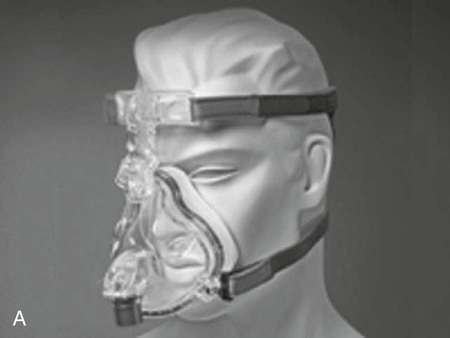
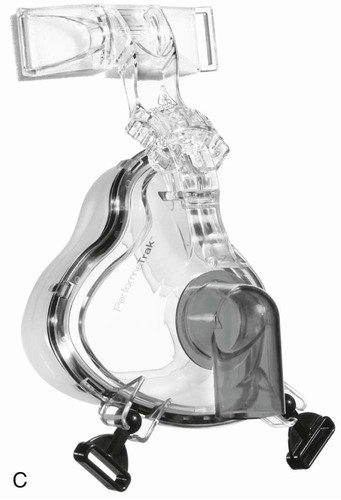
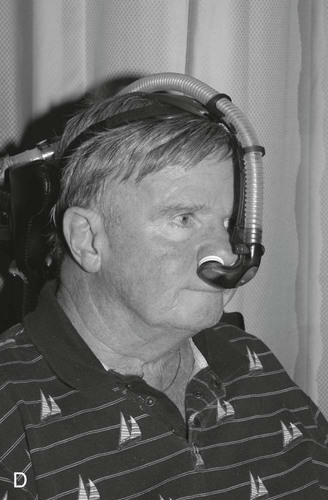
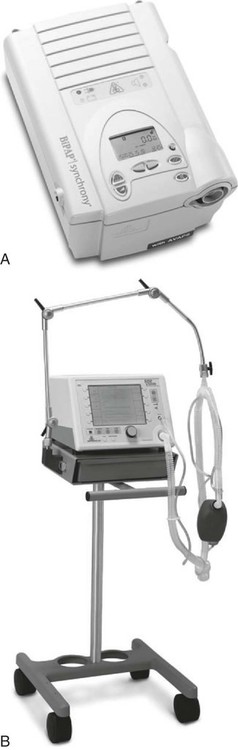
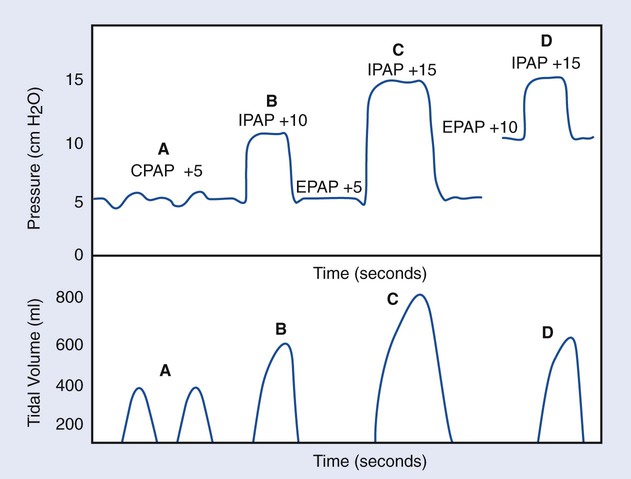
1. Identify the goals and benefits of noninvasive ventilatory support. 2. List the indications, selection, and exclusion criteria for successful noninvasive ventilation (NIV). 3. List the predictive factors for successful NIV. 4. Identify types of interfaces used in conjunction with NIV and their complications during use. 6. Describe how NIV settings influence physiologic outcomes of the patient. 7. Perform a continuous positive airway pressure (CPAP) or bilevel positive airway pressure (BiPAP) patient-ventilator system assessment. Delivery of ventilatory support without using an invasive artificial airway is termed noninvasive ventilation (NIV). NIV may include the application of continuous positive airway pressure (CPAP) or bilevel positive airway pressure (BiPAP). NIV is used to maintain or improve oxygenation and ventilation and to provide respiratory muscle rest. A listing of the goals of NIV is provided in Box 21-1. Typically, NIV is delivered via a nasal mask, a pillow, or a full face mask. Images of these devices, or interfaces, are provided in Figure 21-1. Selection of an interface device that fits properly and that the patient is comfortable with is important to help ensure patient compliance and use. Selection factors such as facial features, ease of use, patient preference, and, of course, availability, should all be taken into consideration when choosing an interface. Complications such as pulmonary infection and tracheal injury, which are associated with invasive mechanical ventilation, make NIV highly advantageous as a ventilatory management therapy. However, some exclusions of its use include refractory asthma, hemodynamic instability, excessive secretions, severe agitation, inability to protect the airway, and apnea. The patient’s medical history, current respiratory complaints, and concurrent medical therapies must be evaluated when choosing NIV therapy to facilitate the best therapeutic outcomes for your patients. Disease processes for which treatment with NIV may be useful are listed in Box 21-2. NIV is used in many realms of respiratory care, ranging from the acute care, long-term care, and home care to polysomnography and sleep medicine. This chapter will focus on its use in the acute and long-term care settings. Its use in preventing airway obstruction during sleep will be discussed in Chapter 28. Over time, clinical judgment and experience will influence your choice of patients likely to benefit from NIV therapy. Until then, selection criteria and guidance from clinical preceptors, physicians, and instructors should be your foundation. A comprehensive physical assessment is essential prior to application of NIV in the long-term setting. However, in the acute care setting and emergent situations, this may not be possible. Selection and exclusion criteria for NIV are provided in Box 21-3. The two forms of NIV discussed here are CPAP and BiPAP. CPAP is the noninvasive application of continuous pressure whereby the patient breathes spontaneously without mechanical assistance against threshold resistance, with pressures above atmospheric pressure maintained at the airway throughout breathing Examples of the devices used to deliver CPAP and BiPAP can be found in Figure 21-2. Initial CPAP pressure settings are generally around 8 to 12 cm H2O, with various oxygen concentrations used to meet the patient’s needs. BiPAP is a spontaneous breathing mode of support, which allows separate regulation of the inspiratory positive airway pressure (IPAP) and expiratory positive airway pressure (EPAP). The pressure difference between the IPAP and the EPAP, which is called the driving pressure or delta P (ΔP), determines the tidal volume being delivered. This concept is illustrated in Figure 21-3. IPAP is associated with ventilation, whereas the EPAP setting is used for oxygenation. The following is the step-by-step process for initiation of noninvasive ventilation. 1. Review the patient’s chart. 2. Verify the physician’s order or the facility’s protocol for standard of care. 3. Obtain, clean, and inspect appropriate equipment prior to entering the patient’s room. 4. Follow personal protective equipment (PPE) requirements, and observe standard precautions for any transmission-based isolation procedure. 5. Identify the patient using two patient identifiers. 6. Follow the facility’s protocol for patient interaction, and introduce yourself to the patient and to the family. 7. Explain the procedure to the patient and to the family, and acknowledge the patient’s understanding. 8. Perform proper hand hygiene, and put on gloves, mask, and protective eyewear, as appropriate for the procedure. 1. Place the patient in a comfortable position. 3. Determine the noninvasive interface for use with CPAP or BiPAP. 4. Ensure proper fit of the interface to prevent excessive leaks. 5. Assemble the circuit, plug it in, attach to the gas source(s), and test the device. 6. Connect the device to the patient, and readjust the interface, as needed, to prevent leaks. 7. Reassess vital signs, and monitor the patient. 8. Remove the supplies from the patient’s room, and clean the area, as needed. 9. Remove PPE, and perform proper hand hygiene prior to leaving the patient’s room.
Noninvasive Ventilatory Support
Equipment





» Skill Check Lists
21-1 Initiating Noninvasive Ventilation: CPAP and BiPAP

Procedural Preparation
Implementation
Noninvasive Ventilatory Support


















