devices used for measuring apnea cannot always detect hypopnea. The diagnosis of hypopnea may be affected by the measurement technique used. In 1999, an American Academy of Sleep Medicine (AASM) task force conducted an evidence-based review of measurement techniques for detection of hypopnea.50 The scoring system was as follows: A, good to excellent agreement with a reference standard (face mask pneumotachygraph); B, limited data, but good theoretical framework and clinical experience suggest the method is valid; C, no data, weak theoretical framework or clinical experience; and D, research or clinical experience suggests the method is invalid. The measuring techniques were scored as follows: nasal pressure, B; respiratory inductance plethysmography (RIP) with sum of chest and abdominal signals, B; dual-channel RIP, C; single-channel RIP, C; piezoelectricity sensors, strain gauges, and thoracic impedance, D; breathing measurement signal with a desaturation or arousal, B; expired carbon dioxide (CO2), D; and thermal sensors, D. A face mask pneumotachygraph allows the greatest precision in measuring airflow, but it is poorly tolerated. Nasal pressure is a reliable way to detect hypopnea and is well tolerated by patients undergoing a diagnostic PSG.5,50 After the sleep study is completed, the sleep technologist scores it. The number of apneas and of hypopneas per hour of sleep are reported as an apnea-hypopnea index (AHI) or respiratory disturbance index (RDI). The AASM has operationally defined the severity of OSA as follows: mild, AHI 5 to 15; moderate, AHI 15 to 30; severe, AHI greater than 30. AHI less than 5 is considered within the normal range for adults. The number of arousals per hour (arousal index), percentage of each sleep stage, frequency of O2 desaturation, mean O2 saturation, and nadir of O2 saturation also are reported (Box 30-3). Abbreviated (portable) cardiopulmonary testing has been used to confirm a diagnosis of OSA. These studies do not record the electrophysiologic signals (EEG, EOG, and EMG) required to stage and score sleep. The portable studies vary in the type and number of cardiopulmonary values recorded. Controversy exists whether portable systems are sufficient to diagnose OSA. Many variables, such as airflow, ventilatory effort, sleep stage, and O2 saturation values, may be less precise or may not be measured at all with these devices. Currently, portable monitoring for the diagnosis of OSA is acceptable in patients with high pretest probability but without significant comorbidities that may affect the accuracy of testing.51 Excerpts of American Association for Respiratory Care (AARC) Clinical Practice Guidelines for a PSG are provided in Clinical Practice Guideline 30-1. Management of OSA should be individualized but generally can be classified into three options: behavioral, medical, and surgical interventions.52 Behavioral therapy should be pursued in the care of all patients. Medical therapy and surgical therapy must be tailored to the individual patient. The likelihood of acceptance of and adherence to the prescribed therapeutic intervention must be considered. The goals of treatment are to normalize O2 saturation and ventilation; eliminate apnea, hypopnea, and snoring; and improve sleep architecture and continuity (Box 30-4).
Disorders of Sleep
 Define obstructive sleep apnea (OSA).
Define obstructive sleep apnea (OSA).
 Identify why airway closure occurs only during sleep.
Identify why airway closure occurs only during sleep.
 State the long-term consequences of uncontrolled OSA.
State the long-term consequences of uncontrolled OSA.
 State how a diagnosis of OSA is made.
State how a diagnosis of OSA is made.
 Identify what groups of patients are at particular risk of OSA.
Identify what groups of patients are at particular risk of OSA.
 State what treatments are available for patients with OSA.
State what treatments are available for patients with OSA.
 Describe how continuous positive airway pressure (CPAP) works.
Describe how continuous positive airway pressure (CPAP) works.
 Identify problems associated with CPAP.
Identify problems associated with CPAP.
 Determine when bilevel pressure is useful in the treatment of OSA.
Determine when bilevel pressure is useful in the treatment of OSA.
 Identify the surgical alternatives for patients with severe OSA.
Identify the surgical alternatives for patients with severe OSA.
Pathophysiology
Obstructive Sleep Apnea
Central Sleep Apnea
Overlap Syndrome
Clinical Features
Laboratory Testing
Treatment
Disorders of Sleep