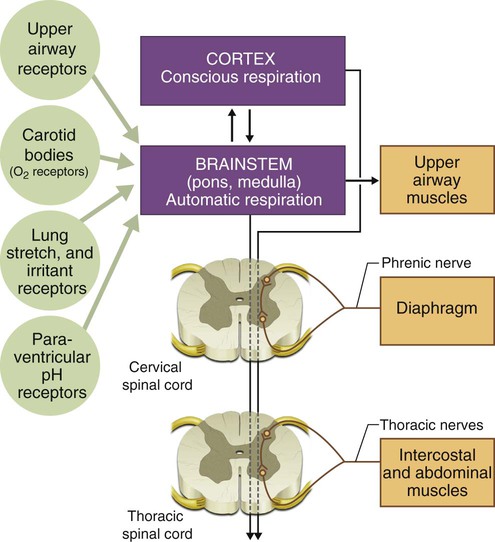
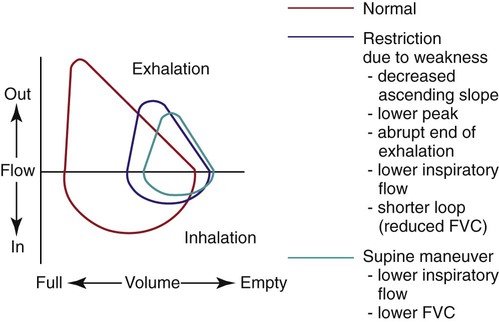
The respiratory system comprises the lungs, which provide an interface between inhaled air and circulating blood, mediating gas exchange; the thoracic cage, which forms the structure of the ventilatory pump; and the muscles of respiration, which are linked to respiratory centers in the brainstem by nerves exiting the spinal column and whose action on the thoracic cage produces movement of air into and out of the lungs. Understanding the interactions between these components is essential to understanding how their dysfunction leads to disease. The neuromuscular organization of the components of the respiratory system is shown in Figure 29-1. Maintenance of normal ventilation depends critically on intact, functional components of the neuromuscular system, which contribute to breathing in three principal ways: (1) regulation of respiratory drive and rate, (2) control of the mechanics of ventilation, and (3) cough and other airway protection. Diseases that affect the brain, nerves, muscles, or thoracic cage can lead to respiratory failure or hypoxemia even if the lungs are normal. The pulmonary consequences of neuromuscular disease include the following: 1. Dysregulation of respiratory drive or rate 2. Loss of strength or control of the mechanics of breathing • Respiratory failure owing to excessive work of breathing • Atelectasis leading to hypoxemia • Secondary effects of chronic hypoxemia (e.g., cor pulmonale, pulmonary hypertension) 3. Loss of strength or control of the muscles that produce cough and protect the airway Some systemic diseases that affect the neuromuscular system also cause interstitial lung disease, which can lead to considerable respiratory dysfunction (see Chapter 24). Respiratory failure, often associated with pulmonary infection, is a frequent cause of death in patients with neuromuscular disorders. A thorough understanding of the physiology of ventilation and chest wall mechanics (see Chapters 10 and 18) is needed to help the reader understand how abnormalities of the upper airway, chest wall, diaphragm, and abdominal muscles cause disease. This chapter reviews major disorders of the neuromuscular and skeletal systems that affect breathing. Disorders are grouped according to which functional unit of the neuromuscular system is affected, focusing on pulmonary manifestations of these disease processes (Table 29-1). TABLE 29-1 Locations at Which Several Neuromuscular Diseases Affect the Respiratory System *A category of systemic diseases that can affect neuromuscular function. Weakness of the respiratory muscles leads to the inability to generate or maintain normal respiratory pressures. Pulmonary function testing in patients with neuromuscular weakness typically reveals a restrictive ventilatory defect even if the lungs are normal. Vital capacity (VC), forced expiratory volume in 1 second (FEV1), and total lung capacity (TLC) are decreased. Residual volume (RV) is normal or decreased, and diffusing capacity corrected for alveolar volume is normal or near-normal but has been reported to be decreased.1 Comparison of spirometric results obtained with the patient in seated and supine positions can be useful in showing that orthopnea is caused by neuromuscular weakness. A decrease in VC or FEV1 of greater than 20% when a patient moves from the seated to the supine position suggests diaphragmatic weakness (Table 29-2 and Figure 29-2). The inability to generate normal respiratory pressures is reflected in a decreased maximal inspiratory pressure (PImax). Expiratory muscle weakness is characterized by a decreased maximal expiratory pressure (PEmax). TABLE 29-2 Pulmonary Function Testing Results from a Patient With Profound Diaphragm Weakness Arterial blood gases in the setting of a rapid, shallow breathing pattern may show a decreased PaCO2, although progressive inspiratory muscle weakness leads to hypoventilation and hypercapnia. Hypoxemia can occur in patients unable to take deep breaths and may be caused by microatelectasis, which leads to ventilation/perfusion mismatching within the lung and a resulting decrease in PaO2 (Figure 29-3). Chronic hypoxemia in this situation may be protective against acute respiratory muscle failure. Experimental data suggest that when hypoxemia is chronic, it may increase diaphragm muscle endurance.2 Hypoventilation that occurs with progressive neuromuscular disease may be a protective mechanism that avoids acute respiratory muscle fatigue. However, when hypoxemia is acute, it potentiates respiratory muscle fatigue, hastening respiratory failure.3 In the early stages of neuromuscular disease, patients with respiratory muscle weakness initially report exertional dyspnea and fatigue. As the disease process progresses, patients may complain of orthopnea or symptoms of cor pulmonale. These symptoms occur because the muscles involved with respiration can no longer generate or maintain normal ventilation. The response to hypoxemia and respiratory drive, measured with airway occlusion pressure (P0.1), is preserved in most patients with neuromuscular weakness.4 Because these patients do not have the strength to take deep breaths, they increase minute ventilation by increasing respiratory rate and adopting a rapid, shallow breathing pattern, which uses less respiratory muscle strength but provides less efficient ventilation. Patients with poor inspiratory muscle function (especially diaphragm weakness) may have marked orthopnea and prefer to sleep in a seated position. They may also experience a decline in the volume and power of voice or voice quality. Progressive muscle weakness can progress to the point where adequate ventilation is no longer maintained, and hypercapnia occurs. Monitoring the ventilatory function of a patient with neuromuscular weakness can involve repeated measurement of inspiratory pressure, VC, and arterial blood gas values. Depending on the condition, the need for mechanical support can be signaled by reaching either a critical value on testing or an overall clinical condition that does not allow unassisted ventilation to continue. Additional measurements that have been suggested to be more indicative of early respiratory insufficiency, at least in amyotrophic lateral sclerosis (ALS), include maximal sniff nasal inspiratory force5 and nocturnal oximetry.6 At least two caveats to this general approach should be mentioned. First, patients with myasthenia gravis having an acute myasthenic crisis may have normal test results within minutes of acute ventilatory failure because of the nature of the disorder.7 Second, the need to protect the upper airway from secretions and aspiration may not be clearly reflected in results of pulmonary function tests, which evaluate only the mechanical function of the ventilatory pump. Neuromuscular weakness may not manifest uniformly in all muscle groups. Ventilation may be only moderately reduced in patients with gross oropharyngeal dysfunction leading to aspiration. Patients with ventilatory weakness can have a high risk of acute respiratory failure if upper respiratory tract infection or pneumonia develops. In these patients, inability to clear secretions can increase the work of breathing; the results are muscle fatigue, hypoventilation, and acute respiratory failure. Respiratory insufficiency and failure to clear secretions are the major consequences of inspiratory and expiratory muscle weakness. Treatment of these patients involves consideration of mechanical ventilation via face mask or other noninvasive interfaces or via tracheostomy. Although often overlooked, therapies to augment secretion clearance and assist with cough are important in these patients (see Chapters 39 and 40). Used together, these interventions can decrease hospitalizations secondary to respiratory complications in patients with neuromuscular disease.8 These measures may also be useful in delaying or preventing the need for intubation or tracheostomy, although severe bulbar muscle weakness may limit a patient’s ability to avoid invasive ventilatory support.9 In addition to these interventions, general rehabilitation focusing on aerobic conditioning, muscle strengthening, and respiratory muscle training can often delay the need for ventilatory support and improve the overall quality of life for patients with muscle weakness.10 Noninvasive ventilation is being used increasingly for short-term and intermittent ventilatory support of patients with neuromuscular disease.11 Acute deterioration, such as during a pneumonia, and surgical procedures such as gastrostomy tube insertion are situations where noninvasive ventilation is safe and effective if used carefully.9,12 If a patient needs long-term ventilatory support on an intermittent basis, such as at night only, noninvasive ventilation may be appropriate.13 Decisions to begin mechanical ventilation in some patients with neuromuscular weakness have varied greatly among physicians14 and may be motivated by many different patient factors.15 No uniform guidelines exist for the use of long-term mechanical ventilation for patients with neuromuscular weakness. However, it is considered a standard option for patients who have reached the point of respiratory failure. Starting a patient on long-term mechanical ventilation requires careful planning and consideration of various issues related to respiratory care in alternative settings. These issues have been addressed in consensus statements16,17 and are discussed in Chapter 51. Diaphragm pacing in patients with spinal cord injury has been described for some time using direct stimulation of an intact phrenic nerve to contract the diaphragm and produce negative intrathoracic pressure and inspiration.18 This technique usually requires a thoracotomy, with its associated risks and high cost, and carries some risk of phrenic nerve injury. These objections have led to the development of an alternative system for diaphragm pacing using direct pacing of the diaphragm employing intramuscular electrodes implanted laparoscopically.19 When the electrodes can be placed in the diaphragm muscle at an electrophysiologically mapped motor point, the result is often elimination of the need for mechanical ventilation in patients with spinal cord injury and delay in the need to start mechanical ventilation in patients with ALS and other neuromuscular diseases.20 Primary muscle disease can decrease the ability of a normal neural impulse to generate effective muscle contraction. Some commonly recognized myopathies include Duchenne muscular dystrophy (DMD), myotonic dystrophy, and polymyositis. Table 29-3 presents a more complete list of myopathic diseases associated with ventilatory dysfunction. TABLE 29-3 Myopathic Diseases With Associated Respiratory Dysfunction Duchenne muscular dystrophy (DMD) is a genetic muscle-wasting disorder caused by mutations in the dystrophin gene.21 Because it is an X-linked recessive disorder, it affects mostly males. The diagnosis is made when a dystrophin mutation is found in DNA from peripheral white blood cells or when dystrophin is found to be absent or abnormal in muscle biopsy tissue. Progressive scoliosis is associated with DMD and can contribute further to respiratory insufficiency. Many patients undergo spine fusion surgery, and often the procedure allows greater comfort and ease in maintaining an upright posture. Although no randomized trials have proven any benefit of surgery on pulmonary function,22 observational data suggest that the rate of respiratory decline is slower after fusion surgery.23 Obstructive sleep apnea has been described in a significant proportion of patients with DMD, prompting some authors to recommend formal polysomnography in patients with symptoms of obstructive sleep apnea or at the stage of becoming wheelchair-bound.24 Institution of positive pressure ventilation (PPV) is a decision most patients face at some point in the disease. The point at which to begin different stages of ventilatory support depends on both test results and clinical condition. Nocturnal PPV is usually indicated when FVC reaches 30% of predicted with signs of hypoventilation.25,26
Neuromuscular and Other Diseases of the Chest Wall
 Identify pulmonary function test results seen in patients with neuromuscular disease.
Identify pulmonary function test results seen in patients with neuromuscular disease.
 List the potential respiratory complications associated with neuromuscular disease.
List the potential respiratory complications associated with neuromuscular disease.
 Identify the clinical signs and symptoms associated with respiratory muscle weakness.
Identify the clinical signs and symptoms associated with respiratory muscle weakness.
 Describe techniques for monitoring patients with respiratory muscle weakness.
Describe techniques for monitoring patients with respiratory muscle weakness.
 Describe general respiratory care management of patients with respiratory muscle weakness.
Describe general respiratory care management of patients with respiratory muscle weakness.
 Describe the clinical findings and treatment for each of the following neuromuscular disorders: Duchenne muscular dystrophy, myotonic dystrophy, polymyositis, myasthenia gravis, Lambert-Eaton syndrome, Guillain-Barré syndrome, unilateral diaphragmatic paralysis, amyotrophic lateral sclerosis, critical illness myopathy and polyneuropathy, spinal cord injury, stroke, traumatic brain injury, kyphoscoliosis, and flail chest.
Describe the clinical findings and treatment for each of the following neuromuscular disorders: Duchenne muscular dystrophy, myotonic dystrophy, polymyositis, myasthenia gravis, Lambert-Eaton syndrome, Guillain-Barré syndrome, unilateral diaphragmatic paralysis, amyotrophic lateral sclerosis, critical illness myopathy and polyneuropathy, spinal cord injury, stroke, traumatic brain injury, kyphoscoliosis, and flail chest.
Location
Disease
Cortex and upper motor neurons
Stroke, traumatic brain injury
Spinal cord
Trauma, transverse myelitis, multiple sclerosis
Anterior horn cells (lower motor neurons)
ALS, spinal muscular atrophy, poliomyelitis and postpoliomyelitis
Peripheral nerves
GBS, critical illness polyneuropathy, Lyme disease
Neuromuscular junction
MG, LES, botulism
Muscle
DMD, polymyositis, acid maltase deficiency
Interstitial lung disease*
Polymyositis, dermatomyositis, tuberous sclerosis, neurofibromatosis
General Principles Relating To Neuromuscular Weakness Of The Ventilatory Muscles
Pathophysiology and Pulmonary Function Testing
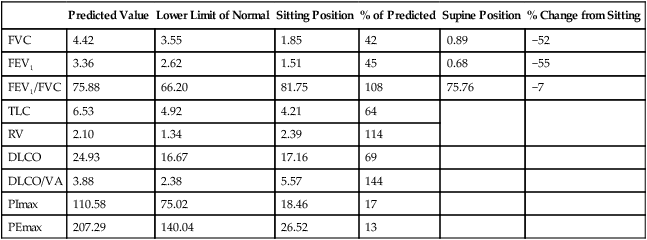
Predicted Value
Lower Limit of Normal
Sitting Position
% of Predicted
Supine Position
% Change from Sitting
FVC
4.42
3.55
1.85
42
0.89
−52
FEV1
3.36
2.62
1.51
45
0.68
−55
FEV1/FVC
75.88
66.20
81.75
108
75.76
−7
TLC
6.53
4.92
4.21
64
RV
2.10
1.34
2.39
114
DLCO
24.93
16.67
17.16
69
DLCO/VA
3.88
2.38
5.57
144
PImax
110.58
75.02
18.46
17
PEmax
207.29
140.04
26.52
13
Clinical Signs and Symptoms
Monitoring and Assessing Patients With Muscle Weakness for Respiratory Insufficiency
Management of Respiratory Muscle Weakness
Specific Neuromuscular Diseases
Disorders of the Muscle (Myopathic Disease)
Muscular Dystrophies
Myopathies
DMD
Congenital myopathies
Myotonic dystrophy
Nemaline rod myopathy
Facioscapulohumeral muscular dystrophy
Centronuclear myopathy
Limb-girdle dystrophy
Metabolic myopathies
Oculopharyngeal dystrophy
Acid maltase deficiency
Mitochondrial myopathies (Kearns-Sayre syndrome)
Inflammatory myopathies
Polymyositis
Dermatomyositis
Hypothyroid-related and hyperthyroid-related myopathies
Endocrine myopathies
Steroid-induced myopathies (including critical illness myopathy)
Miscellaneous myopathies
Electrolyte disorders (e.g., hypophosphatemia, hypokalemia)
Rhabdomyolysis
Periodic paralysis
Postneuromuscular blockade myopathy
Duchenne Muscular Dystrophy and Becker Muscular Dystrophy
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Neuromuscular and Other Diseases of the Chest Wall

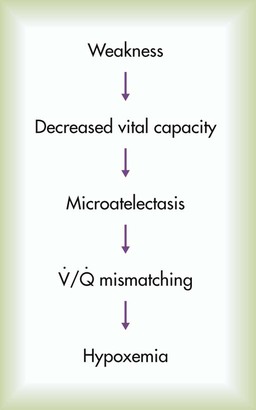
 , Ventilation/perfusion.
, Ventilation/perfusion.