Fig. 33.2 ECG in a patient with mitral stenosis. Atrial fibrillation, with very coarse fibrillatory waves in lead V1 – these might be mistaken for an atrial tachycardia, but running one’s eye along the rhythm strip at the bottom, one can see that the fibrillatory waves change continuously in appearance, which would not be the case with an atrial tachycardia. The QRS response is irregular, another hallmark of atrial fibrillation. Normal axis, but dominant R wave in lead V1 (due to pulmonary hypertension).
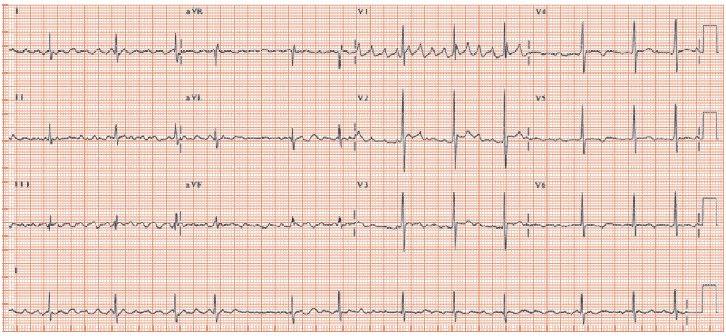
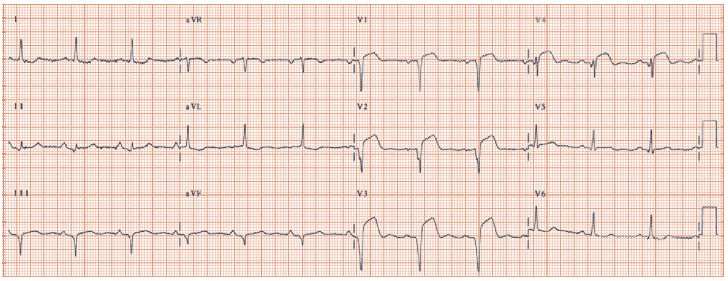
Fig. 33.3 Functional mitral regurgitation. Patient with old anterior wall myocardial infarction. Sinus rhythm, left atrial enlargement (prominent late negative deflection in lead V1 P wave). Q waves leads III, aVF and V1–4 (suggesting an left anterior descending [LAD] artery that ‘goes round the corner’, i.e. supplies some of the inferior wall). Persisting ST elevation in leads V1–4 suggest persisting occlusion of the infarct related artery, which increases the chance of finding a ventricular aneurysm.
Mitral regurgitation
Mitral regurgitation (MR) is by far the commonest valve lesion. There are two causes:
- Intrinsic disease of the mitral valve and its supporting apparatus (termed ‘organic’ MR). The common causes are: rheumatic heart disease, mitral valve prolapse, papillary muscle dysfunction or rupture due to myocardial infarction (MI). Connective tissue diseases (Marfan, Ehlers–Danlos syndrome) cause a few cases, bacterial endocarditis is a rare cause, systemic lupus erythematosus (SLE) a very rare cause. The ECG signs of organic MR are:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


