Patients admitted to today’s cardiac intensive care units (CICUs) have increasingly complex medical conditions; consequently, palliative care is becoming an integral component of their care. Although there is a robust body of literature emanating from other intensive care unit settings, there has been less discussion about the role of palliative care in the CICU. This study examined all admissions to the Mount Sinai Hospital CICU from January 1 through December 31, 2012. Of the 1,368 patients admitted, there were 117 CICU patient deaths. End-of-life discussions were carried out in 85 patients (72.6%) who died during that hospital admission; the primary CICU team led these discussions and helped with decision making in >1/2 of them. For the 85 patients who had goals of care (GOC) discussions, there was a higher rate of redirected GOC toward comfort care or no escalation of care (38.8% vs 3.1%, p <0.001) and withdrawal of life-sustaining treatments, such as mechanical ventilation and vasopressors (23.5% vs 6.3%, p = 0.02) compared with patients for whom no GOC discussions were held. Among patients who had GOC discussions, there was no statistically significant difference for patients who had their mechanical circulatory support, defibrillator, or pacing therapies turned off compared with patients who were not involved in GOC discussions. With the exception of discontinuation of mechanical circulatory support which took place for 6 of the 7 patients in the CICU, end-of-life interventions were split evenly between the palliative care unit and the CICU. There was no difference in CICU length of stay or days to mortality from the time of CICU admission between the 2 groups. In conclusion, our study demonstrates the effect of palliative care and end-of-life decision making in the CICU. As such, we advocate for increased palliative care education and training among clinicians who are involved in cardiac critical care.
With the development of advanced therapies, the coronary care unit has evolved over the last 5 decades to one now delivering complex critical care for cardiac patients, and oftentimes palliative care; as such, the unit is now more appropriately referred to as the cardiac intensive care unit (CICU). Mount Sinai Hospital (MSH) is a large, academic, 1,170-bed tertiary care hospital in Manhattan, New York. The CICU is a 14-bed unit that routinely manages cardiac patients with complex arrhythmias, advanced heart failure (HF), mechanical circulatory support (MCS), and post–cardiac transplantation care. Its team consists of an attending cardiologist, an attending intensivist, a cardiology fellow, a house staff team, and specialized nurses. MSH is also home to an inpatient palliative care unit (PCU) and a multidisciplinary palliative care service that provides palliative care consultative services. The purpose of this study was to determine the effect of palliative care interventions in a typical tertiary CICU on outcomes such as length of stay (LOS), inpatient mortality, and redirection of goals of care (GOC) toward comfort measures or withdrawal of life-sustaining treatments (LSTs) such as mechanical ventilation or hemodynamic support.
Methods
A total of 1,368 patients admitted to the MSH CICU from January 1 through December 31, 2012, were screened by the electronic medical record (EMR). The study was approved by Mount Sinai’s Institutional Review Board. In an effort to identify patients who were most likely to have received a palliative care intervention, patients who died during the hospital stay (whether in the CICU, the PCU, or another inpatient unit) were selected for further review. One hundred seventeen patients admitted to the CICU died during their hospitalization.
Patient information such as imaging and laboratory data for baseline characteristics, diagnoses pertaining to acute management, and GOC discussions were acquired by review of chart notes and the EMR. Respiratory failure was defined as the utilization of invasive positive pressure ventilation; cardiac failure as the use of inotropic support; severe sepsis as the development of hypotension requiring resuscitation with fluids or vasopressors in the setting of a documented or suspected infection requiring antibiotic treatment for >48 hours; acute kidney injury as an abrupt and persistent decrease in renal function, often requiring consultation by a nephrologist; neurologic complications as a cerebrovascular accident or transient ischemic attack either confirmed with neurologic imaging or confirmed by a consulting neurologist.
A GOC discussion was defined as a structured discussion with the patient and/or family regarding the patient’s end-of-life care that was documented as such in the patient chart. Specifically, GOC discussions that were held in our CICU were consistent with previously defined criteria and addressed at least one of the following: the lack of hope for cure, prolongation of life, quality of life, comfort, life goals, and family/caregiver support. This conversation could be initiated by either the primary CICU team or the palliative care consult team. Patients who had GOC discussions were then compared with those who did not with regards to LOS, discontinuation of MCS, discontinuation of implantable cardioverter-defibrillator/pacing therapies, redirected GOC (whether no escalation of care, comfort measures, withdrawal of LST, or palliative extubation), transfer to the PCU, and days from admission to death.
Patients who received GOC discussions were also compared on the basis of baseline characteristics and diagnoses. Whereas differences between categorical variables were calculated according to the chi-square and Fisher’s exact tests, differences between continuous variables were tested using the Wilcoxon rank sum test. p Values were used, with a 2-sided value of <0.05 considered significant. Analyses were performed using SAS 9.3 (SAS Institute, Cary, North Carolina).
Results
Of the 117 patients who did not survive their hospitalization, 69 died in the CICU; 85 patients and/or surrogates had GOC discussions. The CICU team had these discussions with 48 patients/surrogates, whereas 37 patients/surrogates received a formal palliative care consultation. Thirty-two patients died without any end-of-life care discussions ( Figure 1 ).
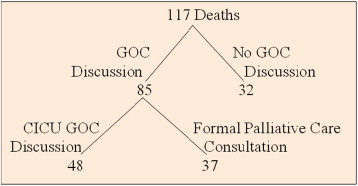
Table 1 illustrates baseline characteristics of the study population. The median age of the overall cohort was 71.5 years, and 56% were men. There was no significant difference between patients with GOC and no GOC discussion for age or gender, and there was no statistical difference in baseline laboratory values among patients who underwent GOC discussions compared with those who did not receive this intervention.
| Baseline Characteristics | ||||
|---|---|---|---|---|
| Variables | GOC Discussion | No GOC Discussion | Overall | P-Value |
| Overall Deaths | 85 | 32 | 117 | |
| Age (years) (median,IQR) | 71 (61 to 86) | 73 (62 to 79) | 71.5 (61 to 84) | 0.46 |
| Male | 47 (55.3%) | 18 (58.1%) | 65 (56.0%) | |
| Female | 38 (44.7%) | 13 (41.9%) | 51 (44%) | |
| Blood urea nitrogen (mg/dL) (median, IQR) | 37 (24 to 60) | 50 (31 to 61) | 39 (25 to 60) | 0.35 |
| Serum creatinine (mg/dL) (median, IQR) | 1.75 (1.11 to 2.71) | 2.14 (1.2 to 3.64) | 1.81 (1.13 to 3.03) | 0.15 |
| Hemoglobin (g/dL) (median, IQR) | 10 (8.8 to 11.7) | 10.4 (9.1 to 12) | 10.2 (8.85 to 11.7) | 0.30 |
Table 2 compares GOC with no GOC discussions for patients with specific diagnoses pertaining to end-organ failure. Sixty-seven patients were treated for HF, 26 for sepsis, 22 for respiratory failure, 6 for acute kidney injury, and 4 for transient ischemic attack or stroke. There was no significant difference among patients who received GOC discussions with respect to any of the single aforementioned diagnoses, although there was a trend toward GOC discussions for those patients with respiratory failure (p = 0.06) or sepsis (p = 0.06). Of note, 17 of the 67 patients with HF had at least 1 of the other 4 noncardiac diagnoses, and all but 1 of these patients had GOC discussions (p = 0.04).
| Diagnosis | GOC | No GOC | Overall | P-Value |
|---|---|---|---|---|
| Respiratory failure | 19 (22.4%) | 3 (9.4%) | 22 (18.8%) | 0.06 |
| Heart failure | 45 (52.9%) | 22 (68.8%) | 67 (57.3%) | 0.13 |
| Sepsis | 22 (25.9%) | 4 (12.5%) | 26 (22.2%) | 0.06 |
| Acute kidney injury | 4 (4.7%) | 2 (6.3%) | 6 (5.1%) | 0.32 |
| TIA or stroke | 3 (3.5%) | 1 (3.1%) | 4 (3.4%) | 0.43 |
| Heart failure + at least one of the above | 16 (18.8%) | 1 (3.1%) | 17 (14.5%) | 0.04 |
Subjects involved in GOC discussions had a statistically significant higher rate of redirected GOC toward comfort measures or no escalation of care (38.8% vs 3.1%, p <0.001), withdrawal of LST vasopressors (23.5% vs 6.3%, p = 0.02), and palliative extubation (21.2% vs 3.1%, p = 0.01) compared with patients for whom no GOC discussions were held ( Table 3 and Figure 2 ). Among patients who had GOC discussions, there was no statistically significant difference for patients who had their MCS or implantable cardioverter-defibrillator/pacing therapies turned off compared with those patients who were not involved in GOC discussions. Despite the greater degree of redirected end-of-life care among patients who received GOC discussions, there was no difference in CICU LOS or days to mortality from the time of CICU admission between the 2 groups, and our results still did not reach statistical significance when mean values were used instead of median values ( Table 4 ).



