The aim of our study was to examine the role of a new, simple protocol of intracoronary adenosine administration performed during primary angioplasty on the immediate angiographic results and clinical course. A prospective, single-center, randomized, placebo-controlled trial of 70 consecutive patients (64 ± 14 years, 54 men) with acute myocardial infarction with ST-segment elevation undergoing primary percutaneous coronary intervention (PCI) was conducted. Patients were randomized to 2 groups. Group 1 (n = 35) received intracoronary adenosine (1 to 2 mg) with a hand injection through the guiding catheter 2 times: immediately after crossing the lesion of the infarct-related artery with guidewire and then after the first balloon inflation. Group 2 (n = 35) received placebo. The baseline clinical and angiographic characteristics of the 2 groups were similar. Percutaneous coronary intervention resulted in Thrombolysis In Myocardial Infarction grade 3 flow after PCI in 32 patients (91.4%) in the adenosine group and 27 patients (77.1%) in the placebo group (p = 0.059). Myocardial blush grade 3 was observed at the end of PCI in 23 patients (65.7%) in the adenosine group and 13 (37.1%) in the placebo group (p <0.05). Resolution of ST-segment elevation (>50%) was more frequently observed in the adenosine than in the placebo group: 27 (77%) versus 15 (43%), respectively (p <0.01). In conclusion, intracoronary adenosine administration improved the angiographic and electrocardiographic results in patients with acute myocardial infarction with ST-segment elevation undergoing PCI. Adenosine administration seemed to be associated with a more favorable clinical course.
The presence of no-reflow during percutaneous coronary intervention (PCI) has been associated with worsened short- and long-term outcomes, an increased risk of subsequent major adverse events, and negative remodeling. Drug treatment aimed at reducing the no-reflow phenomenon could improve myocardial salvage, thus preventing left ventricular remodeling. Various treatment strategies, including the use of vasodilators, such as verapamil, diltiazem, and sodium nitroprusside, have been associated with an improvement in angiographic flow in several studies; however, whether these treatment strategies affect the clinical outcome has not been clear. Adenosine, which is capable of dilating the coronary resistance vessels and increasing flow, is also one of the used agents in the treatment of no-reflow. Moreover, adenosine antagonizes many of the biochemical and physiologic mechanisms implicated in ischemia–reperfusion injury and has been shown to reduce postischemic ventricular dysfunction and myocyte necrosis and apoptosis. The exact mechanisms of the cardioprotective effect of adenosine are not fully understood, although neutrophil activation and prevention of endothelial damage seem to play a major role. In animal models, adenosine limits reperfusion injury, reducing the infarct size and improving ventricular function. Also, data from some human studies have confirmed the beneficial effects of intracoronary adenosine. However, the widespread use of that drug has been limited owing to the complicated protocols of adenosine infusion during and after PCI. The aim of our study was to examine the role of a new simple protocol of adenosine administration performed during primary angioplasty on the immediate angiographic results and clinical course.
Methods
Patients with acute myocardial infarction with ST-segment elevation who had been referred for primary PCI within 6 hours of symptom onset were considered for the present study. The patients underwent diagnostic coronary angiography. If the culprit lesion was suitable for PCI and had presented with Thrombolysis In Myocardial Infarction (TIMI) flow 0 to 2, the patient was included in the present study and randomized after informed consent had been given. Patients presenting with TIMI flow 3 were not included in the present study. Patients with chronic obstructive pulmonary disease or asthma and those who had received previous thrombolysis were excluded from the present study. The ethics committee of our institution approved the study protocol, and all patients provided written informed consent.
Each patient received aspirin (300 mg) and clopidogrel (300 mg) ≥30 minutes before PCI. After intravenous administration of heparin (100 U/kg), left and right coronary angiography was performed using a femoral approach with Judkin’s technique. A venous sheath was also inserted into the femoral vein, and a temporary pacing wire and pacemaker left “on demand 70 beats/min” were ready on the table for possible immediate use.
The obstruction of the infarct related-artery was crossed with a 0.014-in. guidewire. Immediately after crossing the lesion, either adenosine (2 mg to the left or 1 mg to the right coronary artery in 10 ml 0.9% NaCl) or saline (10 ml 0.9% NaCl) was rapidly hand injected into the coronary artery through the guiding catheter. After 1 minute, the balloon catheter was advanced to the infarct-related artery, positioned at the level of the obstruction, and dilated with low pressure (4 to 6 atm) for a few seconds. Next, the balloon catheter was pulled out, and, again, either adenosine (2 mg to the left or 1 mg to the right coronary artery in 10 ml 0.9% NaCl) or saline (10 ml 0.9% NaCl) was rapidly hand injected into the coronary artery through the guiding catheter. The dilation procedure was completed according to the standard technique. Stenting of the dilated coronary segment was performed in all cases using bare metal stents. After completion of the dilation procedure, the second contrast injection for the assessment of TIMI flow and myocardial blush grade (MBG) was performed. The invasive procedure was limited to the culprit lesion in all patients. Glycoprotein IIb/IIIa inhibitors and an intra-aortic balloon pump were used at the discretion of the operator.
The angiograms were reanalyzed as a single group, in chronologic sequence, by 2 observers, who had not participated in the invasive procedure and were unaware of the treatment received. The TIMI flow grade was assessed, as defined previously. The analysis of coronary flow was also done according to the TIMI frame count method, as described by Gibson et al. The MBG was assessed using the method described by van’t Hof. The MBG was assessed by 2 observers who were unaware of the other’s findings and of the clinical data. ST-segment elevation was measured 60 ms after the J point on the initial electrocardiogram (on admission to the hospital) and on a second electrocardiogram performed 60 minutes after angioplasty. A ≥50% reduction in the sum of the ST-segment elevations on the second electrocardiogram was considered ST-segment elevation resolution. The electrocardiograms were analyzed in a blinded fashion by an experienced cardiologist. Creatine kinase, creatine kinase-MB, and troponins were assessed every 8 hours in the first day of admission, unless clinical events suggested the need for repeat measurements.
The physicians in charge of the patients on the coronary care floor were informed of the angiographic results of the primary PCI but were unaware of the study treatment administered during the procedure. The patients received standard pharmacologic treatment, including aspirin, clopidogrel, β blockers, angiotensin-converting enzyme inhibitors, and statins, unless contraindicated. Significant major cardiac events within 1 month of follow-up, including death, recurrent myocardial infarction, cardiac arrest, cardiogenic shock, and heart failure, were recorded. The recurrent episodes of significant angina that led to repeat angiography were also noted. A 2-dimensional echocardiogram with ejection fraction measurement using the modified Simpson rule was performed 5 to 7 days after primary coronary angioplasty. Interpretation of the examination was kept unaware of patient treatment.
The primary study end points were (1) the MBG at the end of procedure and (2) ST-segment elevation resolution 60 minutes after PCI. The secondary end points included the feasibility and safety of the new protocol of intracoronary adenosine administration in the setting of primary PCI, the final TIMI flow grade at the end of procedure, the TIMI frame count at the end of procedure, and the composite end point of death, recurrent myocardial infarction, cardiac arrest, cardiogenic shock, heart failure, and recurrent episodes of significant angina that led to repeat angiography and subsequent revascularization during 1 month of follow-up.
Data are expressed as the mean ± SD for continuous variables and as percentages for categorical variables. Continuous variables were compared using nonparametric tests (Mann-Whitney U test). The chi-square test was used to compare the categorical variables. p Values <0.05 were considered significant. Statistical analysis was performed using Statistica, version 8.0 (StatSoft Inc., Tulsa, Oklahoma).
Results
A total of 70 patients (64 ± 14 years, 54 men) were included in the present study. The patients were randomized into 2 groups. Group 1 (n = 35) received intracoronary adenosine twice and group B (n = 35) received placebo. Primary coronary angioplasty was successfully completed for all study patients. The baseline clinical and angiographic characteristics of the 2 groups were similar ( Table 1 ). Glycoprotein IIb/IIIa inhibitors (abciximab) were given to 18 patients, 10 (28.6%) in adenosine group and 8 (22.9%) in the placebo group (p = NS). An intra-aortic balloon pump was not used in any patient.
| Variable | Adenosine (n = 35) | Placebo (n = 35) |
|---|---|---|
| Age (years) | 65.3 ± 11 | 64.5 ± 13 |
| Male gender | 23 (63%) | 21 (60%) |
| Hypertension (>140/90 mm Hg) | 21 (60%) | 23 (63%) |
| Diabetes mellitus | 8 (23%) | 8 (23%) |
| Hypercholesterolemia (total cholesterol >5.2 mmol/L) | 27 (77%) | 29 (83%) |
| Smoker | 22 (63%) ⁎ | 13 (37%) ⁎ |
| Previous myocardial infarction | 3 (9%) | 4 (11%) |
| Symptom onset to needle (minutes) | 273 ± 137 | 225 ± 110 |
| Infarct-related coronary artery | ||
| Left anterior descending | 17 | 20 |
| Right | 14 | 10 |
| Left circumflex | 4 | 5 |
| Myocardial infarction location | ||
| Anterior | 17 | 20 |
| Inferior | 14 | 10 |
| Lateral | 4 | 5 |
| Multivessel coronary disease | 12 | 12 |
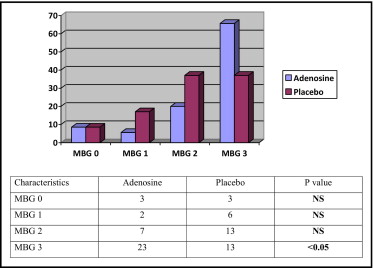
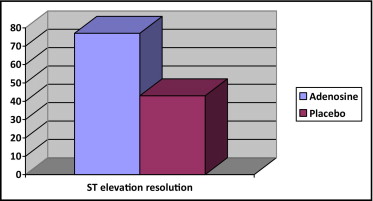
MBG 3 was observed in 23 patients (65.7%) in adenosine group and 13 patients (37.1%) in placebo group (p <0.05) at the end of PCI ( Figure 1 ). Resolution of ST-segment elevation (>50%) was more frequently observed in the adenosine than in the placebo group: 27 (77%) versus 15 (43%) patients, respectively (p <0.01; Figure 2 ).

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


