Neurogenic Structures of the Mediastinum
Thomas W. Shields
Phrenic and Vagus Nerves
Phrenic Nerves
The phrenic nerve on the right lies on the medial border of the anterior scalene muscle and enters the thoracic inlet as it continues with the anterior scalene muscle between the subclavian vein and artery. It crosses the origin of the internal mammary artery and is joined by the pericardiacophrenic branch of the artery. According to a study by Owens and coworkers,13 there is no constant relationship between the phrenic nerve and the internal mammary artery on right or left sides as these structures cross behind the first rib. The vessel may be anterior or posterior to the nerve in any individual. These structures pass caudally over the cupula of the pleura on the lateral surface of the superior vena cava. In its caudad descent, the phrenic nerve passes ventrally to the hilar structures. The nerve lies deeper and has a more vertical course than the left nerve as it passes along the lateral aspect of the pericardium between the pericardium and the mediastinal surface of the pleura. Just above the diaphragm, it divides into two or more terminal trunks.
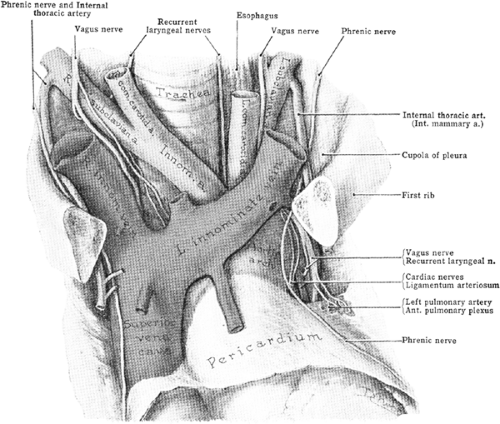
The left phrenic nerve is longer than the right. In the root of the neck, it is crossed by the thoracic duct, and in the upper portion of the visceral compartment, it lies between the left common carotid and subclavian arteries. The left phrenic nerve lies behind the left innominate vein lateral to the vagus nerve (Fig. 165-1). As the nerve crosses down, it moves ventrally; in the region where the left superior intercostal vein joins the left innominate vein, it comes to lie medial and anterior to the vagus nerve as these two nerves cross over the aortic arch. As on the right, the left phrenic nerve lies ventral to the hilum of the lung; except for its longer route, its remaining course and relationship to the pericardium are the same as on the right.
Vagus Nerves
The right vagus nerve enters the thoracic inlet within the carotid sheath between the internal jugular vein ventrally and the common carotid artery dorsally. It crosses the first part of the right subclavian artery. Here it gives off the right recurrent nerve; this branch loops under the arch of this vessel and passes dorsal to it, traveling to the tracheoesophageal groove and upward to the larynx. Caudally, the main descending trunk comes to lie on the right side of the trachea and passes dorsal to the pulmonary hilum. The trunk forms the posterior pulmonary plexus, and below this, it forms a plexus of nerve fibers on the dorsal aspect of the esophagus. After receiving branches from the left vagus, it forms a single trunk, the posterior vagus nerve, and lies slightly dorsal away from the wall of the esophagus before passing through the esophageal hiatus to enter the abdomen.
The left vagus nerve enters the thorax between the left carotid and subclavian arteries deep to the left innominate vein. It comes over the dorsal aspect of the left side of the aortic arch angling somewhat dorsally in its caudad descent. It passes between the aorta and left pulmonary artery just distal to the ligamentum arteriosum. At this site, it gives off the left recurrent branch, which loops from in front to behind the arch to lie on the side of the trachea (Fig. 165-2). The recurrent nerve then passes upward in the tracheoesophageal groove to the neck. As on the right, the major trunk of the left vagus passes dorsally to the pulmonary hilus where the nerve flattens out into the posterior pulmonary plexus. It reaches the esophagus as a variable number of smaller trunks, which lie on the ventral aspect of the esophageal wall. After receiving branches from the right vagus, these branches form a single trunk, which is closely applied to the esophagus as it passes through the diaphragmatic hiatus into the abdomen. From there, it continues onto the stomach, distributing branches over its anterosuperior surface. Some of these extend over the fundus, and others along the lesser curvature. Filaments from these branches enter the lesser omentum and join the hepatic plexus.
Spinal Nerves and Sympathetic Trunks
Each nerve emerges from the vertebral canal through the intervertebral foramen below the corresponding vertebra. Each nerve is in relation to the spinal rami of the artery and vein for the respective foramen. Essentially, the spinal nerve, as it leaves the vertebral foramen, divides into four branches: (a) posterior primary division (ramus posterior); (b) anterior primary division (ramus anterior); (c) ramus communicans, by which
it connects to the sympathetic trunk; and (d) a smaller ramus meningeus, which returns to the spinal canal. The anterior ramus runs laterally and is joined by the respective intercostal artery and vein to run in the groove on the undersurface of each rib.
it connects to the sympathetic trunk; and (d) a smaller ramus meningeus, which returns to the spinal canal. The anterior ramus runs laterally and is joined by the respective intercostal artery and vein to run in the groove on the undersurface of each rib.
The thoracic sympathetic trunk is made up of a variable number of ganglia connected by the sympathetic trunk, which lies ventral to the heads of the first through tenth ribs, at which site it passes more ventrally to lie on the bodies of the lower two thoracic vertebrae. Above, the sympathetic trunk is continuous with the cervical trunk and posterior to the vertebral artery; inferiorly, it passes out of the thorax just posterior to the medial lumbocostal arch. The trunk is external to the costal pleura and crosses ventrally to the aortic intercostal arteries.
The number of ganglia in the thoracic chain is variable, usually 10 or 11. The first thoracic ganglion is frequently fused with the inferior cervical ganglion, forming the “stellate ganglion.” The location of the ganglia may vary. They may lie on the heads of the ribs, the costovertebral articulation, or even the bodies of the vertebrae. Each ganglion receives a white ramus communicans from the respective thoracic nerve and gives off a gray ramus communicans to the same nerve.
With the increase of interest in and the performance of thoracic sympathectomy by the video-assisted thoracic surgery (VATS) approach for the management of craniofacial, palmar, and axillary hyperhidrosis, the anatomic variations in the origin and branching of the second thoracic nerve root—including the nerve of Kuntz and the adjacent structures of the sympathetic
trunk—have become important to those surgeons who perform upper sympathectomy for the various manifestations of hyperhidrosis. Chung and associates3 dissected the upper sympathetic trunk and upper symphathetic ganglia in 39 adult cadavers—bilaterally in 27 and on one side in 12 for a total of 66 dissections. The dissections were centered on the anatomy of the intrathoracic nerve of Kuntz (INK). This nerve is an inconsistent intrathoracic ramus described by Kuntz8 in 1927 connecting the first and second thoracic nerves. Chung and colleagues3 identified an INK in 68.2% of the specimens; it was present bilaterally in 48.1% of the bilateral dissection group. These authors classified the INK into four types according to its connection to the adjacent nerves: (a) type A, connecting from the T2 to the T1 nerve (47%); (b) type B, connecting from the T2 to the first intercostal nerve (12.1%); (c) type C, connecting from the T2 nerve to ramus communicans between the stellate ganglion and the T1 nerve (7.6%); and (d) type D, the nerve branching and connecting from the T2 nerve to the T1 nerve and the first intercostal nerve (1.5%) (Figs. 165-3 and 165-4). Twenty-one slides did not have a demonstrable INK but had a ramus communicans connecting from the T2 nerve to the stellate ganglion. Any ascending connection was absent in 7.6% of specimens, and an INK was noted connecting the T2 and T3 nerves in 7.6%. The location of the T2 sympathetic ganglion was most frequently located in (a) the second intercostal space (50%), followed in decreasing frequency by (b) the upper border of the third rib, (c) elongated from the second to the third rib where the T2 ganglion seemed to be fused to the stellate ganglion, (d) the lower border of the second rib, and (e) from the second to the third intercostal space over the entire width of the third rib, where the second (T2) sympathetic ganglion appeared to be fused with the T3 sympathetic ganglion. In 7.6% of the specimens, Chung and associates3 could not identify a T2 sympathetic ganglion. The importance and significance of the location and the necessity of division of INK for a successful sympathectomy (the dissection needs to be extended at least 1.5 cm laterally from the sympathetic trunk) were discussed in detail by Chung and colleagues.3
trunk—have become important to those surgeons who perform upper sympathectomy for the various manifestations of hyperhidrosis. Chung and associates3 dissected the upper sympathetic trunk and upper symphathetic ganglia in 39 adult cadavers—bilaterally in 27 and on one side in 12 for a total of 66 dissections. The dissections were centered on the anatomy of the intrathoracic nerve of Kuntz (INK). This nerve is an inconsistent intrathoracic ramus described by Kuntz8 in 1927 connecting the first and second thoracic nerves. Chung and colleagues3 identified an INK in 68.2% of the specimens; it was present bilaterally in 48.1% of the bilateral dissection group. These authors classified the INK into four types according to its connection to the adjacent nerves: (a) type A, connecting from the T2 to the T1 nerve (47%); (b) type B, connecting from the T2 to the first intercostal nerve (12.1%); (c) type C, connecting from the T2 nerve to ramus communicans between the stellate ganglion and the T1 nerve (7.6%); and (d) type D, the nerve branching and connecting from the T2 nerve to the T1 nerve and the first intercostal nerve (1.5%) (Figs. 165-3 and 165-4). Twenty-one slides did not have a demonstrable INK but had a ramus communicans connecting from the T2 nerve to the stellate ganglion. Any ascending connection was absent in 7.6% of specimens, and an INK was noted connecting the T2 and T3 nerves in 7.6%. The location of the T2 sympathetic ganglion was most frequently located in (a) the second intercostal space (50%), followed in decreasing frequency by (b) the upper border of the third rib, (c) elongated from the second to the third rib where the T2 ganglion seemed to be fused to the stellate ganglion, (d) the lower border of the second rib, and (e) from the second to the third intercostal space over the entire width of the third rib, where the second (T2) sympathetic ganglion appeared to be fused with the T3 sympathetic ganglion. In 7.6% of the specimens, Chung and associates3 could not identify a T2 sympathetic ganglion. The importance and significance of the location and the necessity of division of INK for a successful sympathectomy (the dissection needs to be extended at least 1.5 cm laterally from the sympathetic trunk) were discussed in detail by Chung and colleagues.3
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree