CHAPTER 65 Neuropsychological Deficits and Stroke
ASSESSMENT
Routine assessment of neurologic injury that occurs in the setting of cardiac surgery is not done for most patients because of the priority of the cardiac lesion and because of costs in time and money. General neurologic examinations by members of the surgical team or individuals lacking specialized training are not adequate to rule out subtle neurologic injuries, and this is the principal reason that the incidence of stroke and neurologic or neuropsychological injury varies widely in the surgical literature.1–3
The most obvious neurologic abnormalities are paresis, loss of vital brain functions (such as speech, vision, or comprehension), and coma. These are commonly lumped under the general heading of stroke. Disorders of awareness or consciousness can include coma, delirium, and confusion, but transitory episodes of delirium and confusion are often dismissed as due to anesthesia or medications. More subtle losses are determined by comparison of preoperative and postoperative performances with a standard battery of neuropsychological tests prepared by a group of neuropsychologists.4 A neuropsychological examination is basically an extension of the neurologic examination with a much greater emphasis on higher cortical function. Dysfunction is objectively defined as a deviation from the expected, relative to a large population. For example, although performing at a 95 IQ level is in the normal range, it is low for a physician, and a search for a neurologic impairment would be triggered by such a poor performance. A 20% decline in two or more of these test results, compared with the patient’s baseline, suggests a neuropsychological deficit that should be followed until it is resolved or not resolved.5 In studies involving long-term follow-up, the inclusion of a control group of nonsurgical patients with the same disease and of similar demographics helps define the causes of neuropsychological decline that occurs later than 3 to 6 months after surgery.6
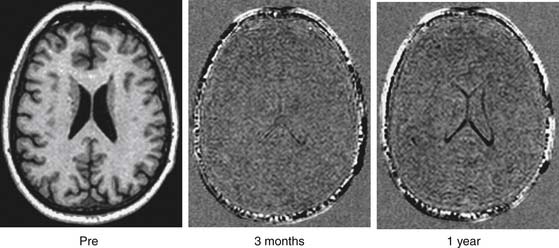
Computed axial tomograms or magnetic resonance imaging (MRI) scans are essential for the definitive diagnosis of stroke, delirium, or coma. Preoperative imaging is usually not necessary when new techniques such as diffusion-weighted MRI imaging, MRI spectroscopy, and MRI angiography are used to assess possible new lesions after operation.7–9 However, studies demonstrate that patients with dementia have a loss in cell volume due to microinfarctions that are not detectable with current radiologic techniques.64 Histologic studies performed on patients who did not survive cardiac surgery have demonstrated millions of small lipid microemboli that may result in massive cell loss and increased volume of ventricles (Fig. 65-1).
Biochemical markers of neurologic injury after cardiac surgery are relatively nonspecific and inconclusive. Neuron-specific enolase is an intracellular enzyme found in neurons, normal neuroendocrine cells, platelets, and erythrocytes.10 S-100 is an acidic calcium-binding protein found in the brain.11,12 The beta dimer resides in glial and Schwann cells. Both S-100 and neuron-specific enolase increase in spinal fluid with neuronal death11,12 and may correlate with stroke or spinal cord injury after CPB.13 However, plasma levels are contaminated by aspiration of wound blood into the pump and hemolysis and are often elevated after prolonged CPB in patients without otherwise detectable neurologic injury.14 Newer blood-borne biochemical markers are being identified but as yet have not been shown to be diagnostic for subtle neurologic injury.
POPULATIONS AT RISK
Advancing age increases the risk of stroke or cognitive impairment in the general population, and surgery, regardless of type, increases the risk still higher.15 In 1985, Gardner and colleagues16 reported the risk of stroke during coronary artery bypass graft surgery to be directly related to age. A European study compared 321 elderly patients without surgery to 1218 patients who had noncardiac surgery and found a 26% incidence of cognitive dysfunction 1 week after operation and a 10% incidence at 3 months.17 Between 1974 and 1990, the number of patients older than 60 years and older than 70 years undergoing cardiac surgery increased twofold and sevenfold, respectively.18 Genetic factors also influence the incidence of cognitive dysfunction after cardiac surgery.19 The incidence of cognitive dysfunction at 1 week after cardiac surgery is approximately double that of noncardiac surgery.
As the age of cardiac surgical patients increases, the number with multiple risk factors for neurologic injury also increases. Risk factors for adverse cerebral outcomes are listed in Table 65-1.20 These factors are divided into stroke with a permanent fixed neurologic deficit (type I) and coma or delirium (type II). Hypertension and diabetes occur in approximately 55% and 25% of cardiac surgical patients, respectively.21 Fifteen percent have carotid stenosis of 50% or greater, and up to 13% have had a transient ischemic attack or prior stroke. The total number of MRI atherosclerotic lesions in the brachiocephalic vessels adds to the risk of stroke or cognitive dysfunction,22 as does the severity of atherosclerosis in the ascending aorta as detected by epiaortic ultrasound scanning.23 Palpable ascending aortic atherosclerotic plaques markedly increase the risk of right carotid arterial emboli as detected by Doppler ultrasound examination.24 The incidence of severe aortic atherosclerosis is 1% in cardiac surgical patients younger than 50 years and 10% in those aged 75 to 80 years.25
Table 65–1 Adjusted Odds Ratios for Type I and Type II Cerebral Outcomes Associated with Selected Risk Factors
| Factor | Model for Type I Cerebral Outcome | Model for Type II Cerebral Outcome |
|---|---|---|
| Significant factors, P < .05 | ||
| Proximal aortic atherosclerosis | 4.52 | |
| History of neurologic disease | 3.19 | |
| Use of intra-aortic balloon pump | 2.60 | |
| Diabetes mellitus | 2.59 | |
| History of hypertension | 2.31 | |
| History of pulmonary disease | 2.09 | 2.37 |
| History of unstable angina | 1.83 | |
| Age (per additional decade) | 1.75 | 2.20 |
| Systolic blood pessure > 180 mm Hg at admission | 3.47 | |
| History of excessive alcohol consumption | 2.64 | |
| History of CABG | 2.18 | |
| Dysrhythmia on day of surgery | 1.97 | |
| Antihypertensive therapy | 1.78 | |
| Other factors (P not significant) | ||
| Perioperative hypotension | 1.92 | 1.88 |
| Ventricular venting | 1.83 | |
| Congestive heart failure on day of surgery | 2.46 | |
| History of peripheral vascular disease | 1.64 |
Modified from Roach GW, Kanchuger M, Mangano CM, et al. Adverse cerebal outcomes after coronary bypass surgery. Multicenter Study of Perioperative Ishemia Research Group and the Ischemia Research and Education Foundation Investigators.
MECHANISMS OF INJURY
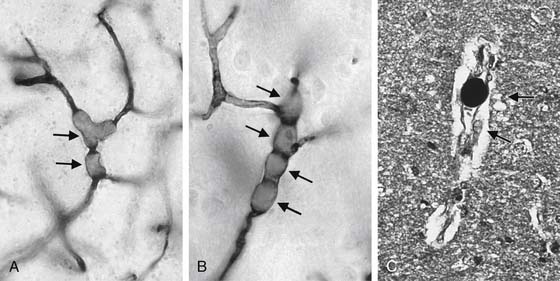
The three major causes of neurologic dysfunction and injury during cardiac surgery are microemboli, hypoperfusion, and a generalized inflammatory reaction that can occur in the same patient at the same time for different reasons. The majority of intraoperative strokes are due to the embolization of atherosclerotic material from the aorta and brachiocephalic vessels. This results from manipulation of the heart and major thoracic vasculature as well as from dislodgement of atheromas by shearing forces directed at the walls of vessels from inflow CPB cannulas.26 Microemboli are distributed in proportion to blood flow27; thus, reduced cerebral blood flow reduces microembolic injury but increases the risk of hypoperfusion.28 During CPB, both alpha-stat acid-base management and phenylephrine reduce cerebral injury in adults, probably by causing cerebral vessel vasoconstriction and reducing the number of microemboli.28,29 Air,30 atherosclerotic debris,31 and fat are the major types of microemboli causing brain injury in clinical practice, and all cause neuronal necrosis by blocking cerebral vessels.32 Massive air embolism causes a large ischemic injury, but gaseous cerebral microemboli may directly damage endothelium in addition to blocking blood flow.33 The identification of unique small capillary arteriolar dilations in the brain associated with fat emboli (Fig. 65-2)34 raises the possibility that these emboli not only block small vessels but also release cytotoxic free radicals, which may significantly increase the damage to lipid-rich neurons.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree