Pathway for the Management of Acute Coronary Syndrome
Eyal Herzog
Fahad Javed
Emad F. Aziz
Mun K. Hong
The practice of medicine is changing at unprecedented speed. Today’s reasonable assumption is outdated by tomorrow’s evidence. A deluge of data faces us as we deal with acute coronary syndrome (ACS). ACS subsumes a spectrum of clinical entities, ranging from unstable angina (UA) to ST-elevation myocardial infarction (STEMI; often referred to as “Q-wave myocardial infarction”). The management of ACS is deservedly scrutinized, as it accounts for 2 million hospitalizations and a remarkable 30% of all deaths in the Unites States each year. Clinical guidelines on the management of ACS, which are based on clinical trials, have been updated and published.1,2
This chapter will outline the current modalities available for the prompt diagnosis and optimal management of ACS patients. In this chapter, we describe a novel pathway for the management of ACS at our institution.3,4
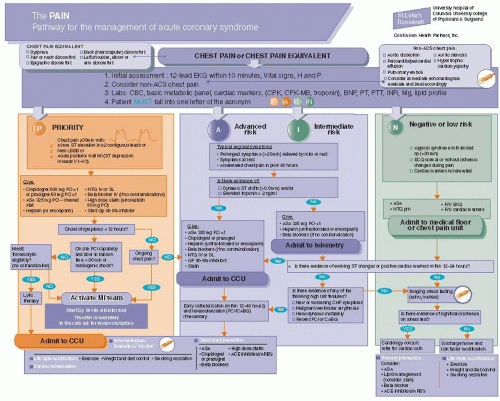
The pathway has been designated with the acronym of Priority risk, Advanced risk, Intermediate risk, and Negative/low risk (PAIN) that reflects patient’s most immediate risk stratification upon admission (Figure 1.1). This risk stratification reflects patient’s 30 days risks for death and MI following the initial ACS event.
The pathway is color-coded with “PAIN” acronym (P—red, A—yellow, I—yellow, and N—green) that guides patient
management according to patient’s risk stratification. These colors—similar to the road traffic light code—have been chosen as an easy reference for the provider about the sequential risk level of patients with ACS.5
management according to patient’s risk stratification. These colors—similar to the road traffic light code—have been chosen as an easy reference for the provider about the sequential risk level of patients with ACS.5
INITIAL ASSESSMENT OF PATIENTS WITH CHEST PAIN OR CHEST PAIN EQUIVALENT
Patients who present to emergency departments with chest pain or chest pain equivalent will be enrolled into this pathway.
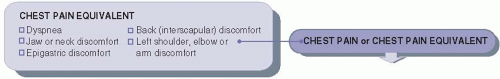
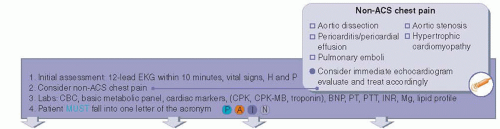
Figure 1.2 shows the chest pain equivalent symptoms. The initial assessment is seen in Figure 1.3. All patients should have an electrocardiogram (ECG or EKG, abbreviated from the German Elektrokardiogramm) performed within 10 minutes as well as detailed history and physical exam.
Non-ACS chest pain should be excluded urgently. Causes include aortic dissection, pericarditis and pericardial effusion, pulmonary emboli, aortic stenosis, and hypertrophic cardiomyopathy. If any of these emergency conditions is suspected, we recommend obtaining immediate echocardiogram or CT and to treat accordingly.
Our recommended initial laboratory tests include CBC, basic metabolic panel, cardiac markers (to include CPK, CPK-MB, and Troponin), BNP, PT, PTT, INR, magnesium, and a lipid profile.
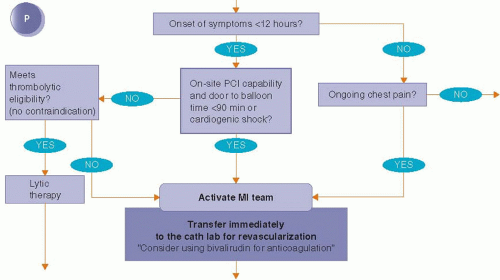
INITIAL MANAGEMENT OF PRIORITY PATIENTS
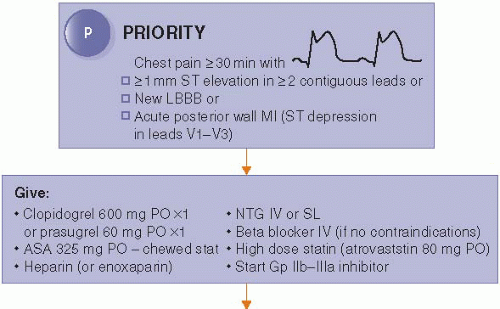
“PRIORITY” patients are those with symptoms of chest pain or chest pain equivalent lasting longer than 30 minutes with one of the following EKG criteria for acute MI:
≥1 mm ST elevation in two contiguous leads, or
New left bundle branch block (LBBB), or
Acute posterior wall MI (ST segment depression in leads V1-V3).
The initial treatment of these patients includes placing an intravenous line, providing oxygen, treating patients with oral aspirin (chewable 325 mg stat), clopidogrel (600 mg loading dose) or prasugrel (60 mg loading dose), intravenous β-blocker (if no contraindication), heparin (unfractionated or enoxaparin), nitroglycerin, oral high-dose statin, and to consider using intravenous glycoprotein IIb to IIIa inhibitors if it will not delay the transfer of the patient to the cardiac catheterization laboratory (Figure 1.4).
The key question for further management of these patients is the duration of the patients’ symptoms. For patients whose symptoms exceed 12 hours, presence of persistent or residual chest pain determines the next strategy. If there is no evidence of continued symptoms, these patients will be treated as if they had been risk stratified with the advanced risk group.
For patients whose symptoms are <12 hours or with ongoing chest pain, further management is based on the availability of on-site angioplasty (percutaneous coronary intervention or PCI) capability with expected door to balloon time of <90 minutes or the presence of cardiogenic shock. Patients with expected door to balloon time of <90 minutes should be transferred immediately to the cardiac catheterization lab for revascularization. The MI team is activated for this group of patients (Figure 1.5).
In our institution, a single call made by the emergency department physician to the page operator activates the MI team, which includes the following health care providers:
The interventional cardiologist on-call (who is considered the “team leader”).
The director of the CCU.
The cardiology fellow on-call.
The interventional cardiology fellow on-call.
The cath lab nurse on-call.
The cath lab technologist on-call.
The CCU nursing manager on-call.
The senior internal medicine resident on-call.
Activating this group has been extremely successful in our institution and has markedly reduced our door to balloon time. These strategies have been recently shown to decrease door to balloon time in the range of 8 to 19 minutes.6
For hospitals with no PCI capability or in situations when door to balloon time is expected to exceed 90 minutes, we recommend thrombolytic therapy if there are no contraindications.
CCU MANAGEMENT AND SECONDARY PREVENTION FOR PATIENTS WITH PRIORITY MI
Patients with “PRIORITY” MI should be admitted to the CCU (Figure 1.6). All patients should have an echocardiogram to evaluate left ventricle systolic and diastolic function and to exclude valvular abnormality and pericardial involvement. We recommend a minimum CCU stay of 24 hours to exclude arrhythmia complication or mechanical complication. For patients with no evidence of mechanical complications or
significant arrhythmia, secondary prevention drugs should be started, including aspirin, clopidogrel or prasugrel, high-dose statin, β-blocker, and ACE inhibitor or angiotensin receptor blocker (ARB).
significant arrhythmia, secondary prevention drugs should be started, including aspirin, clopidogrel or prasugrel, high-dose statin, β-blocker, and ACE inhibitor or angiotensin receptor blocker (ARB).
Most patients can be discharged within 48 hours with recommendations for life style modification including exercise, weight and diet control, smoking cessation, and cardiac rehabilitation. Secondary prevention drugs should be continued on discharge.
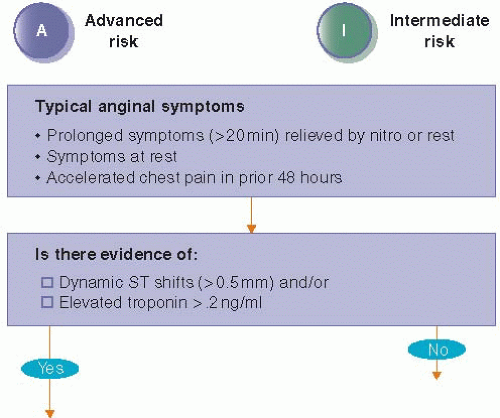
MANAGEMENT OF ADVANCED RISK ACS
Typical anginal symptoms must be present in patients, who will enroll in the advanced or the intermediate risk groups.
These symptoms include the following:
prolonged chest pain (>20 minutes) relieved by nitroglycerine or rest;
chest pain at rest; or
accelerated chest pain within 48 hours.
In order to qualify for the advanced risk group, patients must have either dynamic ST changes on the EKG (>0.5 mm) and/or elevated troponin (>0.2 ng per /ml) (Figure 1.7).
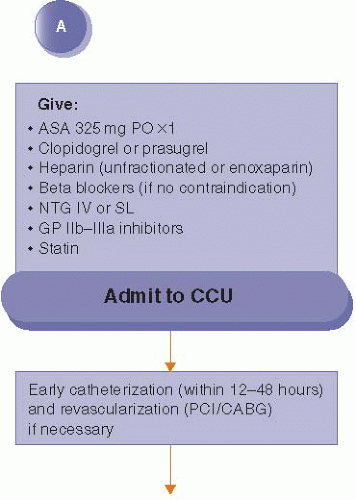
We recommend that patients be admitted to the CCU and be treated with aspirin, clopidogrel or prasugrel, heparin, glyoprotein IIb-IIIa inhibitor, β-blocker, statin, and nitroglycerin if there are no contraindications (Figure 1.8).
These patients should have early cardiac catheterization within 12 to 48 hours and revascularization by PCI or coronary artery bypass surgery (CABG) if necessary. All patients should have an echocardiogram to evaluate LV function. Recommendation for secondary prevention medication, life style modification, and cardiac rehabilitation should be provided similar to the patients with PRIORITY risk group (Figure 1.6).
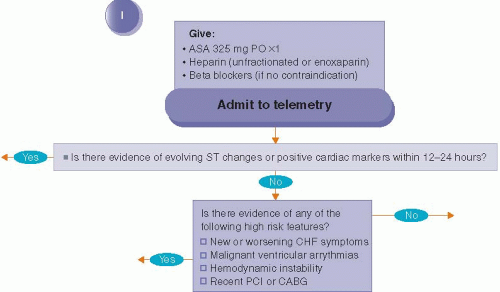
MANAGEMENT OF INTERMEDIATE RISK GROUP
Both intermediate risk group and advanced risk patients present to the hospital with typical anginal symptoms. Compared with the advanced risk patients, the immediate risk patients do not have evidence of dynamic ST changes on the EKG or
evidence of positive cardiac markers. These patients should be admitted to the telemetry floor and be given aspirin, heparin, and β-blocker if no contraindication (Figure 1.9). We recommend a minimum telemetry stay of 12 to 24 hours. If during this period of time there is evidence of dynamic ST changes on the EKG or evidence for positive cardiac markers, the patients should be treated as if they had been stratified to the advanced group.
evidence of positive cardiac markers. These patients should be admitted to the telemetry floor and be given aspirin, heparin, and β-blocker if no contraindication (Figure 1.9). We recommend a minimum telemetry stay of 12 to 24 hours. If during this period of time there is evidence of dynamic ST changes on the EKG or evidence for positive cardiac markers, the patients should be treated as if they had been stratified to the advanced group.
The intermediate risk group patients are assessed again for the following high risk features:
New or worsening heart failure symptoms;
Malignant ventricular arrhythmias;
Hemodynamic instability; or
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree