Fig. 41.2 (a) Approach to diagnosing narrow complex tachycardias. (b) Pathways taken by common supraventricular tachycardias.
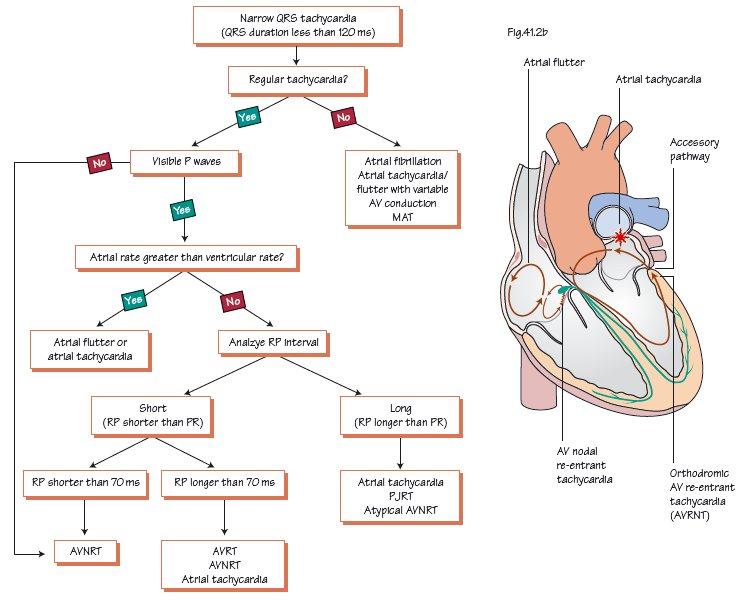
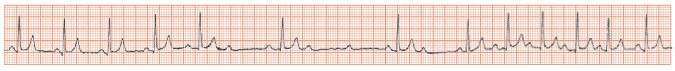
Fig. 41.3 Intravenous (IV) adenosine inducing transient atrioventricular (AV) block. A bolus (2–18 mg) of IV adenosine has been given. Sinus rhythm is present for 5 beats, then a P wave occurs without a QRS complex – heart block has occurred, initially 2:1, then 3:1, then 2:1. After a few seconds the adenosine wears off, and sinus rhythm (often slightly faster than before, as here) is re-established. When giving adenosine, start at a low dose, 3 mg, then work up to a high dose (18–24 mg). Stop when AV block has been induced, the arrhythmia terminated, or side-effects (flushing, breathlessness, chest pain) become troublesome.
In diagnosing narrow complex tachycardias, the first objective is to decide whether the rhythm is sinus or a tachyarrhythmia (Table 41.1). The key to this, as in any arrhythmia, is to determine the relationship of the P wave to the QRS complex. In particular:
- How many P waves to each QRS complex?
- If there are more P waves than there are QRS complexes (and provided the QRS rate is fast, i.e. this is not pathological heart block), then the diagnosis is an atrial arrhythmia with a degree of ‘physiological block’. What is this? Many atrial arrhythmias beat at rates of 200–300 per minute, and the normal AV node cannot repolarize fast enough to allow this number of impulses to the ventricle. The AV node will then often let every second or third beat through, resulting in the QRS rate being half or one third of the atrial rate. This is physiological block, a finding that does not imply any pathological damage to the conducting tissue of the heart. Arrhythmias with organized atrial beats, and so similar shaped P waves, include atrial flutter, and atrial tachycardia.
- If the ratio of P waves to QRS complexes is 1 to 1, next ascertain whether the P wave precedes or follows the QRS? If the P wave precedes the QRS complex (i.e. the PR interval is short, and conversely the RP interval is long), then the diagnosis is usually sinus tachycardia (Table 41.2). If the P wave closely follows the QRS complex (i.e. the RP interval is short, and conversely the PR interval is long), then the diagnosis is usually an arrhythmia (very rarely sinus rhythm with a very long PR interval gives rise to this pattern). If the P wave follows very close indeed to the QRS complex (Figs 45.2c and d), then the diagnosis is usually atrioventricular nodal re-entrant tachycardia (AVNRT); if the P wave is quite distinct, and occurs within the T wave, usually the diagnosis is atrioventricular re-entrant tachycardia (AVRT).
- If the P waves cannot clearly be seen, either the rhythm is sinus, and the heart rate is so high that the P waves of one beat are buried in the T wave of the preceding beat, or, more likely, the P wave occurs simultaneously with the QRS complex, so hiding its appearance, as in most cases of AVNRT.
The accurate determination of this relationship allows one to diagnose whether an arrhythmia is present and its nature.
Sinus tachycardia
The key features pointing to sinus tachycardia are:
- The P waves are usually clearly visible; their shape is the same as normal rhythm.
- Usually there is an obvious illness (sepsis, hypovolaemia, thyrotoxicosis, drugs, etc.). If not, and the P wave is normally shaped, consider: (a) inappropriate sinus tachycardia due to sick sinus syndrome; (b) postural orthostatic tachycardia (PAT) syndrome; or (c) sinus node reentrant tachycardia (very rare).
- PR interval << RP interval, a ‘long RP’ tachycardia; most, not all, long RP tachycardias are sinus (Table 41.2 & Fig. 41.2

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


