Outcome data regarding postoperative acute coronary syndrome treated with percutaneous coronary intervention (PCI) are limited. The objective of this study was to determine clinical outcomes of patients undergoing PCI within 7 days after a surgical procedure. We assessed outcomes of 517 patients who underwent PCI within 7 days after a surgery across 44 hospitals from January 2010 to December 2011 from the Blue Cross Blue Shield of Michigan Cardiovascular Consortium registry. Patients with postoperative PCI were compared with all other patients with PCI using propensity-matched analysis. Of the 65,175 patients who underwent PCI within the study period, 517 patients had undergone surgery within the previous 7 days. In unadjusted analysis, patients with postsurgical PCI had higher in-hospital mortality (6.96% vs 1.33%), stroke (0.96% vs 0.26%), bleeding events (6.96% vs 2.6%), heart failure (6.96% vs 2.36%), and cardiogenic shock (7.16% vs 1.95%). After propensity matching, mortality remained higher in postsurgical patients (6.5% vs 3.96%, odds ratio 1.7 [1.1 to 2.6], p = 0.02). The odds of mortality were especially high among patients who would otherwise be considered low risk (<1% of predicted mortality in a nonsurgical setting) in whom a recent surgery was strongly associated with death (odds ratio 5.7, p = 0.02). In conclusion, PCI performed within 7 days after a surgical procedure is associated with an increased risk of early mortality. Although some of this increased risk is related to an adverse clinical profile, higher mortality is also observed in patients otherwise considered low risk for PCI.
There is paucity of contemporary data on the outcome of percutaneous coronary intervention (PCI) performed among patients who have had a recent surgery. We accordingly used data from a large contemporary cohort of patients undergoing PCI in the state of Michigan to assess the prevalence and outcome of patients undergoing PCI after a recent surgery.
Methods
The study sample included 65,175 consecutive PCI procedures in a large multicenter PCI registry, the Blue Cross Blue Shield of Michigan Cardiovascular Consortium (BMC2), from January 2010 to December 2011 in Michigan. This registry enrolls all consecutive patients undergoing PCI at nonfederal hospitals in Michigan. The registry has been approved by the institutional review board of each participating hospital. Data were prospectively collected using standardized definitions and a standardized data collection form. In addition to a random audit of 2% of all cases, medical records of all patients who underwent multiple procedures or coronary artery bypass grafting and of patients who died in the hospital were reviewed to ensure data accuracy.
We divided the study population into those who underwent recent surgery and those undergoing PCI without having undergone recent surgery. Recent surgery was defined as a surgical procedure performed using general, spinal, or regional anesthesia in the 7 days before the PCI.
The primary end point was in-hospital mortality. Secondary end points included in-hospital cerebral vascular accident (CVA), bleeding event within 72 hours, clinical heart failure, cardiogenic shock after procedure, and stent thrombosis. CVA was defined as a loss of neurologic function severe enough to leave a persistent deficit for >24 hours and included hemorrhagic and occlusive strokes. Bleeding events were defined as a hematocrit decrease of ≥10% and/or hemoglobin drop of ≥3 g/dl and/or transfusion. Cardiogenic shock was defined as a sustained episode of systolic blood pressure of <90 mm Hg, and/or cardiac index of <2.2 L/min/m 2 secondary to cardiac dysfunction, and/or requirement for inotropic or vasopressor agents and/or mechanical support to maintain blood pressure and cardiac index above specified levels. Subacute stent thrombosis was defined by angiographic evidence of stent thrombosis in the original stent at repeat angiography.
Categorical data are summarized as a group percentage with group comparisons tested using the Fisher’s exact test. Continuous data are summarized as the mean ± SD and comparisons were made using Student t tests. Patient-predicted risk of mortality was estimated from the updated BMC2 mortality risk adjustment model. Area under the receiver operating characteristic curve was used to assess the discrimination of the risk model, with confidence intervals obtained by the Delong method.
Multivariate logistic regression models were fitted to the data with death as the outcome and postsurgical status, predicted mortality risk, and a risk by status interaction as predictors to evaluate the effect of a recent surgery on the risk of death adjusting for model-predicted risk and to determine whether that effect varied across the continuum of risk as estimated by other baseline clinical characteristics.
Patients were grouped by predicted mortality risk into 3 categories: <1%, 1% to 3%, and >3% of predicted risk. Within each group, the ratio of observed to expected mortality (O/E ratio) was compared graphically between postsurgical and other patients.
A generalized propensity score was developed using logistic regression models to estimate the likelihood that a given observation was postoperative based on other baseline clinical covariates. Postoperative and other patients were then matched on a 1:1 basis without replacement using the estimated propensity score to identify an analysis cohort balanced on baseline covariates. All analysis was performed in R version 2.14.
Results
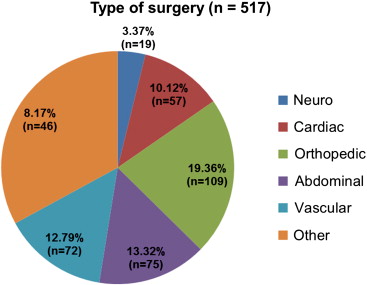
Of a total of 65,175 PCIs performed during the study period, 517 patients had undergone a surgical procedure in the previous 7 days. The respective number and anatomic distribution of surgical procedures are depicted in Figure 1 . The proportion of patients undergoing PCI after surgery was small at each of the participating institutions (median 0.7%, interquartile range 0.6% to 1.1%) and overall made up to only 0.8% of the total PCI volume. Baseline characteristics of patients who received PCI after a recent surgery and those receiving PCI without a recent surgery are listed in Table 1 . In the postoperative PCI group, a greater prevalence of end-stage renal disease requiring dialysis, peripheral arterial disease, cerebrovascular disease, diabetes, chronic lung disease, recent gastrointestinal bleed, and atrial fibrillation were observed. Patients who received PCI after a surgical procedure had higher rates of heart failure, left ventricular systolic dysfunction, cardiogenic shock within 24 hours, and cardiac arrest within 24 hours. Patients receiving PCI after a recent surgical procedure were more likely to be receiving immediate PCI for ST elevation myocardial infarction (STEMI) or non-STEMI.
| Variable | Unadjusted | Propensity Matched | ||||
|---|---|---|---|---|---|---|
| Postsurgical PCI, n = 517 (%) | Other PCI, n = 64,658 (%) | p | Postsurgical PCI, n = 505 (%) | Other PCI, n = 505 (%) | p | |
| Age (yrs) | 68.5 ± 11.3 | 65.3 ± 12.1 | <0.001 | 68.5 ± 11.3 | 67.9 ± 11.3 | 0.44 |
| Men | 59.2 | 66.1 | <0.001 | 59.2 | 59.2 | 1.00 |
| White | 84.7 | 86.9 | 0.15 | 84.6 | 81.2 | 0.16 |
| Black | 13.0 | 10.6 | 0.09 | 13.1 | 15.0 | 0.37 |
| Asian | 1.4 | 1.0 | 0.34 | 1.4 | 1.2 | 0.78 |
| Hispanic | 1.0 | 1.3 | 0.46 | 1.0 | 2.0 | 0.19 |
| Native American | 0.2 | 0.2 | 0.83 | 0.2 | 1.2 | 0.06 |
| Current smoker | 25.5 | 29.4 | 0.06 | 25.5 | 25.7 | 0.94 |
| Former smoker | 38.5 | 31.8 | 0.001 | 38.4 | 33.3 | 0.09 |
| Hypertension ∗ | 89.8 | 85.0 | 0.003 | 89.9 | 89.9 | 1.00 |
| Dyslipidemia † | 80.3 | 83.3 | 0.07 | 80.4 | 76.4 | 0.13 |
| Family history of premature CAD | 13.5 | 20.82 | <0.001 | 13.3 | 16.8 | 0.11 |
| Previous MI | 38.3 | 35.0 | 0.12 | 38.0 | 37.6 | 0.90 |
| History of heart failure | 23.0 | 15.4 | <0.001 | 23.6 | 21.6 | 0.45 |
| Previous valve surgery | 3.3 | 1.6 | 0.002 | 3.4 | 1.8 | 0.11 |
| Significant valve disease | 10.4 | 5.4 | <0.001 | 10.7 | 10.7 | 1.00 |
| Previous PCI | 40.4 | 44.9 | 0.04 | 40.4 | 37.8 | 0.40 |
| Previous CABG | 20.3 | 18.7 | 0.36 | 20.2 | 21.2 | 0.70 |
| Previous ICD | 4.6 | 2.7 | 0.008 | 4.8 | 3.6 | 0.34 |
| Patient height (cm) | 170.1 ± 10.4 | 171.1 ± 10.6 | 0.03 | 170.0 ± 10.5 | 169.6 ± 11.4 | 0.56 |
| Patient weight (kg) | 87.5 ± 20.2 | 89.5 ± 21.3 | 0.02 | 87.7 ± 20.3 | 87.4 ± 22.7 | 0.81 |
| BMI (kg/m 2 ) | 30.2 ± 6.3 | 30.6 ± 7.8 | 0.19 | 30.3 ± 6.4 | 30.5 ± 8.6 | 0.73 |
| Currently on dialysis | 7.2 | 2.2 | <0.001 | 7.1 | 6.7 | 0.80 |
| Cerebrovascular disease | 23.8 | 15.2 | <0.001 | 24.2 | 26.1 | 0.47 |
| PAD | 29.2 | 16.5 | <0.001 | 29.1 | 25.5 | 0.20 |
| Chronic lung disease | 25.7 | 18.4 | <0.001 | 25.9 | 24.6 | 0.61 |
| Diabetes mellitus | 45.3 | 37.1 | <0.001 | 45.4 | 46.1 | 0.80 |
| Current or recent GI bleed | 5.6 | 1.1 | <0.001 | 5.7 | 5.7 | 1.00 |
| Atrial fibrillation | 19.3 | 10.5 | <0.001 | 19.8 | 19.6 | 0.94 |
| Cardiac transplant | 0 | 0.1 | 0.581 | 0 | 0 | NA |
| Heart failure within 24 h prior to PCI | 26.9 | 9.9 | <0.001 | 27.5 | 21.8 | 0.03 |
| LV systolic dysfunction | 14.3 | 10.3 | 0.002 | 14.3 | 16.4 | 0.34 |
| Cardiogenic shock within 24 h | 7.5 | 1.6 | <0.001 | 7.1 | 6.3 | 0.62 |
| Cardiac arrest within 24 h | 5.0 | 1.8 | <0.001 | 4.6 | 7.1 | 0.08 |
| STEMI (within 7 days) | 26.1 | 14.9 | <0.001 | 25.5 | 26.3 | 0.77 |
| NSTEMI (within 7 days) | 40.2 | 18.5 | <0.001 | 40.6 | 42.4 | 0.57 |
| Unstable angina | 23.0 | 36.7 | <0.001 | 23.0 | 20.8 | 0.40 |
| Other CAD presentation | 10.6 | 29.9 | <0.001 | 10.9 | 10.5 | 0.84 |
∗ Hypertension is defined by any 1 of the following: a history of hypertension diagnosed and treated with medication, diet, and/or exercise, previous documentation of blood pressure of ≥140 mm Hg systolic and/or 90 mm Hg diastolic for patients without diabetes or chronic kidney disease, or previous documentation of blood pressure of ≥130 mm Hg systolic or 80 mm Hg diastolic on at least 2 occasions for patients with diabetes or chronic kidney disease.
† Dyslipidemia is defined as a history of dyslipidemia that was diagnosed and/or treated by a physician, or levels of total cholesterol >200 mg/dl, low-density lipoprotein ≥130 mg/dl, and high-density lipoprotein <40 mg/dl in men and <50 mg/dl in women, or currently receiving antilipidemic treatment.
The preprocedural, intraprocedural, and postprocedural medications used are listed in Table 2 . Patients undergoing PCI within 7 days after surgery were more likely to require vasopressors before, during, and after the procedure. There was no major difference in the periprocedural anticoagulation with glycoprotein IIb/IIIa inhibitor and bivalirudin use being similar in both groups.
| Medication | Before Procedure | During Procedure | After Procedure | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Postsurgical PCI (%) | Other PCI (%) | p | Postsurgical PCI (%) | Other PCI (%) | p | Postsurgical PCI (%) | Other PCI (%) | p | |
| Aspirin | 89.8 | 92.9 | 0.005 | 5.6 | 4.3 | 0.16 | 94.4 | 94.3 | 0.95 |
| Clopidogrel | 43.7 | 45.5 | 0.42 | 49.5 | 47.9 | 0.47 | 83.6 | 78.3 | 0.004 |
| Prasugrel | 1.7 | 3.7 | 0.02 | 5.8 | 11.8 | <0.001 | 7.9 | 14.9 | <0.001 |
| Abciximab | 0.2 | 0.1 | 0.42 | 3.3 | 1.9 | 0.02 | 1.7 | 1.3 | 0.37 |
| Eptifibatide | 3.3 | 5.2 | 0.06 | 26.3 | 31.7 | 0.01 | 19.9 | 25.3 | 0.005 |
| GPI | 3.5 | 5.3 | 0.06 | 29.8 | 33.5 | 0.07 | 21.5 | 26.7 | 0.008 |
| Bivalirudin | 0.4 | 0.4 | 0.89 | 32.9 | 36.5 | 0.09 | 1.9 | 3.4 | 0.06 |
| Vasopressor | 10.3 | 1.3 | <0.001 | 15.7 | 4.5 | <0.001 | 10.8 | 2.3 | <0.001 |
| Statin | 62.5 | 60.9 | 0.45 | NA | NA | NA | 76.4 | 78.3 | 0.31 |
| β Blocker | 72.5 | 68.0 | 0.03 | NA | NA | NA | 80.7 | 84.9 | 0.008 |
The unadjusted primary end point of death was significantly greater in the postsurgical PCI group ( Table 3 and Figure 2 ). Unadjusted secondary end points of CVA, bleeding events within 72 hours, heart failure, and cardiogenic shock were also significantly greater in those patients receiving PCI in the postsurgical period ( Table 3 and Figure 2 ). Rates of acute stent thrombosis were similar.



