Pathway for the Management of Acute Heart Failure
Edgar Argulian
Eyal Herzog
Emad F. Aziz
Marrick L. Kukin
EPIDEMIOLOGY AND IMPACT
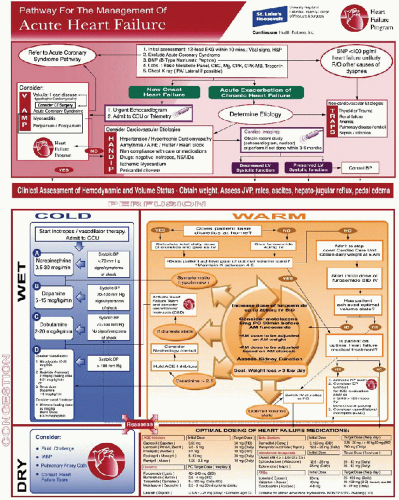
Heart failure is a common and growing problem in the United States with estimated prevalence of almost 6 million patients. Acute decompensated heart failure accounts for more than a million hospital admissions per year with numbers expected to rise owing to an aging population.1 The current chapter is intended to outline a simple, yet comprehensive approach to the diagnosis and management of acute decompensated heart failure by synthesizing the evidence from multiple studies and major cardiology society recommendations.2,3 It is based on the initial acute heart failure management pathway published by our heart failure team (Figure 9.1).4
DEFINITIONS
Acute decompensated heart failure refers to the acute onset of dyspnea owing to elevated cardiac filling pressures. It can be newly diagnosed heart failure or exacerbation of preexisting chronic heart failure condition. Despite major advances in laboratory and diagnostic modalities, heart failure remains a clinical diagnosis of a constellation of signs and symptoms. Careful history taking and focused physical examination are the cornerstones of the diagnosis. The diagnosis is established by the combination of symptoms of heart failure (such as dyspnea and orthopnea), signs of fluid overload (such as jugular venous distention, pulmonary crackles, and peripheral edema) and objective evidence of structural heart disease (such as third heart sounds, cardiac murmurs, and echocardiographic findings). Acute decompensated heart failure is a continuum of clinical presentations ranging from mild dyspnea to florid pulmonary edema to cardiogenic shock. Although initially described for patients with myocardial infarction, the Forrester classification can be applied to patients with acute decompensated heart failure to guide the management.5 It assigns patients to groups based on estimation of left-sided filling pressures (“wet” meaning pulmonary congestion and high pulmonary capillary wedge pressures) and perfusion state (“cold” meaning low perfusion state and low systemic blood pressure). Most patients with acute decompensated heart failure fall into the “wet” and “warm” category: They have evidence of pulmonary congestion/pulmonary edema with normal or high blood pressure. Patients with pulmonary edema and low systemic pressures are in cardiogenic shock, which typically signifies bad prognosis unless a reversible cause is rapidly identified and corrected (e.g., reperfusion therapy in a patient with acute myocardial infarction or a corrective surgery in a patient with acute valvular dysfunction). Sometimes patients with cardiogenic shock (“cold” state) have no evidence of pulmonary congestion and systemic hypoperfusion dominates the clinical picture. Patients with right ventricular infarction are a classic example in this category.
ETIOLOGY AND PREDISPOSING FACTORS
There is a long list of possible heart failure etiologies but in reality a few causes account for most of the cases. From longterm heart failure management perspective, the causes can be broadly divided into heart failure with low left ventricular ejection fraction (LVEF) and heart failure with preserved LVEF. Coronary artery disease is the most common cause of heart failure with low LVEF.6 Dilated cardiomyopathy that can be idiopathic or associated with other conditions (infections, toxins, peripartum, etc.) is a less common cause. The prevalence of heart failure with preserved LVEF increases with age and overall accounts for almost 50% of heart failure cases.7 Diastolic heart failure is the largest category within the heart failure with preserved LVEF, and hypertension is the most important etiologic factor. Some valvular diseases (such as aortic stenosis and mitral regurgitation), hypertrophic cardiomyopathy, and restrictive cardiomyopathy also present as heart failure with preserved LVEF.8
In any patient who presents with new-onset acute decompensated heart failure or chronic heart failure exacerbation, the precipitating cause should be identified and adequately addressed. Myocardial ischemia is a common precipitating factor and should be considered in the differential diagnosis. Valvular pathology can cause acute heart failure if it develops suddenly: typical examples include flail mitral valve with chordal rupture or aortic valve perforation in infectious endocarditis. Myocarditis and postpartum cardiomyopathy can present as acute heart failure. VAMP (Valvular disease, Acute coronary syndromes, Myocarditis, and Peripartum/Postpartum cardiomyopathy) is a useful mnemonic in evaluating a patient with new-onset acute heart failure (Figure 9.2).4 Severe hypertension is another common condition typically associated with preserved LVEF and better in-hospital outcomes. Both supraventricular and ventricular arrhythmias can precipitate heart failure. It is important to know that patients with diastolic dysfunction are highly dependent on preload for left ventricular filling. Certain arrhythmias such as atrial fibrillation decrease
diastolic filling by increasing heart rate and eliminating atrial kick, and therefore they can provoke florid heart failure in an otherwise stable patient. Interestingly, frequent ventricular premature beats and right ventricular pacing can create dyssynchrony contributing to heart failure.9 Medication along with diet noncompliance is one of the most common factors that precipitates acute exacerbation in patients with chronic heart failure. HANDIP (hypertension, arrhythmias, noncompliance with care, drugs, ischemic myocardium, and pericardial disease) is another useful mnemonic in evaluating patients with heart failure exacerbation from cardiac causes (Figure 9.2).4
diastolic filling by increasing heart rate and eliminating atrial kick, and therefore they can provoke florid heart failure in an otherwise stable patient. Interestingly, frequent ventricular premature beats and right ventricular pacing can create dyssynchrony contributing to heart failure.9 Medication along with diet noncompliance is one of the most common factors that precipitates acute exacerbation in patients with chronic heart failure. HANDIP (hypertension, arrhythmias, noncompliance with care, drugs, ischemic myocardium, and pericardial disease) is another useful mnemonic in evaluating patients with heart failure exacerbation from cardiac causes (Figure 9.2).4
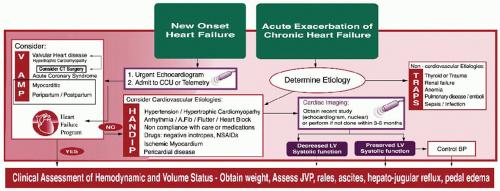 Figure 9.2. Differential diagnosis between new onset heart failure and acute exacerbation of chronic heart failure with timing of imaging and consideration of precipitating pathophysiology. |
Noncardiac factors can precipitate heart failure in otherwise stable patients by creating high oxygen demand and inducing tachycardia (such as anemia, thyroid diseases, drugs, fever and infection, and pulmonary emboli), causing fluid overload (inhospital IV fluid administration, renal failure, and nonsteroidal anti-inflammatory drugs or NSAIDs) or decreasing myocardial contractility (negative inotropes such as verapamil). TRAPS (thyroid, renal failure, anemia, pulmonary disease, and sepsis) is a mnemonic to help categorize noncardiac precipitants of heart failure exacerbation (Figure 9.2).4
DIAGNOSIS AND WORKUP
Once the history and physical examination findings consistent with heart failure are ascertained, further workup is directed towards confirming the diagnosis, establishing the cause of the heart failure, addressing the precipitating factor(s), and identifying prognostic indicators. Physical examination should specifically focus on the degree of respiratory failure (tachypnea, accessory respiratory muscle use), vital signs, and signs of fluid overload (pulmonary crackles, jugular venous distension, and peripheral edema). Cardiac assessment may provide important clues to the diagnosis (e.g., a new murmur). Bedside rapid assessment of left-sided filling pressures and systemic perfusion helps to assign the patient to one of the Forrester categories as described above. The essential set of initial tests includes EKG, laboratory workup (electrolytes, renal function and liver function test, and coagulation profile), cardiac enzymes and chest X-ray. It is important to remember that up to one-third of patients with Acute Coronary Syndrome (ACS) have no chest pain upon presentation.10 Therefore, serial EKGs and cardiac enzymes are an essential part of the initial workup. Of note, some repolarization abnormalities and QTc interval prolongation can be caused by acute heart failure per se, not necessarily myocardial ischemia.11 Similarly, small increase in cardiac biomarkers is often seen in acute decompensated heart failure.12 Other important findings on EKG include arrhythmias, conduction delays, and hypertrophy. Chest X-ray helps to assess the degree of fluid overload, and it can demonstrate some other relevant pathology (large pleural effusion, infiltrates, and cardiomegaly). Arterial blood gases provide information about oxygenation, ventilation, and acid-base status; arterial blood gases should be obtained in every patient with significant respiratory distress as well as low perfusion (“cold”) state.
B-type natriuretic peptides (BNP and proBNP) are released from myocardial cells in response to increase in the wall stress. Their levels are elevated in systolic as well as diastolic heart failure.13 Measuring BNP level can supplement the evaluation of patients with suspected acute decompensated heart failure if used in the appropriate clinical context. Low BNP levels (<100 pg per ml) have a high negative predictive value, which makes the diagnosis of heart failure unlikely in a patient who presents to the emergency department with dyspnea.14 Values >400 pg per ml are consistent with heart failure, whereas intermediate values (100 to 400 pg per ml) are in the gray zone.2 Studies showed linear correlation between the admission BNP levels in patients with acute decompensated heart failure and in-hospital mortality.15 Of note, obese patients with heart failure have lower BNP levels that should be factored in during clinical decision making. Sudden, “flash” pulmonary edema can sometimes be associated with falsely low BNP levels. At the same time, the positive predictive value of elevated BNP levels (especially gray zone values) is not very high as they can be elevated in patients with left ventricular hypertrophy, pulmonary hypertension, sepsis, renal dysfunction, and liver disease.16 For example, in a septic patient with possible heart failure elevated BNP levels add little information to clinical judgment. In patients with preexisting chronic heart failure who come
with acute exacerbation, one-time elevated BNP level conveys little information.
with acute exacerbation, one-time elevated BNP level conveys little information.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree