32 Occlusion of Septal Defects
Atrial Septal Defect
 Basics
Basics
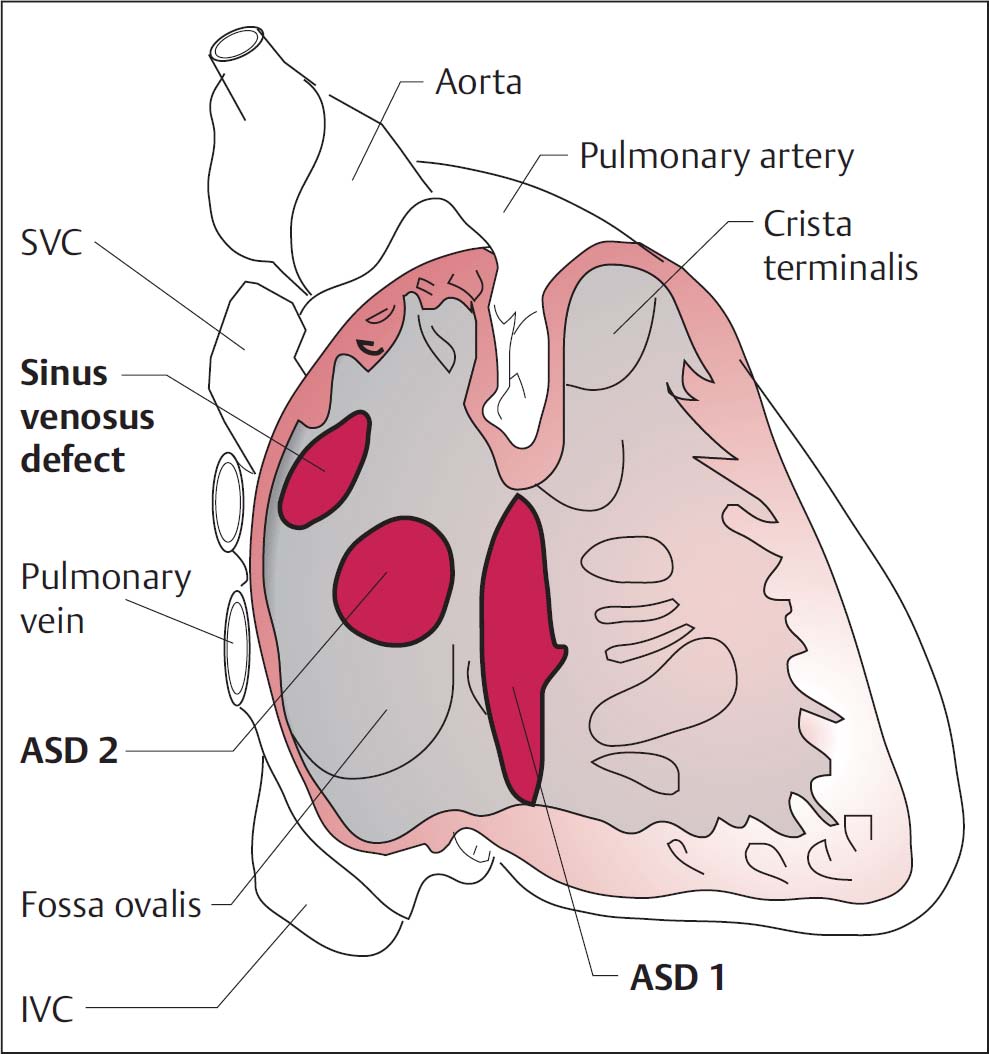
At approximately 8 % of all congenital heart defects, atrial septal defect (ASD) is one of the most common. Many patients only become symptomatic as adults. Major signs and symptoms associated with ASD are right ventricular failure and pulmonary hypertension with dyspnea and peripheral edema. Other complaints are supraventricular arrhythmias or recurrent pulmonary infections. Women are 1.5 to 2.5 times more frequently affected than men. Anatomically three forms can be differentiated (Fig. 32.1):
 Septum primum defect (ASD type 1): variant of an atrioventricular defect, most often with involvement of the AV valves (cleft formation).
Septum primum defect (ASD type 1): variant of an atrioventricular defect, most often with involvement of the AV valves (cleft formation).
 Septum secundum defect (ASD type 2): the most frequent form, it is a true defect in the fossa ovalis, associated in ~25 % with partial anomalous pulmonary venous return.
Septum secundum defect (ASD type 2): the most frequent form, it is a true defect in the fossa ovalis, associated in ~25 % with partial anomalous pulmonary venous return.
 Sinus venosus defect: ~11 % of all ASDs, always associated with partial anomalous pulmonary venous return.
Sinus venosus defect: ~11 % of all ASDs, always associated with partial anomalous pulmonary venous return.
Clinical findings are a fixed, wide split in the second heart sound and an early systolic murmur in the left parasternal region in the second to third intercostal space. The ECG shows right axis deviation and a rSR′ configuration or a complete right bundle branch block. The chest radiograph shows signs of right ventricular overload and an enlarged pulmonary segment as a result of right ventricular volume overload. The definitive diagnostic modality is echocardiography (transthoracic [TTE] and transesophageal [TEE]). It provides information on the morphology of the defect and on the anatomy of the pulmonary veins (anomalous return?), as well as on concomitant heart defects and intracavitary thrombi. Doppler and color Doppler echocardiography as well as contrast echocardiography (wash-out phenomenon) are used to assess the shunt. Invasive catheterization of both the right and left heart provides hemodynamic quantification of the shunt and can detect other comorbidities. Alternatively, cardiac MRI also allows imaging of the morphology and, with phase contrast imaging, the left-to-right shunt can be quantified.
Fig. 32.1 Different types of atrial septal defects (ASD). SVC, superior vena cava; IVC, inferior vena cava.
 Indications and Contraindications
Indications and Contraindications
Only the most frequent form of ASD—the septum secundum defect without partial anomalous pulmonary venous return—is amenable to interventional occlusion. A precise morphological and hemodynamic examination of the defect is required prior to intervention.
The procedure may be indicated if the following criteria are met:
 ASD type 2 without partial anomalous pulmonary venous return
ASD type 2 without partial anomalous pulmonary venous return
 Ratio of pulmonary/systemic flow > 1.5:1
Ratio of pulmonary/systemic flow > 1.5:1
 Defect < 30 mm (non–balloon-stretched diameter)
Defect < 30 mm (non–balloon-stretched diameter)
 Pulmonary arterial resistance is markedly less than systemic resistance ASD occlusion is not indicated or is contraindicated for
Pulmonary arterial resistance is markedly less than systemic resistance ASD occlusion is not indicated or is contraindicated for
 Fixed pulmonary hypertension with right-to-left shunt, where the pulmonary arterial resistance exceeds the systemic resistance (Eisenmenger reaction)
Fixed pulmonary hypertension with right-to-left shunt, where the pulmonary arterial resistance exceeds the systemic resistance (Eisenmenger reaction)
 Partial anomalous pulmonary venous return
Partial anomalous pulmonary venous return
 Detectable left atrial thrombi
Detectable left atrial thrombi
 Rim of the septum missing or width < 5 mm
Rim of the septum missing or width < 5 mm
 Instruments
Instruments
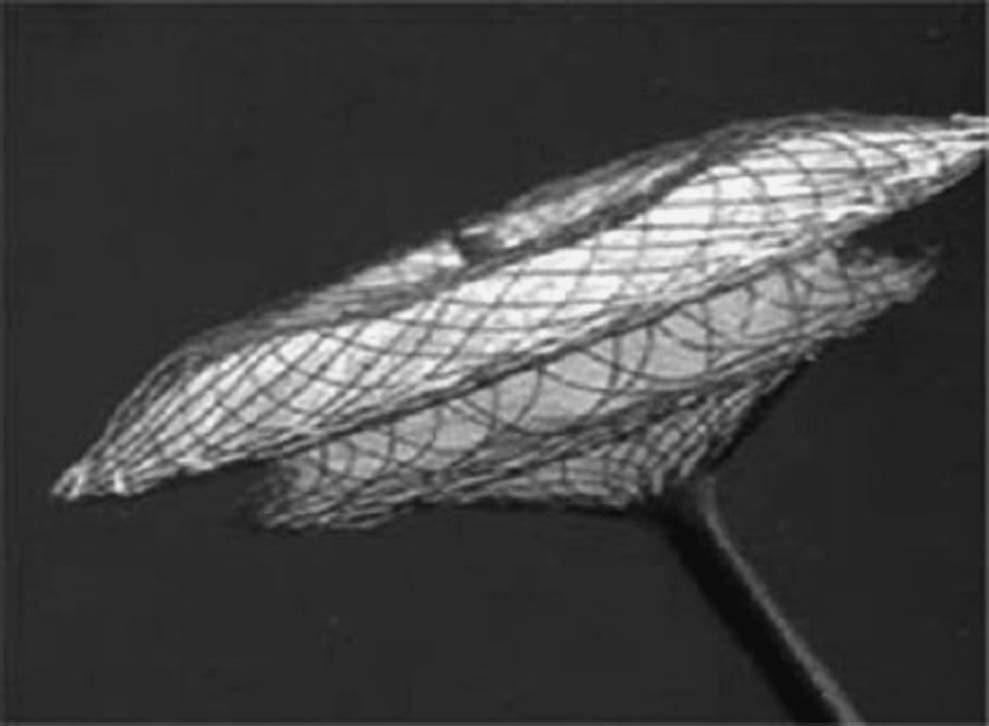
Numerous systems are available for interventional occlusion. The Amplatzer septal occluder (St. Jude Medical, St. Paul, MN, USA) is the system most commonly used. It is a prefabricated, self-centering device made of nitinol wire available in various sizes (Fig. 34.2). Alternatives include the Helex occluder (Gore Medical, Flagstaff, AZ, USA), the Occlutech occluder (Occlutech International AB, Helsingborg, Sweden), and the Atriasept occluder (Cardia, Inc., Eagan, MN, USA). For patients with a multifenestrated ASD, which previously could only be treated surgically, there are now also interventional options available.
The occluders of the individual manufacturers are available in different sizes from 4 to almost 40 mm. The diameter of the left and right atrial disks vary with the diameter of the connection waists. The breadth of the connection waists is 3 to 4 mm.
The following materials are required for the procedure:
 8F to 12F sheath, depending on the defect and device size
8F to 12F sheath, depending on the defect and device size
 5F to 7F multipurpose diagnostic catheter
5F to 7F multipurpose diagnostic catheter
 Amplatz Super Stiff Guidewire, 300 cm, J-tip
Amplatz Super Stiff Guidewire, 300 cm, J-tip
 Sizing balloon with 25, 30, or 40 mm diameter (depending on defect size) with radiopaque markers for calibration
Sizing balloon with 25, 30, or 40 mm diameter (depending on defect size) with radiopaque markers for calibration
 Long 8F to 12F sheath/delivery system
Long 8F to 12F sheath/delivery system
 Occlusion system in different sizes
Occlusion system in different sizes
Fig. 32.2 Amplatzer Septal Occluder with the connecting waist, which occludes the defect, the left and right atrial disks, and the screwed-on cable.
We perform the intervention with the patient either in deep sedation or under anesthesia with endotracheal intubation, as the intervention is continuously monitored by TEE, which most patients do not tolerate well when supine.
 Procedure
Procedure
 Place an 8F to 12F sheath in the femoral vein.
Place an 8F to 12F sheath in the femoral vein.
 Administer heparin (100 IU/kg body weight).
Administer heparin (100 IU/kg body weight).
 Give perisurgical antibiotic prophylaxis.
Give perisurgical antibiotic prophylaxis.
 Place the TEE probe for 360° imaging of the defect.
Place the TEE probe for 360° imaging of the defect.
 On crossing of the septal defect with the multipurpose catheter, use biplane fluoroscopy in AP and 90° LAO projection.
On crossing of the septal defect with the multipurpose catheter, use biplane fluoroscopy in AP and 90° LAO projection.
 Angiographic imaging of the catheter position, ideally in the left superior pulmonary vein.
Angiographic imaging of the catheter position, ideally in the left superior pulmonary vein.
 Confirm that the catheter is not positioned in the left auricle.
Confirm that the catheter is not positioned in the left auricle.
 Place the Amplatz Super Stiff Guidewire in the left superior pulmonary vein and withdraw the diagnostic catheter.
Place the Amplatz Super Stiff Guidewire in the left superior pulmonary vein and withdraw the diagnostic catheter.
 Advance the sizing balloon into the defect and slowly manually fill the balloon with diluted contrast medium (~1:3), without exerting substantial pressure; there should be constant fluoroscopic (and echocardiographic) monitoring with low pressure.
Advance the sizing balloon into the defect and slowly manually fill the balloon with diluted contrast medium (~1:3), without exerting substantial pressure; there should be constant fluoroscopic (and echocardiographic) monitoring with low pressure.
 Measure the waist of the expanded balloon by echocardiography and by angiography after calibration (either using the radiopaque markers on the sizing balloon or, preferably, using a previously imaged calibration sphere → balloon-stretched diameter of the defect) (Fig. 32.3).
Measure the waist of the expanded balloon by echocardiography and by angiography after calibration (either using the radiopaque markers on the sizing balloon or, preferably, using a previously imaged calibration sphere → balloon-stretched diameter of the defect) (Fig. 32.3).
 Perform measurements in several planes.
Perform measurements in several planes.
 Confirm with color Doppler that the defect is completely occluded by the expanded balloon.
Confirm with color Doppler that the defect is completely occluded by the expanded balloon.
 Select the appropriately sized occluder:
Select the appropriately sized occluder:
– In the size of the balloon-stretched diameter of the defect or rounded up to the next larger disk size (e.g., when 17.3 mm is measured, implantation of an 18-mm disk)
– If an aortic septal rim is lacking or only very narrow, the occluder should be selected two to three sizes (not 2–3mm) larger (i.e., for an 18.5-mm defect a size 24 occluder)
 The occluder is screwed onto the delivery cable and is introduced into the supplied loading sheath submerged in a water bath to reduce the chance of air entrapment in the delivery system.
The occluder is screwed onto the delivery cable and is introduced into the supplied loading sheath submerged in a water bath to reduce the chance of air entrapment in the delivery system.
 Place the long sheath (diameter depends on occluder size) transseptally into the left atrium and remove the Amplatz wire.
Place the long sheath (diameter depends on occluder size) transseptally into the left atrium and remove the Amplatz wire.
 If ventilated: increase PEEP to 10 mm Hg.
If ventilated: increase PEEP to 10 mm Hg.
 The loading sheath with the occluder is connected to the long sheath without introducing air. Then advance the occluder to the end of the sheath.
The loading sheath with the occluder is connected to the long sheath without introducing air. Then advance the occluder to the end of the sheath.
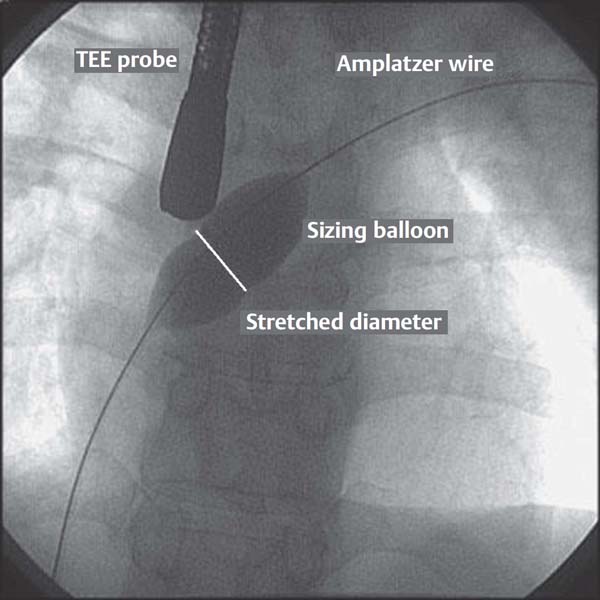
Fig. 32.3 Measurement of the defect with a sizing balloon and determination of the balloon-stretched diameter at the waist of the balloon. The measurement is done using both TEE and the angiographic image.
 Deploy the left atrial disk when its location in the left atrium is confirmed and it is freely movable.
Deploy the left atrial disk when its location in the left atrium is confirmed and it is freely movable.
 Pull back the system to the septum under fluoroscopic and echocardiographic guidance.
Pull back the system to the septum under fluoroscopic and echocardiographic guidance.
 When the left atrial disk is in close contact with the septum, pulsations can often be felt at the sheath and at the cable.
When the left atrial disk is in close contact with the septum, pulsations can often be felt at the sheath and at the cable.
 Deploy the right atrial disk by pulling back the sheath over the cable.
Deploy the right atrial disk by pulling back the sheath over the cable.
 After the expansion of the occluder, advance the cable so that the occluder assumes its flat configuration.
After the expansion of the occluder, advance the cable so that the occluder assumes its flat configuration.
 Echocardiographically document correct implantation:
Echocardiographically document correct implantation:
– Correct position
– Defect occluded according to color Doppler; a minimal central residual shunt through the occluder is always present acutely and closes spontaneously over time
– Safe distance from the mitral valve
 Safe distance from the coronary sinus
Safe distance from the coronary sinus
 Confirm the stability of the occluder by “wiggling” with the cable.
Confirm the stability of the occluder by “wiggling” with the cable.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree