The benefits of chronic total coronary occlusion (CTO) revascularization are not well established. In this prospective cohort study, 47 consecutive patients with successful percutaneous recanalization of CTO underwent adenosine stress cardiac magnetic resonance (CMR), 6-minute walk test (6MWT), and the Short Form-36 Health Survey before and 6 months after the procedure. Successful recanalization of a CTO was followed by significant improvement of (1) global physical and mental health status; (2) the distance walked in the 6MWT; (3) the incidence of chest pain at the end of the 6MWT; and (4) the score of a novel CMR ischemic burden index on the basis of the characteristics of adenosine stress perfusion defects (extension, persistence, transmurality, and induced contractile regional dysfunction). Patients with greater CMR ischemic index before percutaneous revascularization showed better improvement in the 6MWT. In conclusion, successful recanalization of a CTO leads to a concurrent improvement in ischemic burden, exercise tolerance, angina frequency, and quality of life scores. Patients with a high ischemic CMR score before CTO recanalization showed the better improvement in exercise tolerance.
Current guidelines recommend percutaneous coronary intervention (PCI) of a chronic total coronary occlusion (CTO) when symptoms are present and there is evidence of significant ischemia and viable myocardium in the territory supplied by the occluded vessel. CTO revascularization has been found to improve global left ventricular (LV) function and regional wall motion, as well as viability and ischemic burden. Most of this parameters are increasingly measured by cardiac magnetic resonance (CMR), with special emphasis in the presence and extent of inducible ischemia. Despite the well-known improvement in these CMR parameters, the benefits of CTO revascularization on survival still remain controversial, and the potential improvement of symptoms, physical activity, and quality of life are even less studied. Thus, there is a growing need to understand whether a reduction in pre-PCI ischemic burden relates with a subsequent clinical improvement. This study was primarily addressed to evaluate the improvement of quality of life, functional status, and inducible myocardial ischemia assessed by adenosine stress CMR at 6 months after successful CTO percutaneous revascularization. In addition, we aimed to evaluate the relation between 4 pre-PCI ischemic CMR parameters and the patient clinical improvement after CTO recanalization.
Methods
Consecutive patients who underwent successful PCI of a CTO vessel from September 2012 to December 2013 were prospectively recruited. From 52 patients in whom percutaneous CTO recanalization had been attempted, success was observed in 47 patients (90.4%). The inclusion and exclusion criteria are detailed in Figure 1 . Of note, all patients included presented with angina and/or one of the following CMR criteria: (1) the presence of ischemia related to CTO and (2) the presence of myocardial viability at the segments of the target vessel, defined as <25% of contrast delayed-enhancement transmurality.
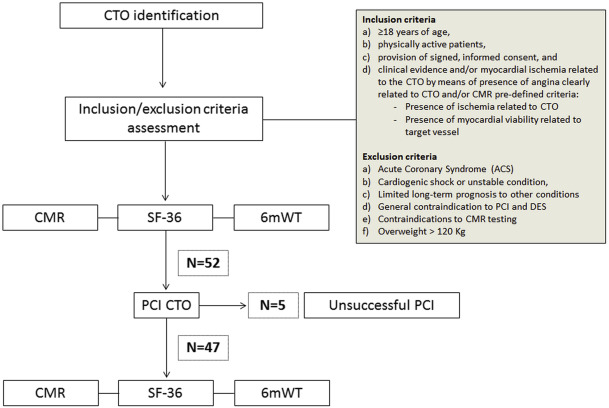
The study flow chart is also summarized in Figure 1 . Briefly, all patients underwent stress adenosine CMR imaging before PCI, and this study was repeated 6 months later. Quality of life and functional status were also assessed before and after PCI. The study was conducted in accordance with the standards set by the “Declaration of Helsinki,” and it was approved by the Clinical Research Ethics Committee at the Hospital de la Santa Creu i Sant Pau. Informed consent was obtained from all patients before starting the study protocol.
According to Euro-CTO criteria, CTO was defined as an occlusion existing for at least 3 months. The duration of the occlusion was verified by a previous angiogram showing the occluded vessel or, in its absence, on clinical data indicating the occurrence of a clinical ischemic event potentially related to the CTO. Acute procedural success was defined as the ability to cross the occluded segment with both a wire and balloon and successfully open the artery with a final in-stent residual stenosis <30% and TIMI flow 3 in the target vessel. All patients were treated with aspirin open-endedly and received heparin at the time of the procedure to achieve an activated clotting time of 250 to 350 seconds. Time of fluoroscopy and total volume of contrast administered were recorded.
A 6-minute walk test (6MWT) was performed in an indoor unobstructed 30-m long corridor, according to the American Thoracic Society guidelines. Patients were instructed to walk the corridor from one end to the other at their own pace, as many times as possible, in the permitted time. The patients were advised on the possibility of slowing down the pace and stopping or resting if needed. After 6 minutes had elapsed, patients were instructed to stop walking, and the total distance walked was measured. Baseline and postwalk vital signs were reported, as well as the presence of chest pain at the end of the test.
Quality of life was measured using the Short Form-36 Health Survey (SF-36). The SF-36 Health Survey is a patient-reported survey used to assess patient health status and monitoring and comparing disease burden. It consists of 36 questions grouped into 8 scaled domains, which are the weighted sums of the questions in their section. These domains are combined into 2 metascores, the physical component summary and the mental component summary, reflecting global physical and mental functioning. These 8 item domains and 2 metascores are ranged on a scale from 0 to 100, with higher scores indicating better functional status. According to previous publications, the normal range is between 40 and 60 and it has clinical relevance when a difference of at least 5 points between the baseline and post-PCI results is detected. Reference values in general population in our geographical area were reported previously by Lopez-Garcia et al.
All CMR studies were performed with a Philips Achieva 1.5 T scanner. Steady-state free precession cine MR images were acquired in long-axis planes and in multiple 8 mm-thick short-axis slices/2 mm gap from the atrioventricular groove to the LV apex.
Perfusion studies were performed using a balanced turbo field echo sequence in 3 short-axis slices (basal, mid, and apical levels). Image acquisition started after 4 minutes of adenosine infusion at 140 mcg/kg/min using gadolinium doses of 0.1 mmol/kg. Ten minutes after stress, rest perfusion imaging was performed repeating the same protocol. Also, cine MR images were obtained in the same 3 short-axis slices during stress and repeated at rest. A 3-dimensional inversion recovery segmented gradient echo sequence was acquired 10 minutes after contrast administration to assess delayed-enhancement. This sequence was used in multiple short-axis planes using the same orientation as the cine MR images. The study duration was 45 minutes.
Cine loops and contrast-enhanced images were assessed on dedicated software (QMass MR 7.1, Medis, Leiden, the Netherlands). Overall LV and necrotic mass, as well as LV ejection fraction were reported in each case. CMR perfusion images and their subsequent cine sequences were assessed during adenosine infusion and at rest, using the American Heart Association 17-segment model and excluding the apical segment. According to clinical practice, an inducible perfusion defect was considered if the signal intensity on stress perfusion images was reduced in at least 2 contiguous myocardial segments, for at least 3 dynamic images, compared with remote myocardium, and this was not present in the rest study.
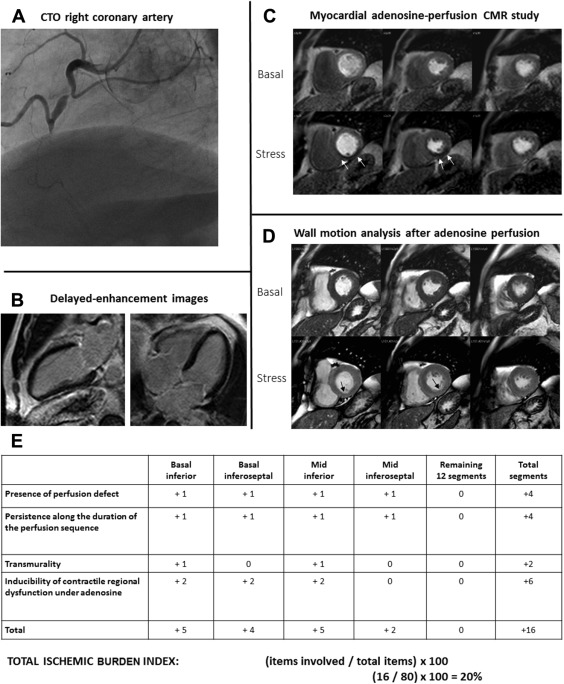
The ischemia was evaluated using 4 different parameters in each LV segment: (1) the presence of perfusion defect; (2) persistence of the defect along the duration of the perfusion sequence; (3) LV transmural extension of the defect; and (4) inducibility of regional contractililty dysfunction under adenosine perfusion. Moreover, we formulated an unexplored index of ischemic burden (IBI) based on the presence of the previously described 4 CMR parameters in each single LV segment. Each parameter was weighted with one point, except for the inducible contractile regional dysfunction parameter, to which we assigned 2 points considering that entails an advanced degree of inducible ischemia. Hence, each single LV segment may range between 0 and 5, and the whole 16-segment score may range between 0 and 80. A representative example of IBI assessment is shown in Figure 2 .
Continuous variables are presented as mean ± SD. Comparisons between before and 6-month after PCI CMRs, SF-36 and walked distance were performed by paired t tests. McNemar’s test was used to compare the presence of chest pain in pre-PCI and post-PCI 6MWT. The cohort was stratified into 2 groups using the median of the IBI on pre-PCI CMR to generate mild severity ischemia group (below the median) and a moderate–severe ischemia group (above the median). Paired t tests and McNemar’s test were separately carried out for comparisons in each of the group. A 2-tailed p <0.05 was considered statistically significant. All statistical tests were performed with IBM SPSS Statistics software, version.20.0, (IBM Corp., Armonk, New York).
Results
The baseline demographics for our cohort are summarized in Table 1 . The CTO vessel was the right coronary artery in 29 patients (61.7%), the left anterior descending coronary artery in 10 patients (21.3%), and the left circumflex coronary artery in 8 patients (17%). In regard to angiography, mean time of fluoroscopy was 70 ± 43.8 minutes and volume of contrast administered was 371 ± 139.9 ml.
| Variable | Overall population (n = 47) |
|---|---|
| Age (years) | 62 ± 10 |
| Men | 42 (89%) |
| Diabetes mellitus | 19 (40%) |
| Hypertension | 35 (75%) |
| Dyslipidemia | 36 (77%) |
| Smoker | 31 (66%) |
| Familiar history of coronary heart disease | 2 (4%) |
| Serum creatinine (>1.5 mg/dl) | 1 (2%) |
| Peripheral artery disease | 6 (13%) |
| Prior stroke | 1 (2%) |
| Prior myocardial infarction | 13 (28%) |
| Previous percutaneous coronary intervention | 15 (32%) |
| Previous coronary bypass | 2 (4%) |
Forty-three of all consecutive patients (91.5%) answered the SF-36 survey at baseline and 6-month follow-up. Score results for the 8 scales, as well as their changes from preprocedural scores are reported in Table 2 . At follow-up, patients showed an improvement in each item of the SF-36 survey compared with baseline situation, which was also reflected in global physical and mental functioning scores. Six items (physical functioning, role physical, general health, vitality, social functioning, and role emotional) showed a clinically relevant improvement, according to a threshold of 5. Conversely, the improvement in 2 items (Bodily Pain and Mental Health) was not of clinical relevance. CTO recanalization showed a positive clinical impact in terms of global physical health, but not in global mental health.
| Variable | Basal | 6 m post-PCI | P-value |
|---|---|---|---|
| Physical Functioning | 39±10 | 46±9 | <0.001 |
| Role-Physical | 39±13 | 47±12 | <0.001 |
| Bodily Pain | 42±11 | 47±10 | 0.015 |
| General Health | 40±9 | 45±10 | <0.001 |
| Vitality | 40±11 | 48±11 | <0.001 |
| Social Functioning | 37±14 | 43±13 | 0.003 |
| Role-Emotional | 39±15 | 45±14 | 0.005 |
| Mental Health | 44±12 | 48±12 | 0.018 |
| Global Physical Health | 39±10 | 46±9 | <0.001 |
| Global Mental Health | 41±16 | 46±14 | 0.029 |
Forty of all consecutive patients (85.1%) underwent 6MWT at baseline and 6-month follow-up. Vital signs, clinical data during the test and final walked distance are reported in Table 3 . No differences were found in vital signs at the end of the 6MWT in pre-PCI study compared with 6 months after PCI study, with the exception of the heart rate. However, after revascularization, patients showed a better physical activity performance (416.5 ± 125.71 vs 463.0 ± 102.61 m; p = 0.002), as well as a reduction in chest pain frequency (39% vs 8%; p <0.001).
| Variable | Basal | 6 m post-PCI | P-value |
|---|---|---|---|
| Systolic blood pressure (mm Hg) | 149±20 | 152±19 | 0.385 |
| Diastolic blood pressure (mm Hg) | 83±9 | 81±12 | 0.198 |
| Heart rate (bpm) | 74±12 | 79±13 | 0.030 |
| Oxygen Saturation by Pulse Oximetry (%) | 97±1 | 97±1 | 0.208 |
| Walked distance (meters) | 417±126 | 463±103 | 0.002 |
| Chest pain at the end of the test | 15 (39%) | 3 (8%) | <0.001 |
In all patients, a complete CMR study protocol could be performed. A total of 1,504 segments were available for perfusion analysis (16 segments × 47 patients × 2 CMR). Table 4 lists the comparison of CMR findings before and after PCI. All parameters measuring ischemia were significantly reduced. The IBI was also reduced 16 points (from 19% to 3%, p <0.001). Mean LV ejection fraction was normal before PCI and did not change significantly after PCI. There were no differences in the necrotic mass between the 2 studies.
| Variable | Basal | 6 m post-PCI | P-value |
|---|---|---|---|
| Necrotic mass (g) | 4.3±5.4 | 3.8±3.9 | 0.131 |
| Necrotic percentage (%) | 3.5±4.36 | 3.0±3.1 | 0.108 |
| Left ventricular ejection fraction (%) | 62±10 | 64±9 | 0.097 |
| Number of segments with perfusion defect (n, % of total segments) | 4.9±2.3 (31±14%) | 1.1±1.8 (7±11%) | <0.001 |
| Number of segments with persistent perfusion defect (n, % of total segments) | 1.7±1.6 (10±10%) | 0.3±0.7 (2±4%) | <0.001 |
| Number of segments with transmural perfusion defect (n, % of total segments) | 1.4±1.7 (9±11%) | 0.3±0.7 (2±4%) | <0.001 |
| Number of segments with inducible contractile dysfunction (n, % of total segments) | 1.6±1.8 (10±11%) | 0.2±0. (1±4%) | <0.001 |
| Ischemic burden index (%) | 19±10 | 3±6 | <0.001 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


