Perioperative management of patients after percutaneous coronary intervention presents physicians with unique challenges and dilemmas. Although newer generation drug-eluting stents, transcatheter-based therapies, and minimally invasive surgical techniques have changed the medical landscape, guidelines for managing perioperative patients after percutaneous intervention are based largely on expert opinion and inconsistent data from an earlier era. In conclusion, the aims of this review are to summarize the data pertinent to managing patients after percutaneous coronary intervention in the perioperative period and to explore future perspectives.
Approximately 600,000 percutaneous coronary interventions (PCIs) are performed annually in the United States. The incidence of noncardiac surgery (NCS) after PCI has been reported to range from 4% to 11% in the first year and from 7% to 34% in the first 2 years after index PCI. With an aging population, the incidence of coronary disease and the use of PCI may further increase, resulting in a greater incidence of NCS after PCI. Clear understanding of the characteristics of the post-PCI and perioperative states and the effects of overlap of the 2 states is imperative for the optimal management of this patient group.
Unique Characteristics of the Postoperative State
Contrary to the common belief that the risk for perioperative myocardial ischemia is greatest during anesthesia induction or intraoperatively, studies have revealed that the risk peaks 2 to 3 days after NCS, unless there is significant left main coronary artery or multivessel disease. Surgical stress results in sympathetic activation, with release of norepinephrine, epinephrine, cortisol, and renin. Plasminogen activator inhibitor levels increase and endogenous tissue plasminogen activator levels decrease, causing decreased fibrinolysis, while procoagulant factors increase. The cumulative result is an intensely prothrombotic, proinflammatory, and catabolic state. Consequently, the risk for thrombosis in the setting of newly deployed nonendothelized stents is enhanced. Coupled with cessation of antiplatelet therapy, as might occur in preparation for surgery, the thrombotic risk is further increased, especially in the first 6 to 8 weeks after stent implantation, when the stent may not be endothelized. Furthermore, this metabolically active state can cause coronary spasm and increase shear stress on coronary plaques, leading to plaque disruption. Dawood et al performed histopathologic analysis on the coronary arteries of 42 patients who had perioperative myocardial infarctions (MIs) and reported plaque erosion or acute plaque disruption as the predominant pathology in this group. Additionally, fluid shifts, tachycardia, and increased cardiac output may result in myocardial demand-supply disparity, predisposing to ischemia and infarction. The unique pathophysiologic milieu of the postoperative state can lead to myocardial ischemia, even in patients without underlying coronary artery disease, but the risk is almost quadrupled in the setting of known coronary disease. The incidence of postoperative myocardial ischemia has been reported to range from 0.8% to 4.1% and is associated with mortality as high as 17% to 70%. It is therefore important to recognize the finite baseline risk for perioperative MI, even for apparently low-risk patients without known coronary disease.
Unique Characteristics of the Post-PCI State
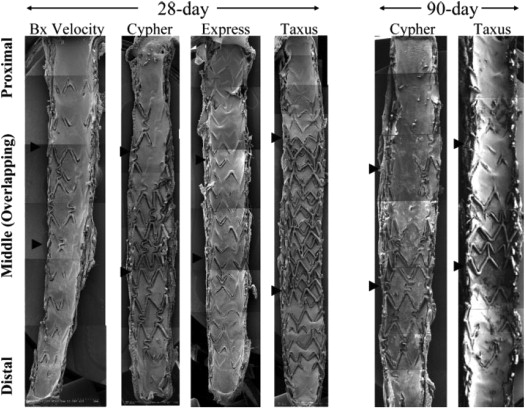
Stent implantation results in denudation of the endothelial surface, exposing the highly thrombogenic subendothelial surface while introducing a foreign object (the stent) into the milieu. The endothelium heals by reendothelization and neointima formation that occurs 6 to 8 weeks after bare-metal stent (BMS) implantation. In contrast, drug-eluting stents (DESs) consist of a metal stent platform, a polymer, and an antirestenotic drug. The controlled release of the antirestenotic agent prevents neointimal hyperplasia but also causes inflammation and endothelial dysfunction and predisposes to a longer period of thrombotic vulnerability ( Figure 1 ). Angioscopic studies have demonstrated delayed neointimal coverage of DES struts compared with BMS struts, and this has been associated with a longer period of higher thrombotic risk. Studies have revealed no overall difference in the frequency of stent thrombosis between DES and BMS, but a clear temporal variation has been described. The incidence of stent thrombosis peaks in the first 6 months after BMS and later with DES (late stent thrombosis [LST], occurring at 31 days to 1 year). The frequency of very late stent thrombosis (VLST; occurring after 1 year) was also reported to be higher after first-generation DESs. Second-generation DESs have been shown to have higher average tissue coverage thickness and a lower degree of uncovered struts, malapposed struts, inflammation, and less fibrin deposition compared with first-generation stents. All of these factors may theoretically protect against LST and VLST in second-generation stents.
Although stent thrombosis has a low reported incidence of <1%, it is associated with a 50% to 70% incidence of MI (usually ST-segment elevation MI) and high mortality of up to 40% ( Figure 2 ). Reddy and Vaitkus retrospectively studied patients who underwent NCS after PCI and reported that the risk for thrombosis-driven events persisted despite continuation of dual-antiplatelet therapy (DAPT), thereby underscoring the overwhelming effect of the thrombogenic postsurgical state. Numerous patient and procedural factors have been associated with stent thrombosis, including advanced age, diabetes, renal insufficiency, premature discontinuation of DAPT, smaller stent diameter, overlapping stent segments, bifurcation stenting, and longer stent lengths. The pathogenesis of stent thrombosis includes platelet activation and aggregation, leading to the development of an occlusive thrombus ( Figure 3 ). It is therefore reasonable to conclude that the key to preventing stent thrombosis is continuation of DAPT, if feasible, and certainly continuation of aspirin monotherapy at the minimum.
Unique Characteristics of the Post-PCI State
Stent implantation results in denudation of the endothelial surface, exposing the highly thrombogenic subendothelial surface while introducing a foreign object (the stent) into the milieu. The endothelium heals by reendothelization and neointima formation that occurs 6 to 8 weeks after bare-metal stent (BMS) implantation. In contrast, drug-eluting stents (DESs) consist of a metal stent platform, a polymer, and an antirestenotic drug. The controlled release of the antirestenotic agent prevents neointimal hyperplasia but also causes inflammation and endothelial dysfunction and predisposes to a longer period of thrombotic vulnerability ( Figure 1 ). Angioscopic studies have demonstrated delayed neointimal coverage of DES struts compared with BMS struts, and this has been associated with a longer period of higher thrombotic risk. Studies have revealed no overall difference in the frequency of stent thrombosis between DES and BMS, but a clear temporal variation has been described. The incidence of stent thrombosis peaks in the first 6 months after BMS and later with DES (late stent thrombosis [LST], occurring at 31 days to 1 year). The frequency of very late stent thrombosis (VLST; occurring after 1 year) was also reported to be higher after first-generation DESs. Second-generation DESs have been shown to have higher average tissue coverage thickness and a lower degree of uncovered struts, malapposed struts, inflammation, and less fibrin deposition compared with first-generation stents. All of these factors may theoretically protect against LST and VLST in second-generation stents.
Although stent thrombosis has a low reported incidence of <1%, it is associated with a 50% to 70% incidence of MI (usually ST-segment elevation MI) and high mortality of up to 40% ( Figure 2 ). Reddy and Vaitkus retrospectively studied patients who underwent NCS after PCI and reported that the risk for thrombosis-driven events persisted despite continuation of dual-antiplatelet therapy (DAPT), thereby underscoring the overwhelming effect of the thrombogenic postsurgical state. Numerous patient and procedural factors have been associated with stent thrombosis, including advanced age, diabetes, renal insufficiency, premature discontinuation of DAPT, smaller stent diameter, overlapping stent segments, bifurcation stenting, and longer stent lengths. The pathogenesis of stent thrombosis includes platelet activation and aggregation, leading to the development of an occlusive thrombus ( Figure 3 ). It is therefore reasonable to conclude that the key to preventing stent thrombosis is continuation of DAPT, if feasible, and certainly continuation of aspirin monotherapy at the minimum.
Noncardiac Surgery After Coronary Intervention
As evident from the preceding discussion, management of post-PCI patients in the metabolically active perioperative state poses unique challenges. These range from determination of optimal timing of the surgical procedure to balancing the risk for perioperative bleeding with that of stent thrombosis. In the following section, we strive to discuss these and provide a simplified approach to managing patients in this complex scenario.
Optimal timing of NCS after PCI
Current consensus multisociety guidelines suggest delaying elective surgery for ≥1 year after DES implantation and for ≥4 to 6 weeks after BMS implantation. If surgery is warranted before that period, it should be performed while on DAPT if safe. Minimums of 6 to 12 months and 4 to 6 weeks of DAPT, respectively, after DES and BMS implantation before NCS are recommended in national guidelines. If surgery is anticipated within 30 days of revascularization or if DAPT is not feasible, balloon angioplasty without stenting may be a reasonable strategy if NCS is anticipated. These recommendations are based largely on expert opinion in conjunction with limited and variable evidence based on first-generation DESs.
Early surgery after PCI can be hazardous. Schouten et al reported a 13.3% major adverse cardiac event (MACE) rate in patients who underwent NCS <1 month after BMS implantation or <3 to 6 months after DES implantation compared with 0.6% in patients who underwent surgery thereafter. Patients who underwent early NCS had a 31-fold higher MACE rate if DAPT was discontinued. Stent type was found to have no bearing on outcomes. A study from the Mayo Clinic by Nuttall et al examined 899 patients who underwent NCS after undergoing PCI with BMS. A MACE rate of 10.5% was found for surgery performed <30 days after PCI, 3.8% for surgery performed between 31 and 90 days, and 2.8% for surgery performed >90 days after PCI with BMS. A 3.5-fold increase in MACE rate was noted when NCS was performed <30 days after BMS implantation (in comparison with after 91 days), with the lowest MACE rate found for NCS performed >90 days after BMS implantation. Cruden et al demonstrated no difference in outcomes (in-hospital mortality or ischemic cardiac events) between DES- and BMS-treated patients who underwent NCS. They did, however, report a threefold higher major cardiac risk for surgery performed <6 weeks after PCI compared with surgery beyond 6 weeks while also reporting fourfold higher cardiac mortality for surgery performed 6 weeks to 1 year after PCI compared with beyond 1 year Wijeysundera et al reconfirmed increased 30-day MACE rates for NCS performed <45 days after PCI and reported risk normalization to nonrevascularized intermediate-risk levels 45 days after BMS implantation and 180 days after DES implantation respectively. Recently, Hawn et al reported stabilization of MACE risk at 6 months after BMS or DES implantation. They also confirmed an inverse association between the timing of NCS after PCI and MACE rate (11.6% at <6 weeks, 6.4% at 6 weeks to <6 months, 4.2% at 6 to 12 months, and 3.5% at >12 to 24 months; p <0.001). In another study from the Mayo Clinic, Rabbitts et al examined 520 patients who underwent NCS <2 years after PCI with DES and reported the lowest MACE rate (3.3%) for NCS performed 1 year after DES implantation and a disconcertingly high MACE rate (17.9%) for patients who underwent emergent surgery. This finding may be a surrogate for decreased MACEs for NCS performed after the course of thienopyridine therapy has been completed and is in line with current guidelines, which recommend deferring elective surgery for 12 months after DES. If surgery cannot be deferred, continuation of aspirin in the perioperative period should be strongly considered. In all series, emergency surgery has been found to be associated with a threefold to fourfold increase in MACE rates ranging from 12% to 18% for NCS after PCI with stenting. A recent large retrospective study identified the 3 factors most strongly associated with MACEs to be nonelective surgery, history of MI in the 6 months preceding NCS, and revised cardiac risk index >2.
Although stent thrombosis is well known to be a low-frequency yet serious event, in-stent restenosis is not a benign event either and presents with acute MI in 3.5% to 19.4% of cases. The risk for thrombosis is highest in the first 2 weeks after implantation and decreases progressively subsequently, whereas the risk for in-stent restenosis tends to increase over time, peaking at approximately 6 months for BMS and 12 months for DES. Thus, despite a fair bit of overlap between these 2 event curves, there may exist an optimal time window for performing surgery during which the rate of stent thrombosis is low because of reendothelization, however in-stent restenosis has yet to completely manifest itself ( Figure 4 ).

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


