, Judy W. Hung2 and Judy W. Hung3
(1)
Harvard Medical School Cardiology Division, Department of Medicine, Massachusetts General Hospital, Boston, MA, USA
(2)
Harvard Medical School, Boston, USA
(3)
Echocardiography, Cardiology Division, Department of Medicine, Massachusetts General Hospital, Boston, MA, USA
Abstract
Myocarditis is an acute or chronic inflammatory process of the heart, caused by a spectrum of infectious agents, toxins and drugs which results in injury to the cardiac myocytes and clinically manifests with cardiac dysfunction.
Abbreviations
ACE
Angiotensin converting enzyme
ARB
Angiotensin II receptor blocker
AV
Atrioventricular
CMR
Cardiac MRI
CP
Chest Pain
ECG
Electrocardiogram
ECMO
Extracorporeal Membrane Oxygenation
HAART
Highly Active Anti-Retroviral Therapy
HF
Heart failure
IABP
Intra-aortic balloon pump
IFN
Interferon
IL
Interleukin
LM
Lymphocytic myocarditis
LV
Left ventricular
LVAD
Left ventricular assist devices
LVEF
Left ventricular ejection fraction
MCS
Mechanical Circulatory Support
MI
Myocardial Infarction
PCR
Polymerase chain reaction
RV
Right Ventricle
STEMI
ST-elevation myocardial infarction
TNF
Tumor necrosis factor
VT
Ventricular tachycardia
Introduction
Myocarditis is an acute or chronic inflammatory process of the heart, caused by a spectrum of infectious agents, toxins and drugs which results in injury to the cardiac myocytes and clinically manifests with cardiac dysfunction.
See Chaps. 14 and 15 for more.
Incidence and Natural History of Myocarditis
True incidence in the community is unknown due to heterogeneity of clinical presentation. Estimates are from published trials and large case series. From US Myocarditis Treatment Trial, approximately 10 % of patients with recent-onset dilated cardiomyopathy met histologic criteria for myocarditis [1].
Natural history varies with underlying etiology and presenting symptoms.
For most adults with acute dilated cardiomyopathy due to myocarditis, ventricular function and clinical status typically improves with standard HF (HF) treatment, however, transition of acute myocarditis to dilated cardiomyopathy is seen in approximately 10–20 % of patients [2].
Five-year survival in acute myocarditis is about 60 % and is comparable to survival in patients with idiopathic dilated cardiomyopathy (DCM) without myocarditis [3]. Giant Cell Myocarditis is associated with 5-year transplant free survival less than 20 %.
Clinical findings such as syncope, bundle branch block and left ventricular ejection fraction (LVEF) <40 % at presentation have been associated with increased risk of death or cardiac transplantation in case series.
Paradoxically, presentation with fulminant myocarditis -severe acute HF complicated by significant hemodynamic compromise and requiring inotropic or mechanical circulatory support – is associated with increased likelihood of recovery, if they survive the acute disease [3]
In patients with acute or fulminant myocarditis complicated by arrhythmia (sustained or symptomatic ventricular tachycardia [VT] or high degree atrioventricular [AV] block) or failure to respond to standard HF management, endomyocardial biopsy may be indicated to rule out more specific forms of myocarditis such as giant cell myocarditis.
Classification of Myocarditis (Table 20-1)
Table 20-1
Comprehensive classification of myocarditis
Causes | Viral, such as enteroviruses (e.g., Coxsackie B), erythroviruses (e.g., Parvovirus B19), adenoviruses, and herpes viruses |
Bacterial, such as Corynebacterium diphtheriae, Staphylococcus aureus, Borrelia burgdorferi, and Ehrlichia species | |
Protozoal, such as Babesia | |
Trypanosomal, such as Trypanosoma cruzi | |
Toxic: alcohol, radiation, chemicals (hydrocarbons and arsenic), and drugs, including doxorubicin | |
Hypersensitivity: sulphonamides and penicillins | |
Histology | Eosinophilic |
Giant cell | |
Granulomatous | |
Lymphocytic | |
Clinical presentation | Fulminant |
Acute | |
Chronic active | |
Chronic persistent |
Myocarditis can be classified on the basis of:
Causative organisms
Histology
Clinical presentation
Immunohistology
Pathogenesis/Etiology
Three stages of pathogenesis in viral myocarditis
1.
Acute myocarditis with viremia and a high fatality rate.
2.
Subacute myocarditis with lymphocytic infiltrates in the myocardium, increasing antibody titers and inflammatory cytokines such as interleukin (IL)-2, tumor necrosis factor (TNF)- α and interferon (IFN)-γ.
3.
Chronic myocarditis with fibrosis and progressive ventricular dilatation leading to a chronic dilated cardiomyopathy
Myocyte damage can also occur via interaction of viral genome with the host protein or directly via apoptosis in the absence of active inflammation (Fig. 20-1).
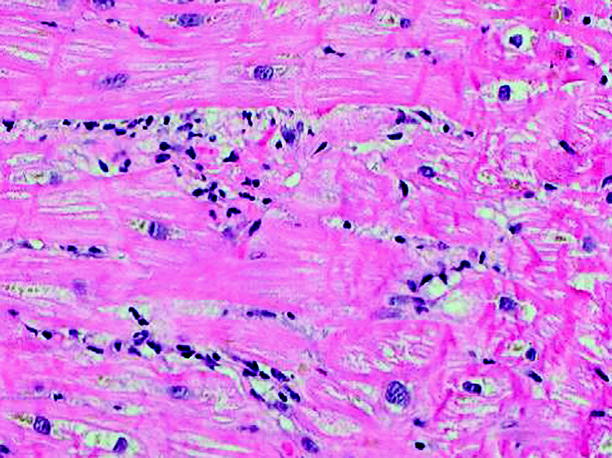
Figure 20-1
Lymphocyte rich infiltrate associated with myocardial necrosis in patient with acute myocarditis (Adapted from Sagar et al. [12])
Clinical Presentation and Diagnosis
A.
Clinical Presentation: there is a wide spectrum of clinical presentation in myocarditis.




Non-specific symptoms of dyspnea, chest pain (CP), or palpitations.< div class='tao-gold-member'>Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


