1 Patient Assessment and Care Management
Note 1: This book is written to cover every item listed as testable on the Entry Level Examination (ELE), Written Registry Examination (WRE), and Clinical Simulation Examination (CSE).
The listed code for each item is taken from the National Board for Respiratory Care’s (NBRC) Summary Content Outline for CRT (Certified Respiratory Therapist) and Written RRT (Registered Respiratory Therapist) Examinations (http://evolve.elsevier.com/Sills/resptherapist/). For example, if an item is testable on both the ELE and WRE, it is shown simply as (Code: …). If an item is testable only on the ELE, it is shown as (ELE code: …). If an item is testable only on the WRE, it is shown as (WRE code: …).
Note 3: The Entry Level Examination has shown an average of 2 questions that directly cover a cardiopulmonary pathology issue; the Written Registry Examination has shown an average of 1 question. It is beyond the scope of this book to cover all the cardiopulmonary diseases and conditions that befall patients for whom respiratory therapists may provide care. It is recommended that asthma, chronic obstructive pulmonary disease (COPD; emphysema or chronic bronchitis or both), pneumonia, pneumothorax, flail chest, congestive heart failure with pulmonary edema, myasthenia gravis, Guillain-Barré syndrome, head (brain) injury with increased intracranial pressure, pediatric croup and epiglottitis, infant respiratory distress syndrome, acute respiratory distress syndrome (ARDS), and smoke inhalation with carbon monoxide poisoning be studied. Some limited discussion of these topics is covered in this book. The Written Registry Examination frequently ask questions about the respiratory therapy procedures that patients with these types of problems are receiving. In addition, the 11 Clinical Simulation Examination scenarios are built around the care of patients with these types of diseases and conditions. See Box 1 in the Introduction.
MODULE A
1. Review the patient’s history: present illness, admission notes, progress notes, diagnoses, respiratory care orders, medication history, do not resuscitate (DNR) status, and previous patient education (Code: IA1) [Difficulty: ELE is R; WRE: Ap]
a. Patient history
Review the complete initial patient history and note the following:
d. Diagnoses
After the medical history, physical exam, and laboratory tests are completed, the patient will be placed into one of the following four diagnostic categories. Refer to Table 1-1 for examples of each category:
TABLE 1-1 Patient Illness Categories
| Category | Examples |
|---|---|
| Crisis/acute onset of illness | Trauma, heart attack, allergic reaction, aspiration of a foreign body, pneumothorax, pulmonary embolism, and some pneumonias |
| Intermittent but repeated Illness | Asthma, chronic bronchitis, congestive heart failure, angina pectoris, myasthenia gravis, and some pneumonias |
| Progressive worsening | Congestive heart failure, chronic bronchitis, emphysema, and upper respiratory tract infection leading to bronchitis or pneumonia |
| Mixed patterns/multiple problems | Chronic obstructive pulmonary disease and cystic fibrosis complicated by multiple problems, mucous plugging or infection; mixes of congestive heart failure and chronic lung disease; mixes of neuromuscular and lung disease; mixes of renal failure and congestive heart failure with chronic lung disease |
2. Review the results of the patient’s physical examination and vital signs (Code: IA2) [Difficulty: ELE: R; WRE: Ap]
c. Respiratory rate
The respiratory rate (f for frequency) is the number of breaths the patient takes in 1 minute. The number is counted by looking at or feeling the chest or abdominal movements, or both. The normal rate varies with age (Table 1-2). It is assumed that the patient is resting but awake and has a normal temperature and metabolic rate. A respiratory rate above or below normal is cause for alarm.
TABLE 1-2 Normal Resting Respiratory Rates
| Age (Years) | Male | Female |
|---|---|---|
| 0 | 31 ± 8 | 30 ± 6 |
| 1-2 | 26 ± 4 | 27 ± 4 |
| 2-4 | 25 ± 4 | 25 ± 3 |
| 5-7 | 22 ± 2 | 21 ± 2 |
| 8-11 | 19 ± 2 | 19 ± 2 |
| 12-14 | 19 ± 2 | 18 ± 2 |
| 15-16 | 17 ± 3 | 18 ± 3 |
| 17-18 | 16 ± 3 | 17 ± 3 |
| Older | 16 ± 3 | 17 ± 3 |
Modified from Eubanks DH, Bone RC: Comprehensive respiratory care, ed 2, St Louis, 1990, Mosby.
d. Blood pressure
Hypertension in the adult is a systolic BP of 140 mm Hg or greater or a diastolic BP of 90 mm Hg or greater, or both. Carefully measure the BP of any patient with a history of hypertension, bounding pulse, or symptoms of a stroke (mental confusion, headache, and sudden weakness or partial paralysis). Fear, anxiety, and pain also cause the patient’s BP to increase temporarily.
e. Heart/pulse rate
The heart/pulse rate (HR) is the number of heartbeats per minute. It can be counted by listening to the heart tones with a stethoscope or by feeling any of the common sites where an artery is easy to locate. Table 1-3 shows the normal pulse rates based on age. It is assumed that the patient is alert but resting when the pulse is counted. Carefully measure the heart/pulse rate in any patient with cardiopulmonary disease or any of the aforementioned conditions for hypotension or hypertension.
TABLE 1-3 Normal Pulse Rates According to Age
| Age | Beats/min |
|---|---|
| Birth | 70–170 |
| Neonate | 120–140 |
| 1 year | 80–140 |
| 2 years | 80–130 |
| 3 years | 80–120 |
| 4 years | 70–115 |
| Adult | 60–100 |
From Eubanks DH, Bone RC: Comprehensive respiratory care, ed 2, St Louis, 1990, Mosby.
3. Serum electrolytes and other blood chemistries
a. Review the results of the patient’s serum electrolyte levels and other blood chemistries (Code: IA3) [Difficulty: ELE: R; WRE: Ap]
b. Recommend blood tests, such as the potassium level, to obtain additional data (WRE code: IC1) [Difficulty: WRE: R, Ap, An]
The serum (blood) electrolytes are measured in most patients when they are admitted to the hospital and as needed thereafter. This is to determine whether the values are within the normal ranges listed in Table 1-4. Any abnormality should be promptly corrected so that the patient’s nervous system, muscle function, and cellular processes can be optimized. Diet and a number of medications can affect the various electrolytes. Most abnormalities can be corrected by dietary adjustments or, if necessary, by oral or intravenous supplementation.
TABLE 1-4 Normal Serum Electrolyte and Glucose Levels
| NORMAL ELECTROLYTE VALUES* | |
| Chloride (Cl−) | 95–106 mEq/L |
| Potassium (K+) | 3.5–5.5 mEq/L |
| Sodium (Na+) | 135–145 mEq/L |
| Calcium (Ca++) | 4.5–5.5 mEq/L |
| Bicarbonate (HCO3−) | 22–25 mEq/L |
| NORMAL GLUCOSE VALUES* | |
| Serum or plasma | 70–110 mg/100 mL (dL) |
| Whole blood | 60–100 mg/100 mL (dL) |
* These values may vary somewhat among references.
1. Potassium (K+)
Potassium is the most important electrolyte to monitor because of its effect on general nerve function and cardiac function. Hyperkalemia is a high blood level of potas-sium. It causes the following electrocardiographic (ECG) changes: high, peaked T waves and depressed S-T segments; widening QRS complex; and bradycardia. Hypokalemia is a low blood level of potassium. It causes the following ECG changes: flat or inverted T waves, depression of the S-T segments, premature ventricular contractions (PVCs), and ventricular fibrillation (if severe enough). Chapter 11 offers a more complete discussion of ECG interpretation.
4. Bicarbonate (HCO3−)
Altered bicarbonate levels are commonly seen in patients with pulmonary conditions. The kidneys of patients with a chronically elevated arterial partial pressure of carbon dioxide (Paco2) typically retain bicarbonate to moderate the respiratory acidosis caused by the elevated carbon dioxide level. Conversely, the kidneys of patients with a chronically decreased Paco2 level excrete bicarbonate to moderate the respiratory alkalosis caused by the decreased Paco2 level.
6. Glucose
The blood glucose level is important to monitor, because it directly relates to how much glucose is available to the patient for energy for daily activities. The normal values are listed in Table 1-4. Hypoglycemia is a low blood level of glucose; it can mean that the patient is malnourished. Hyperglycemia is a high blood level of glucose; this may indicate that the patient has diabetes mellitus or Cushing’s disease or is being treated with corticosteroids. More specific testing must be done to prove the diagnosis.
4. Complete blood count
a. Review the results of the patient’s complete blood count (Code: IA3) [Difficulty: ELE: R; WRE: Ap]
b. Recommend a complete blood count for additional data. (Code: IC1) [Difficulty: WRE: R, Ap, An]
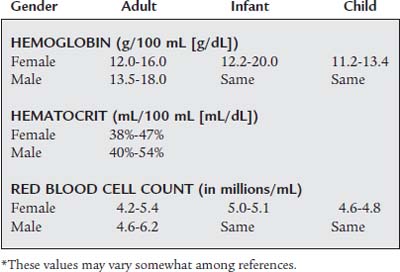
The key normal values for the RBC count are listed in Table 1-5. The hemoglobin and hematocrit values also are important, because they directly relate to the patient’s oxygen-carrying capacity. Decreased hemoglobin and hematocrit values indicate that the patient is anemic. An anemic patient has less oxygen-carrying capacity, and as a result, more stress is placed on the heart during exercise. Hypoxemia resulting from a cardiopulmonary abnormality places this patient at great risk. A transfusion is indicated if the hematocrit is below the level the physician considers clinically safe.
The key normal leukocyte count and differential are listed in Table 1-6. A normal leukocyte count and a normal differential reveal two things about the patient. First, no active bacterial infection is present. Second, the patient’s body is able to produce the normal number and variety of WBCs to combat an infection.
TABLE 1-6 White Blood Cell and Differential Counts*
| WHITE BLOOD CELL COUNT (mm3) | |
| Adult | 4,500-11,000 |
| Infant and child | 9,000-33,000 |
| DIFFERENTIAL COUNT | |
| Segmented neutrophil | 40% |
| Lymphocytes | 20% |
| Monocytes | 2% |
| Eosinophils | 0% |
| Bands | 0% |
| Basophils | 0% |
* These values may vary somewhat among references.
A mild to moderate increase in the leukocyte count is called leukocytosis. It is seen as a WBC count of 11,000 to 17,000 per cubic millimeter (mm3). Usually, the higher the count, the more severe the infection. A WBC count above 17,000/mm3 is seen in patients with severe sepsis, miliary tuberculosis, and other overwhelming infections. When a patient has an acute, severe bacterial infection, the WBC differential count shows an increased number of neutrophils. Exceptions to this are patients who are elderly, those who have acquired immunodeficiency syndrome (AIDS), and those with other immunodeficiencies. These patients may have an infection but show only a mildly elevated WBC count.
5. Review the patient’s coagulation study results (Code: IA3) [Difficulty: ELE: R; WRE: Ap]
Coagulation studies are routinely done for many hospitalized patients; for those who are to have surgery; and for those who have or are suspected of having a blood-clotting disorder. Also, many medications speed or slow clotting time (so-called blood thinners). It is important to review a patient’s coagulation studies before drawing a blood sample or performing a procedure that may lead to bleeding. Table 1-7 lists normal coagulation study results. If the patient’s clotting time is increased, the individual is at risk of bleeding. Be prepared to apply pressure to a blood sampling site (especially and arterial one) longer than expected.
TABLE 1-7 Normal Coagulation Study Results
| Test Name | Normal Value | Critical Value |
|---|---|---|
| Bleeding time | 1-9 min | >15 min |
| Prothrombin time (PT or Pro-time) | 11.0-12.5 sec; 85%-100% | >20 sec |
| Partial thromboplastin time (PTT) | 60-70 sec | >100 sec |
| Activated partial thromboplastin time (APTT) | 30-40 sec | >70 sec |
6. Gram stain results, culture results, and antibiotic sensitivity results
a. Review the patient’s Gram stain results, culture results, and antibiotic sensitivity results (Code: IA3) [Difficulty: ELE: R; WRE: Ap]
7. Review the patient’s urinalysis results
A urine sample routinely is taken from every patient admitted to the hospital and from pregnant women and presurgical patients. Much information about the functioning of the kidneys and other metabolic processes can be gathered from the urinalysis results. A urinalysis also is done for diagnostic purposes in patients with abdominal or back pain, hematuria, and chronic renal disease. Table 1-8 lists the normal findings for a urinalysis. Any abnormal findings should be further investigated to discover the cause.
TABLE 1-8 Normal Urinalysis Results
| Test Item | Normal Value |
|---|---|
| Appearance | Clear |
| Color | Amber yellow |
| pH | 4.6-8.0 (average 6.0) |
| Specific gravity | Adult: 1.005-1.030 (usually 1.010-1.025) |
| Newborn: 1.001-1.020 | |
| White blood cells | 0-4 |
| Red blood cells | 0-2 |
8. Review the patient’s pleural fluid study results
If a patient has had a thoracentesis procedure to remove pleural fluid, the fluid is sent to the laboratory for further analysis. The fluid may turn out to be watery, bloody, infected, or lymphatic. See Chapter 18 for a complete discussion of the types of pleural fluids.
MODULE B
2. Recommend radiographic and other imaging studies to obtain additional data (Code: IC2) [Difficulty: ELE: R, Ap; WRE: An]
a. Chest radiograph
A chest radiograph should be recommended in the following situations:
d. MRI scan
An MRI scan provides images of body organs without the use of radioactive materials. The images are created when the powerful magnet of the MRI machine is turned on and off, affecting the way hydrogen atoms align within the body. A limitation of MRI is that the patient cannot have any metallic implants. In addition, most mechanical ventilators cannot be used during an MRI scan because the magnetic field will interfere with the unit. Indications for an MRI scan include, but are not limited to, the following:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree