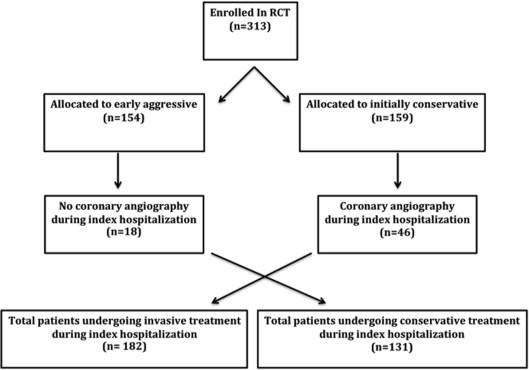
The Italian Elderly ACS study was the first randomized controlled trial comparing an early aggressive with an initially conservative strategy in patients with non–ST-segment elevation acute coronary syndromes aged ≥75 years, with the results showing no significant benefit of early aggressive therapy. The aim of this study was to evaluate the outcomes of trial patients, according to the treatment actually received during hospitalization. The trial enrolled 313 patients. The primary end point was the composite of death, myocardial infarction (MI), disabling stroke, and repeat hospital stay for cardiovascular causes or bleeding within 1 year. All patients in whom coronary angiography was performed during initial hospitalization were defined as having undergone invasive treatment (182 patients), whereas all patients who did not undergo coronary angiography were classified as medically managed (conservative treatment [CT] group, 131 patients). The primary end point occurred in 53 patients (40.5%) in the CT group and 45 patients (24.7%) in the invasive treatment group (hazard ratio 0.56, 95% confidence interval 0.37 to 0.83, p = 0.003). The invasive treatment group showed significantly lower rates of MI (6% vs 13% in the CT group; hazard ratio 0.43, 95% confidence interval 0.20 to 0.92, p = 0.034) and the aggregate of death and MI (14.3% vs 27.5% CT group; hazard ratio 0.48, 95% confidence interval 0.29 to 0.81, p = 0.004). In conclusion, elderly patients with non–ST-segment elevation acute coronary syndromes treated invasively experienced significantly better survival free from the composite of all-cause mortality, nonfatal MI, disabling stroke, and repeat hospitalization for cardiovascular causes or bleeding.
Elderly patients constitute an increasing proportion of those presenting with acute coronary syndromes (ACS), and older age is a major risk factor for adverse outcomes in non–ST-segment elevation ACS (NSTEACS). Although several randomized trials have evaluated the effect on outcomes of an early aggressive strategy in comparison with a more selective invasive approach in patients with NSTEACS, uncertainty remains regarding the benefits of this strategy on short- and long-term outcomes, particularly in elderly patients, who have usually been underrepresented in clinical trials of ACS. The Italian Elderly ACS trial was the first randomized study investigating treatment strategies for elderly patients with NSTEACS. The results of the randomized trial showed no significant benefit of an early aggressive approach in the whole population in reducing the primary end point of death, myocardial infarction (MI), stroke, and rehospitalization within 1 year. However, the results of the trial could have been affected by the fact that 46 patients (25%) in the conservative-strategy arm underwent coronary angiography during the index hospitalization, followed by revascularization in 36 patients. Indeed, data from a recent meta-analysis, conducted in 7 randomized trials enrolling a very large series of NSTEACS patients, suggest that revascularization itself, rather than the timeliness of invasive therapy, may be the key determinant in improving late clinical outcomes. Therefore, we performed an “as-treated” subanalysis of the Italian Elderly ACS trial comparing the outcomes of patients who actually underwent coronary angiography during index hospitalization with those of patients who were treated only medically, irrespective of randomized assignment in the trial.
Methods
The Italian Elderly ACS randomized trial enrolled patients aged ≥75 years with NSTEACS who were admitted within 48 hours of the most recent ischemic symptoms and showed ischemic electrocardiographic changes, elevated cardiac markers, or both. The study design has been published previously. Patients enrolled in the trial were randomly assigned to either (1) an early aggressive strategy of coronary angiography within 72 hours and, when indicated, coronary revascularization by either percutaneous coronary intervention or coronary artery bypass grafting, or (2) an initially conservative strategy, consisting of medical therapy and coronary angiography during the index hospital stay allowed in the case of refractory ischemia, myocardial reinfarction, heart failure of ischemic origin, or malignant ventricular arrhythmias. After discharge, follow-up visits were planned up to 405 days. In the present analysis we assessed the outcomes of the study population according to the invasive or medical treatment actually received during index hospitalization. To that end, we defined as having undergone “invasive treatment” (IT) all patients in whom coronary angiography, followed by revascularization when suitable, was performed during initial hospitalization; in contrast, all patients who did not undergo coronary angiography were classified as “medically managed.” The primary end point was the composite of all-cause mortality, nonfatal MI, disabling stroke, and repeat hospital stay for cardiovascular causes or severe bleeding within 12 months. Other outcomes of interest were death, MI, the composite of death and MI, and bleedings. The study definitions have been previously described in detail. Absolute and percentage frequencies are used to describe categorical variables and means and SDs to describe continuous variables. Categorical variables were compared using the χ 2 test and continuous variables using Student’s t test. Estimations of the cumulative primary event rates were done using the Kaplan-Meier method, and events time were compared using the log-rank test. The Cox proportional-hazards model was used to estimate the treatment effect as unadjusted hazard ratios with 95% confidence intervals. Two-sided p values <0.05 were considered significant. Analysis were performed using SPSS version 20 (SPSS, Inc., Chicago, Illinois).
Results
A total of 313 patients were enrolled in the randomized trial, 154 in the early aggressive arm and 159 in the initially conservative arm. As reported in Figure 1 , during the index hospitalization, a total 182 patients (58% of the whole population) underwent coronary angiography, 136 patients initially randomized to the early aggressive arm and 46 patients randomized to the initially conservative arm. These patients constituted the IT cohort. The conservative treatment (CT) cohort comprised 131 patients who did not undergo coronary angiography during the index hospitalization. The baseline characteristics of the patients are listed in the Table 1 . No differences were noted between the 2 groups regarding the common risk factors for cardiovascular disease except for older age and lower hemoglobin levels in the CT compared with IT group. Moreover, no difference between groups was noted in terms of prognostic risk as indicate by a similar Thrombolysis In Myocardial Infarction (TIMI) risk score and left ventricular ejection fraction. As previously reported, the reasons for not performing coronary angiography among patients in the early aggressive randomized arm were heart failure in 6 patients, withdrawn consent in 5, bleeding in 2, sepsis in 2, and death, transient ischemic attack, and acute renal insufficiency in 1 case each, whereas the indications for catheterization in patients initially randomized in the conservative cohort of the RCT were recurrent ischemia in 37 cases, heart failure in 6, reinfarction in 1, and sustained ventricular tachycardia in 2. The revascularization procedures performed in the IT group were percutaneous coronary intervention in 111 patients (61%) and coronary artery bypass grafting in 10 patients (5.5%). As expected, the use of glycoprotein IIb/IIIa inhibitors was higher in the IT group, whereas no differences were noted regarding the use of other antithrombotic drugs during the index hospitalization ( Table 2 ). Pharmacologic treatments at discharge were similar between groups except for higher use of nitrates and diuretics in the CT group. Length of hospital stay and the rate of adverse events occurred during hospitalization ( Table 3 ) were similar in the 2 groups. Of note, IT was not associated with an increased rate of death or procedure-related MI during the index admission compared with CT. The primary end point occurred in 53 patients in the CT group and 45 patients in the IT group (hazard ratio [HR] 0.56; 95% confidence interval [CI] 0.37 to 0.83, p = 0.003; Table 4 ). The incidence of nonfatal MI was significantly lower in the IT group (HR 0.43, 95% CI 0.20 to 0.92, p = 0.034). The combined end point of death and MI was significantly lower in the IT group compared with the CT group (HR 0.48, 95% CI 0.29 to 0.81, p = 0.004). No differences were observed for the other primary end point components except for the rate of bleeding that occurred in 3 patients in the CT group compared with none in the IT group (p = 0.040). The Kaplan-Meier curves for the primary end point and the combined end point of death and MI confirmed the better event-free survival for the invasively treated patients ( Figure 2 ). At Cox regression analysis, the IT performed during index hospitalization was the most important predictor of event-free survival (HR 0.55, 95% CI 0.37 to 0.82, p = 0.004) and was confirmed after correction for univariate differences between groups (HR 0.59, 95% CI 0.39 to 0.88, p = 0.010). We performed an additional analysis evaluating the outcomes of patients initially allocated to the IT or CT group according to the treatment effectively received during index hospitalization. The results of this analysis (249 patients: 136 in the IT group and 113 in the CT group) confirmed our previous observations. Indeed, the primary end point (24.3% in the IT group vs 38.1% in the CT group, p = 0.019) and the combined end point of death and MI (14% vs 24.8%, p = 0.030) were significantly lower in the IT group compared with the CT group. Finally, we evaluated the prognosis of the IT cohort of patients who did not undergo coronary angiography with that of patients in the CT group, both overall ( Supplementary Table 1 ) and divided according to treatment received during initial hospital stay ( Supplementary Table 2 ). No differences were noted in the 2 analyses with regard to the primary outcome or the other primary end point components.
| Variable | IT (n=182) | CT (n=131) | p value |
|---|---|---|---|
| Age (years) | 80.57 ± 4.21 | 82.32 ± 4.83 | 0.001 |
| Men | 96 (52.7%) | 61 (46.6%) | 0.281 |
| Hypertension | 152 (83.5%) | 107(81.7%) | 0.671 |
| Hypercholesterolemia | 82 (45.1%) | 55 (42%) | 0.589 |
| Diabetes Mellitus | 70 (38.5%) | 44 (33.6%) | 0.377 |
| Mean eGFR (mL/min/1.73m 2 ) | 53.60 ± 19 | 50.79 ± 18.2 | 0.194 |
| Prior Myocardial Infarction | 54 (29.7%) | 43 (32.8%) | 0.552 |
| Prior Percutaneous Coronary Intervention | 25 (13.7%) | 22 (16.8%) | 0.455 |
| Prior Coronary Bypass | 19 (10.4%) | 10 (7.6%) | 0.398 |
| Serum Hemoglobin (g/dL) | 13.38 ± 1.72 | 12.86 ± 1.68 | 0.008 |
| Ejection Fraction | 49.22 ± 9.55 | 47.81 ± 10.92 | 0.240 |
| TIMI risk score | 4.08 ± 1.38 | 4.21 ± 1.38 | 0.403 |
| Length of hospital stay | 8.41 ± 6.02 | 7.86 ± 5.94 | 0.424 |
| Variable | IT (n=182) | CT (n=131) | p value |
|---|---|---|---|
| During hospital stay | |||
| Aspirin | 176 (96.7%) | 124 (94.7%) | 0.371 |
| Thienopiridines | 171 (94%) | 118 (90.1%) | 0.203 |
| GP IIb/IIIa Inhibitors | 31 (17%) | 4 (3.1%) | 0.0001 |
| Unfractionated heparin | 47 (25.8%) | 29 (22.1%) | 0.453 |
| Low molecular weight heparin | 113 (62.1%) | 74 (56.5%) | 0.319 |
| Bivalirudin | 8 (4.4%) | 0 | 0.0001 |
| At follow up | |||
| Aspirin | 164 (90.1%) | 120 (91.6%) | 0.653 |
| Thienopiridines | 142 (78%) | 102 (77.9%) | 0.973 |
| Beta Blocker | 104 (57.1%) | 81 (61.8%) | 0.405 |
| Ace-inhibitor | 140 (76.9%) | 112 (85.5%) | 0.059 |
| Statin | 147 (80.8%) | 104 (79.4%) | 0.763 |
| Nitrates | 95 (52.2%) | 86 (65.6%) | 0.047 |
| Diuretics | 83 (45.6%) | 80 (61.1%) | 0.021 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


