Palliative Laser Stent Treatment
Presentation
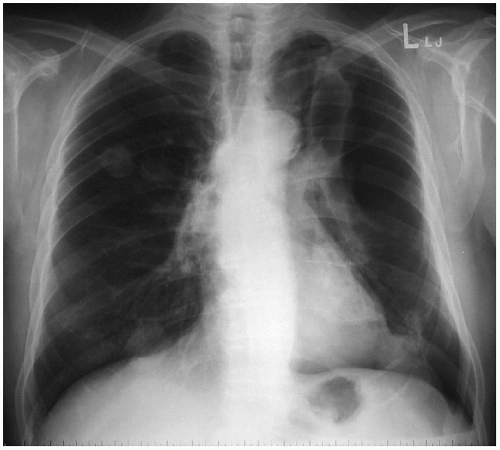
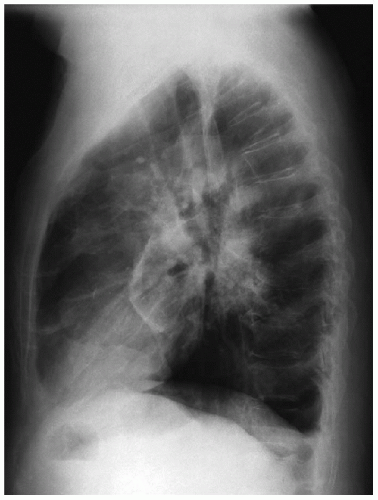
A 65-year-old man presents to the emergency department in moderate distress. The patient reports dyspnea on exertion and blood-streaked sputum for past 4 months. He now presents with an acute exacerbation, which began several hours before the emergency department admission. The patient was diagnosed with advanced non-small cell lung cancer 8 months ago, for which he received two cycles of chemotherapy. On physical examination, vital signs are stable, but room air saturations are 78%. On auscultation, there are decreased breath sounds over the left chest. The trachea is midline. The patient is treated initially with 100% oxygen, and full panel laboratory tests, an electrocardiogram, and the following chest x-rays are obtained.
Case Continued
A left-sided tube thoracostomy is placed in the emergency department with marked clinical improvement; however, repeat chest x-ray demonstrates a partially expanded left lung. The patient is admitted to the hospital, and the tube thoracostomy is placed on suction. Chest x-ray on the second hospital day shows nonexpansion of the lung and no air leak.
Recommendation
Failure of the lung to expand may be from either a large bronchopleural fistula with persistent air leak or airway obstruction by tumor, leading to atelectasis of a lobe or segment of the left lung. Computed tomography (CT) scans and bronchoscopy are necessary for further diagnosis and treatment planning.
▪ CT Scans
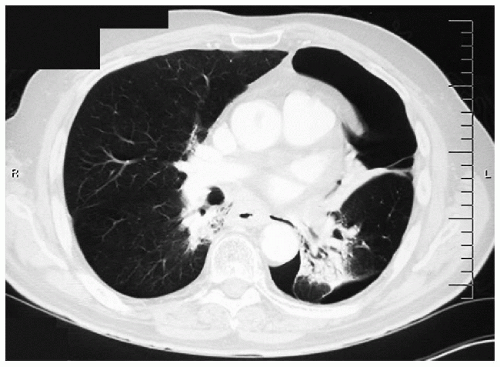 Figure 35-3
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|