Low-density lipoprotein (LDL) is an important risk factor for coronary artery disease, but its localization within the human coronary arterial wall is poorly understood. Imaging of LDL in 30 coronary arteries excised from 15 subjects who underwent autopsy was performed using near-infrared fluorescent angioscopy system and using indocyanine green dye as a biomarker of LDL. The percentage incidence of LDL in 28 normal segments, 24 white plaques (early stage of plaque growth), and 21 yellow plaques (mature stage of plaque) classified by conventional angioscopy, was 14.2, 79.1 (p <0.01 vs normal segments and p <0.05 vs yellow plaques), and 28.5, respectively. Coronary near-infrared fluorescent angioscopy showed similar results in 7 patients in vivo. Our results suggested that LDL begins to deposit in the human coronary arterial wall in the early stage of atherosclerosis, increasingly deposits with plaque growth and decreases in the mature stage; and therefore, molecular therapy targeting LDL should be started before plaque maturation.
We have imaged native low-density lipoprotein (LDL) in excised human coronary plaques using color fluorescent angioscopy and nile blue dye as a biomarker of LDL, but because the dye is lipotrophic, intravascular administration in patients is not recommended. Our search for a biomarker of LDL that would be clinically applicable revealed indocyanine green dye (ICG) elicits near-infrared fluorescence (NIRF) characteristic of human LDL only. Therefore, in the present study, molecular imaging of native LDL in human coronary plaques by an NIRF angioscopy (NIRFA) system was performed using ICG as a biomarker of LDL ex vivo and in vivo.
Methods
The NIRFA system used in the present study is consisted of a fluorescence excitation unit, angioscope, fluorescence emission unit, and camera. The angioscope (modified VecMover; Clinical Supply Co, Gifu, Japan) consisted of a 2.5Fr fiberscope containing 6,000 quartz fibers for image guidance and 300 quartz fibers for light guidance. The fiberscope is incorporated in a 5Fr guiding balloon catheter and is steerable along a 0.014-inch guidewire, which enables observation of a coronary segment up to 7 cm in length after a single saline flush. This angioscope has been approved for clinical use on a commercial basis by the Japanese Ministry of Health and Labor, supported by National Insurance.
For NIRFA, the light guide of the angioscope is connected to a fluorescent exciter (developed in collaboration with Olympus). The light generated by mercury–xenon (Hg–Xe) lamp was irradiated through a bandpass filter (BPF) of 690 ± 20 nm onto the coronary luminal surface and the evoked NIRF was received by a chilled charge-coupled device camera (C5985; Hamamatsu Photonics, Hamamatsu, Japan) through a dichroic membrane which cuts out light waves <780 nm, and a band absorption filter (BAF) of 780 nm, which allows light waves >780 and <880 nm to pass through. This pair of BPF and BAF was used because we found by NIRF microscopy (NIRFM) that ICG elicits an NIRF of human LDL only and not that of other major substances comprising atherosclerotic plaques.
The obtained images were amplified by changing the sensitivity (stepwise from 0 to 10 when NIRF was weak) of the intensified charge-coupled device camera controller (C3510, Hamamatsu Photonics) and displayed on a video monitor while being recorded on a digital vesatile disc recorder. The NIRF intensity was arbitrarily defined as strong, moderate, weak, and absent when the sensitivity required for imaging was within 5, over 5 and within 7, over 7 and within 9, and over 9, respectively.
The ex vivo study was carried out with the approval of the ethical committees of the Japan Foundation for Cardiovascular Research, Tsukuba Memorial Hospital, Funabashi Futawa Hospital, and Toho University Medical Center and after obtaining written informed consent from the families concerned.
Thirty coronary arteries (15 left anterior descending arteries, 5 left circumflex arteries, and 10 right coronary arteries) were excised from 15 autopsied cases (62.5 ± 3 years of age, 4 women, 11 men; cause of death: acute myocardial infarction [3], diabetic nephropathy [3], cerebral infarction or bleeding [4], pancreatic carcinoma [2], hepatocellular carcinoma [1], gastric carcinoma [1], and pneumonia [1]).
A Y connector was introduced into the proximal portion of each coronary artery for perfusion with saline solution at a rate of 20 ml/min and then the angioscope was introduced through the connector into the artery for observation. Initially, conventional angioscopy (details were described elsewhere ) was carried out to detect plaques. As a result, 45 plaques (24 white plaques and 21 yellow plaques) and 28 normal segments were confirmed. Details of angioscopic classification of coronary plaques were described elsewhere.
After conventional angioscopy, the NIRFA system was set up; a BPF of 690 ± 20 nm and BAF of 780 nm were selected and a control image was obtained under saline perfusion. After ceasing the perfusion, 1 ml of 0.1% ICG solution was injected into the perfusion circuit and 5 minutes later the perfusion of saline solution was restarted and the target portion was observed again. Quantitative measurement is difficult with NIRFA because the target becomes a “fish eye” image through the lens attached to the angioscope’s tip.
The plaques and normal segments that were observed by conventional angioscopy and NIRFA were isolated by transecting the proximal and distal ends along the shorter axes. Next, the isolated plaques and normal segments were transected at the center into 2 parts 1 to 2 mm in width. One part was stored at −20 ○ C for immunohistochemical staining of LDL. The other part was mounted on a deck glass in such a way that the transected surface faced the glass for NIRFM scanning, and 0.1 ml of 10 −6 M ICG solution was dripped onto the specimen so that it diffused to the transected surface and stained LDL.
The frozen excised vessels were cut into 2 sections of 20 μm in thickness on a cryostat (Tissue Tec 3D; Sakura Finetek Japan, Tokyo). Next, the section adjacent to the part used for NIRFM was fixed with 4% paraformaldehyde solution and LDL was stained immunohistochemically with anti-LDL antibody (anti-LDL antibody ab157795, chicken polyclonal to LDL, which reacts with human LDL; Abcam Ltd, Tokyo, Japan). Similarly, M1-macrophages in a remaining section was stained using an anti-CD68 antibody (mouse monoclonal antibody NCL-CD68-KP1, react with human CD68, Vision Biosystems Novocastra, New Castle, United Kingdom). By this staining technique, LDL and M1-macrophages were stained brown. The obtained images were compared with the corresponding NIRFA and NIRFM images.
After obtaining written informed consent for NIRFA, 7 patients (aged 60.3 ± 2. 4 years; 1 woman, 6 men; 4 patients with stable angina pectoris and 3 patients with old myocardial infarction) underwent routine coronary angiography, then, conventional angioscopy followed by NIRFA of the left anterior and/or right coronary artery. Conventional angioscopic and NIRFA systems as described earlier were used for imaging. After conventional angioscopy, the light and image guide were connected to fluorescence excitation and emission units, respectively, without changing the location of the angioscope tip, and NIRFA was performed before and after selective intracoronary administration of 1 ml of 0.1% ICG solution. Details of NIRFA procedure were described elsewhere.
The data obtained were tested by chi-square formulae and were compared among different deposition sites, patterns, and plaque morphology. A value of p <0.05 was considered to be statistically significant.
Results
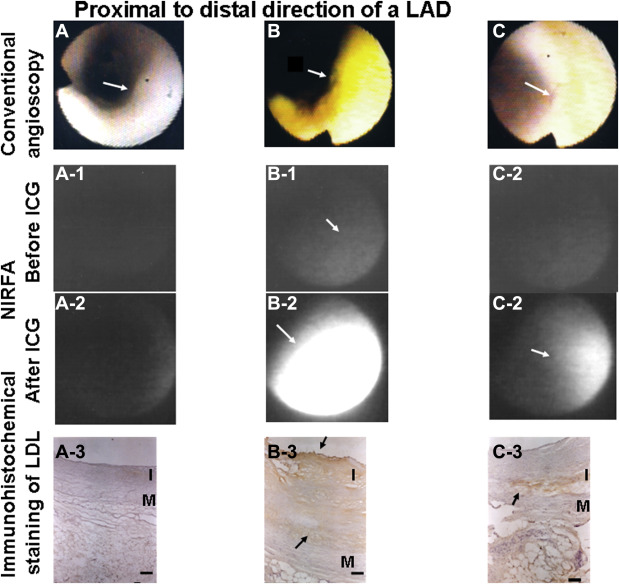
Figure 1 shows representative NIRFA images of LDL evoked by ICG and the relation to conventional angioscopic images and LDL stained by immunohistochemical staining in the corresponding plaques or normal segments. The presence or absence of LDL differed from plaque to plaque and between normal segments.
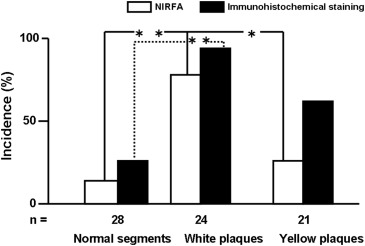
The percentage incidence of LDL in white plaques (early stage of plaque growth) was significantly higher than that of yellow plaques (matured stage of plaque) or normal segments classified by conventional angioscopy ( Figure 2 ). The percentage incidence of immunohistochemically stained LDL in the transected surface of white plaques was also higher than that in normal segments and showed a tendency to be higher than that in yellow plaques. Although statistically not significant, the percentage incidence of LDL visualized by NIRFA was lower than that with immunohistochemical staining ( Figure 2 ). The sensitivity and specificity of NIRFA for imaging LDL were 87.8% and 100%, respectively.
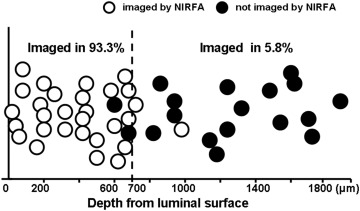
Compared with immunohistochemical staining, NIRFA could visualize LDL located within a depth of 700 μm from the luminal surface in most preparations but rarely that located beyond this depth ( Figure 3 ). As shown in Figures 4 and 5 , the localization of LDL in the transected surface of plaques visualized by NIRFM using ICG coincided with that on immunohistochemical staining in most preparations. The sensitivity and specificity of NIRFM for imaging LDL were 87.8% and 96.7%, respectively. LDL deposited diffusely in the intima, where M1-macrophages were not observed. In a few preparations, LDL showing dotty pattern was observed in the superficial layer of the intima where macrophages were observed (arrowheads in Figure 4 ).

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


