LEARNING OBJECTIVES
Learning Objectives
The student will be able to define and describe bronchogenic carcinoma, distinguishing its various subtypes.
The student will be able to define and describe bronchial carcinoid tumor, distinguishing typical from atypical subtypes.
The student will be able to identify the most common benign lung tumor, the most common malignant lung tumor, and the most common primary neoplasm in cancer-related death in the United States.
Although some use the term “tumor” as a synonym of neoplasm, its core meaning is swelling or mass. Using this broader definition of “tumor,” lung tumors include non-neoplastic masses, as well as benign and malignant neoplasms.
The most common benign lung tumor is a pulmonary hamartoma, typically a popcorn-shaped mass of cartilage, fat, fibrous tissue, and blood vessels (Fig. 31.1). A hamartoma is a non-neoplastic mass of tissue in a normal anatomic location but with abnormal architecture. Despite its name, cytogenetic evidence suggests that the pulmonary hamartoma is neoplastic. Benign neoplasms of the lung include fibroma (a proliferation of spindle cells resembling mature fibroblasts), leiomyoma (a proliferation of spindle cells resembling mature smooth muscle cells), hemangioma (a proliferation of mature endothelial cells forming blood vessels of variable size), chondroma (a proliferation of cells resembling mature chondrocytes admixed with chondroid extracellular matrix), and inflammatory pseudo-tumor (a myofibroblastic proliferation).
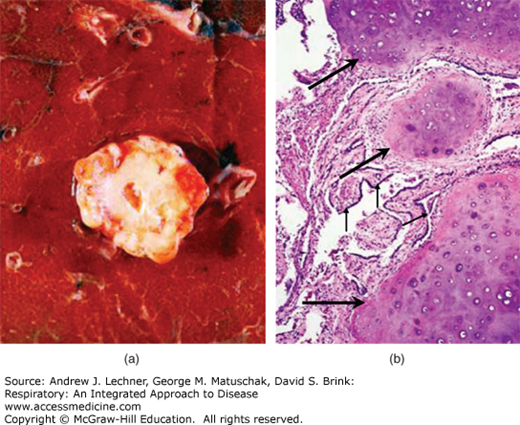
FIGURE 31.1
Pulmonary hamartoma. (a) Grossly, pulmonary hamartoma consists of a well-circumscribed lobulated mass with a shiny cut surface. (b) Histologically, the hamartoma shows islands of cartilage (large arrows) associated with bronchial epithelium (small arrows). From Rosai and Ackerman’s Surgical Pathology, 9th ed., Mosby-Elsevier, 2004.
The most common malignant neoplasm in the lung is a metastasis. Among primary malignant neoplasms of the lung, 90%-95% of these are derived from bronchial epithelium and are collectively referred to as bronchogenic carcinoma; the remaining 5%-10% of primary malignant pulmonary neoplasms comprise a heterogeneous group of cancers. Unless otherwise specified, the term “lung cancer” typically refers to bronchogenic carcinoma rather than metastasis or non-bronchogenic malignancies.
BRONCHOGENIC CARCINOMA
Excluding non-melanoma skin cancers (squamous cell carcinoma of the skin and basal cell carcinoma of the skin), bronchogenic carcinoma represents the second most common cancer in the United States (see Fig. 32.1) and the most common cause of cancer-related death in men and women. The development of bronchogenic carcinoma is a multistep process in which numerous specific mutations accumulate in a temporal sequence. Common oncogenes involved in the pathogenesis of bronchogenic carcinomata include c-MYC, k-RAS, EGFR, c-MET, and c-KIT. Tumor suppressor genes that are commonly deleted or inactivated in the pathogenesis of bronchogenic carcinoma include p53, RB, p16, and unknown genes on the short arm of chromosome 3. Risk factors for the development of bronchogenic carcinoma are discussed in Chap. 32 and include tobacco smoking. Of note, tobacco smoking also increases the risk of the development of cancer of the lip, tongue, floor of the mouth, pharynx, larynx, esophagus, urinary bladder, pancreas, and kidney.
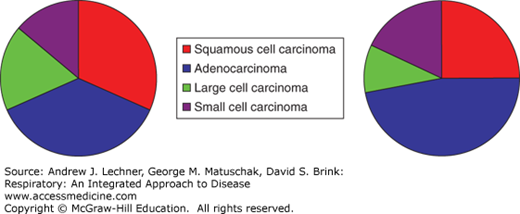
Bronchogenic carcinoma is further subclassified by microscopic morphologic criteria. Broadly speaking, there are four major types of bronchogenic carcinoma, and each can be further subtyped. All types are associated with cigarette smoking and are aggressive, locally invasive, and frequently are already widely metastatic at the time of diagnosis. Furthermore, all types are associated with paraneoplastic syndromes (Chap. 32). The four major types of bronchogenic carcinoma are squamous cell carcinoma (SCCA), adenocarcinoma, large cell carcinoma, and small cell carcinoma (Fig. 31.2).
Squamous cell carcinoma is more common in men and generally is a central disease (Fig. 31.3), often with central necrosis, cavitation, and hilar lymph node involvement. However, the incidence of SCCA in more peripheral lung locations is increasing. Microscopically, SCCA is characterized by production of keratin and/or by the presence of intercellular bridges between malignant epithelial cells. In well-differentiated SCCAs, keratin and/or intercellular bridges may be easily identified; in more poorly differentiated SCCA, mitotic activity is typically increased, and keratin and intercellular bridges are more difficult to identify. Variants of SCCA include papillary, clear cell, small cell (not to be confused with small cell carcinoma, see below), and basaloid. Common genes implicated in the pathogenesis of SCCA include p53, RB, p16, and many others.
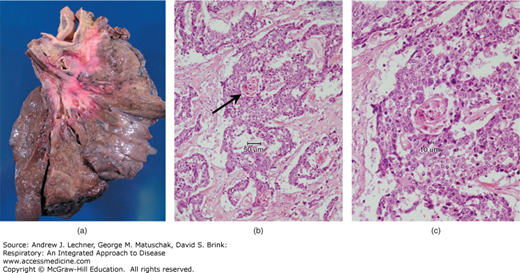
FIGURE 31.3
Squamous cell carcinoma (SCCA) is typically located near the hilum, as in this example (a). (b) Histologically, the malignant cells of SCCA have intercellular bridges between cells (not identifiable at this magnification). In this well-differentiated SCCA, keratin production is present; the arrow indicates a keratin pearl, which is seen at higher magnification in (c). (a): From Kemp et al. Pathology: the Big Picture, McGraw-Hill; 2008.
Adenocarcinoma is more common in women and generally is a peripheral lung disease (Fig. 31.4). It is the most common primary lung cancer in nonsmokers, and the most common type of bronchogenic carcinoma in men and women (previously, SCCA was most common in men). Microscopically, adenocarcinoma shows mucin production and/or gland formation, features that are more easily recognized in well differentiated tumors than in poorly differentiated tumors. Variants of adenocarcinoma include acinar, papillary, bronchioloalveolar, and solid. Of the subtypes, bronchioloalveolar carcinoma stands out as distinct not only grossly and microscopically but also clinically and is further discussed below. Common genes implicated in the development of adenocarcinoma include k-RAS, p53, RB, p16, EGFR, and c-MET.
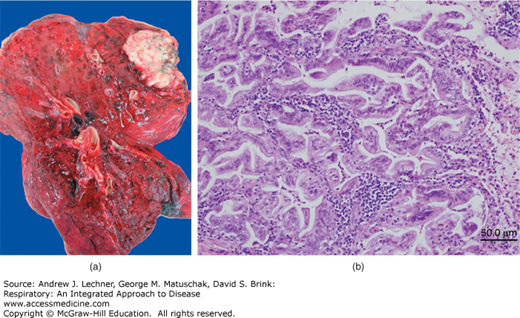
FIGURE 31.4
Adenocarcinoma is typically located in the lung periphery, far removed from the hilum, as in the example (a). (b) This example of adenocarcinoma shows a well-differentiated neoplasm, with easily recognizable glands. In the setting of a more poorly differentiated neoplasm, special stains and/or immunohistochemical analysis may be necessary to demonstrate glandular differentiation. (a): From Kemp et al. Pathology: the Big Picture, McGraw-Hill; 2008.
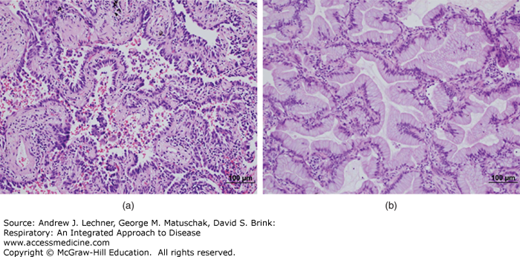
Bronchioloalveolar adenocarcinoma is typically a peripheral, multinodular lesion that grows along the preexisting framework of acini without destruction of its architecture. This growth pattern is called lepidic, a somewhat colorful term likening the growth of neoplastic cells to butterflies sitting atop a fence (Fig. 31.5). The bronchioloalveolar subtype of adenocarcinoma, in contrast to other adenocarcinoma subtypes, shows no significant association with smoking. Bronchioloalveolar carcinoma is further subclassified into mucinous and nonmucinous subtypes, with the latter more likely to show aerogenous spread and, hence, be multinodular (Fig. 31.6).