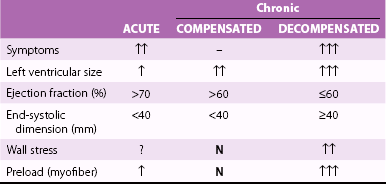
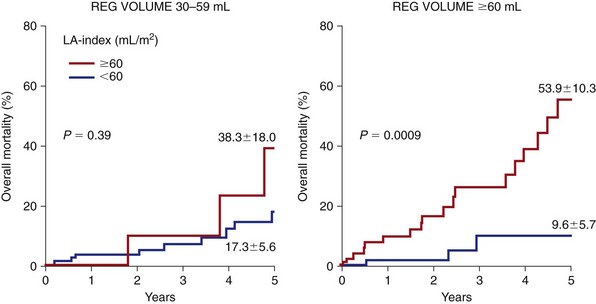
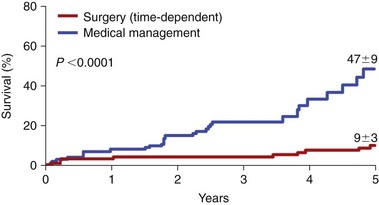
Chapter 20 The optimal timing for surgery for severe mitral regurgitation (MR) has been controversial.1–6 In the symptomatic patient with severe MR, relief of volume overload by mitral valve repair or replacement improves symptoms and functional status. 7 Thus, the primary indication for operation in a patient with severe MR has been the presence of severe symptoms. However, the natural history of severe MR is not benign, and surgical correction of MR in asymptomatic patients may improve survival and reduce risk of complications such as heart failure and atrial fibrillation. In the past, clinicians have been reluctant to subject asymptomatic patients with MR to operation owing to an in-hospital operative mortality and morbidity as well as potential long-term complications of a valve prosthesis. In current practice, however, severe MR due to degenerative disease can be repaired in more than 90% of patients with very low operative risk (<1% to 2%). It is well known that chronic volume overload may lead to irreversible left ventricular (LV) systolic dysfunction, and this systolic dysfunction can develop before the onset of symptoms.8–10 Once systolic dysfunction occurs, the outcome becomes poorer, whether or not operation is performed. Conventional measurements of LV function do not reliably predict the onset of LV dysfunction, owing to changes in load on the ventricle imposed by the MR.8,9,11,12 It is important, therefore, to identify and correct severe MR before irreversible LV dysfunction occurs.1,2 There have been advances in our knowledge, diagnosis, and treatment of MR. The pathophysiology of the volume overload on the left ventricle and its eventual outcome on LV function is now better understood.6,13 The natural history of severe MR has been clarified and elucidated by multiple centers.14–16 Echocardiography can now accurately assess the valve morphology and severity of the regurgitation noninvasively in most patients as well as determine the effect of the volume overload on the left ventricle. Current operative interventions have resulted in a much lower operative mortality and better long-term outcome than was possible several decades ago, with clear benefits of mitral valve repair over valve replacement.2,3,5,17,18 All of these advances have provided an incentive to change the indication for timing of operation in patients with MR, setting the paradigm of early operation before the onset LV dysfunction. This chapter outlines these advances and provide recommendations regarding optimal timing of surgery for MR. The diagnosis of severe MR is made when 50% of the total stroke volume is diverted to regurgitant flow. 13 Several general stages describe the hemodynamic response to the excessive volume overload of MR in terms of intrinsic LV myocardial as well as circulatory responses ( Table 20-1). These stages are (1) an acute volume overload stage, (2) a chronic compensated volume overloaded stage, and (3) the decompensated stage of MR with irreversible LV dysfunction.1,6,8,13,19,20 The short-term LV response to volume overload is an increase in LV volume from a lengthening of sarcomeres along their normal length tension curve so that total stroke volume increases via the Starling mechanism. 8 Fractional shortening of the left ventricle increases and end-systolic volume decreases as the result of the low resistance runoff into the low-pressure left atrium. There is thus a decrease in the integrated systolic wall tension. If forward cardiac output can be maintained by these compensatory mechanisms, and if LA pressure is lowered by therapy, an evolution from the acute to the chronic compensated stage of MR occurs.6,8,13,19,20 The major compensatory mechanism that occurs in this chronic steady state of MR is LV enlargement. LV dilation occurs from rearrangement of sarcomeres, added in series and parallel. 19 The individual sarcomeres are not extended beyond their optimal contractile length and, thus, the stretch (or preload) on the individual sarcomere is normalized. The increase in LV cavity size allows a greater LV volume as a result of the MR while maintaining normal diastolic pressures. Wall stress on the left ventricle depends on LV pressure, volume, and wall thickness. The initial unloading of the left ventricle by the low-resistance runoff into the left atrium is countered by an increase in LV size during this compensatory stage, returning systolic wall stress to normal levels.6,13 In this chronic compensated stage of MR, appropriate LV adaptation occurs by dilation with adequate forward cardiac output and maintenance of normal filling pressures. Patients remain asymptomatic during this state, and the normalized preload and wall stress help the left ventricle maintain normal contractility. Patients may remain in this chronic compensated stage for years to decades following the onset of MR.6,8,11,13,19 In patients with severe MR, there will eventually be progressive LV enlargement beyond that of a compensated stage.6,8,13,19–22 This progressive LV enlargement is due to increasing severity of MR, continued compensatory chamber enlargement, or a combination of both. Mitral valve competence is highly dependent on the integrated function of the entire mitral valve apparatus—the mitral annulus, papillary muscle orientation, chordae, and leaflets. Progressive LV enlargement itself can cause increasing degrees of MR from altered LV geometry and annular dilation; thus the saying “MR begets MR.” In degenerative MR, disruption of supporting structures such as rupture of chordae tendineae may occur, further increasing the severity of MR. As disease progresses, systolic wall stress on the left ventricle is increased as a result of increased circumferential stress from a larger LV minor axis as the left ventricle assumes a more spherical shape.8,11,12,20,22 An increase in end-diastolic stress occurs from further stretching of the myocytes beyond their normal contractile length, leading to an increase in end-diastolic pressure as the ventricle overfills. The effect of the continued abnormally elevated wall stresses on the ventricle is a decreased contractile state, with reduced myofiber content and interstitial fibrosis. The cumulative effects of prolonged oxidative stress with secondary lipofuscin accumulation and cardiomyocyte myofibrillar degeneration further account for LV contractile dysfunction. 23 As this process continues, irreversible LV dysfunction occurs, leading to the decompensated stage of MR. Once irreversible LV dysfunction is present, the prognosis is poor. Development of symptoms is an unreliable guide to the transition from the compensated to the uncompensated stage. By the time significant symptoms of dyspnea occur, there may already be significant irreversible dysfunction. The usual ejection phase indices of LV contractility may not reflect deterioration of LV systolic function, owing to the dependence of these indices on the load imposed on the left ventricle. Preload, afterload, and wall stress are abnormal and variable in patients with MR, and indices such as ejection fraction (EF) and fractional shortening may remain normal despite progressive decrease in contractile function of the left ventricle. Therefore, other parameters, such as preload-corrected EF, end-systolic wall stress normalized for end-systolic volume index, mass normalization of LV elastance, and end-systolic wall stress normalization of EF, have all been proposed as possible indices of a deterioration in intrinsic LV function.9,12,20,22,24,25 However, although studies of these indices have been able to identify patients who are already in the decompensated stage, none has been shown to determine when the transition stage begins. Indeed, as discussed later, the outcome of patients with MR depends largely on the severity of valve leakage, and in current practice, criteria for optimal timing of intervention rely mainly on quantitative measurements of the severity of mitral valve leakage rather than indices of LV function, size, or wall stress. The goal of optimal timing is to intervene before the decompensated stage of irreversible LV dysfunction occurs. The natural history of severe MR in the modern era is now well documented,2,14,18,26,27 on the basis of studies of patients followed up with flail posterior leaflet (a surrogate for severe MR) ( Figure 20-1). In an initial study by Ling et al, 14 of patients who were followed up for more than 10 years, mortality rate was higher (6.3% yearly) than the expected survival rate (see Figure ON20-1 on website). Twenty percent of patients receiving medical management died; 69% of the deaths were from cardiac causes. High morbidity was also noted, with 10-year incidences of atrial fibrillation of 30% and of heart failure 63%. Once heart failure developed, the prognosis was worse, with a 5-year survival of less than 20%. At 10 years, 90% of patients with a flail posterior leaflet had either died or undergone surgical repair because of the development of symptoms. 14 These high event rates were confirmed in a multicenter study, linearized event rates/year for those receiving nonsurgical management being 5.4% for atrial fibrillation, 8.0% for heart failure, and 2.6% for death 27 ( Figure 20-2). Sudden death is a frequent catastrophic event, responsible for approximately one fourth of deaths in patients receiving medical treatment. 28 FIGURE 20-1 Incidence of atrial fibrillation (AF), heart failure (HF), mitral valve surgery, and surgery or death. FIGURE 20-2 Long-term outcomes for patients with mitral regurgitation due to a flail mitral valve receiving medical treatment in a multicenter study. The natural history of predominantly asymptomatic patients with moderately severe MR and normal LV function has been controversial. Rosen et al 15 in 1994 reported a benign prognosis, with no deaths and no progression to subnormal LV function, after 5 years of follow-up. However, in this report, there was a 10% average annual risk for development of symptoms leading to surgery. In addition, the patients in this study most likely had less severe MR than those in other studies, given the smaller LV size and lack of quantitative measurements. 5 In a subset of patients from a multicenter study who were completely asymptomatic with normal LV function, the 5-year combined incidence of atrial fibrillation, heart failure, or cardiovascular death was 42% ± 8%. 27 FIGURE ON20-1 Observed and expected long-term survival with medical treatment in 229 patients with mitral regurgitation due to a flail mitral valve leaflet. The outcome of patients with severe MR is highly dependent on initial symptoms and LV function. In the study reported by Ling et al, 14 patients with New York Heart Association (NYHA) functional class III or IV symptoms who did not undergo an operation had considerable mortality (34% yearly) ( Figure 20-3). Even those patients with NYHA functional class I or II symptoms had a mortality of 4.1% per year. Those patients with an EF of less than 60% also had a substantial mortality in comparison with those whose EF was 60% or greater. Ten-year survival was 61% in patients with an EF greater than 60%, compared with 40% for patients with an EF less than 60% ( Figure 20-4). 14 FIGURE 20-3 Overall long-term survival with medical treatment in patients with flail mitral valve leaflet. FIGURE 20-4 Long-term survival with medical treatment in 229 patients with flail mitral valve leaflet. More data on the natural history of asymptomatic patients with MR has been accumulated on the basis of the ability not only to measure LV function but also to quantify the degree of MR. 29 After stratification by quantitative Doppler echocardiography, 456 patients with asymptomatic primary MR were prospectively followed. Five years after the diagnosis, 22% of patients had died (14% from cardiac causes) and one third of patients suffered a cardiac event, defined as death from cardiac cause, heart failure, or new atrial fibrillation. Independent determinants of survival were age, presence of diabetes, but also the regurgitant orifice area (ROA), which provides a quantitative measure of severity of MR. Those patients with an ROA of at least 40 mm2 had a 5-year survival rate lower than expected on the basis of U.S. census data (58% versus 78%). In comparison with patients with an ROA of less than 20 mm2, those with an ROA of at least 40 mm2 had a higher risk of death from any cause, of death from cardiac causes, and of cardiac deaths ( Figures 20-5 and 20-6). This finding has been confirmed in a study of 286 patients with asymptomatic severe MR who were monitored medically. The ROA as well as the baseline grade of pulmonary hypertension were independent predictors of heart failure or need for surgery. 30 FIGURE 20-5 Kaplan-Meier estimates of the mean (± SE) rates of cardiac events among patients with asymptomatic mitral regurgitation receiving medical management. FIGURE 20-6 Kaplan-Meier estimates of the mean (± SE) rates of death from cardiac causes among patients with asymptomatic mitral regurgitation receiving medical management. Overall, the presence of severe MR portends a poor prognosis, even in the asymptomatic patient with preserved EF. This insight into the natural history of patients with MR has important implications regarding timing of operation. Data show very clearly that patients with a regurgitant volume of at least 60 mL/beat or an ROA of at least 40 mm2 have a poor outcome with medical management alone. In addition, close follow-up of patients with intermediate grades of MR (ROA 20 to 39 mm2) is essential. Although these patients with less severe MR have low risk of death and cardiac events during the first 12 to 18 months after diagnosis, the rates of death and other complications increase substantially thereafter. 29 LA enlargement is the end result of the pathophysiologic response to MR. LA enlargement strongly predicts survival and other cardiac events (heart failure, atrial fibrillation) in patients with MR managed medically ( Figure 20-7; see also Figure ON20-2). Compared with patients with LA volume less than 40 mL/m2, those with LA volume greater than 60 mL/m2 have increased mortality and rate of cardiac events31,32 Among patients with marked LA dilation, mortality and cardiac event rates are lower in those treated surgically compared to those maintained on medical management ( Figure 20-8; see also Figure ON20-3). FIGURE 20-7 Cardiac events after diagnosis of severe mitral regurgitation. FIGURE 20-8 Cardiac events after diagnosis of mitral regurgitation in patients with markedly enlarged left atrium. There has been interest in the use of measurements of natriuretic peptides for predicting outcome in patients with MR.33–35 Brain natriuretic peptide (BNP) activation in MR increases with the severity of MR 35. BNP Levels of brain natriuretic peptide are independently predictive of heart failure and mortality in patients with MR33–35 ( Figure 20-9; see also Figures ON20-4 and ON20-5). FIGURE 20-9 Survival free of heart failure or left ventricular systolic dysfunction (LVDSD) according to initial brain natriuretic peptide (BNP) levels. Determination of optimal timing of valve operation requires knowledge of the risks and benefits of the operation itself. There have been significant changes in the surgical treatment of MR, with substantial effect on the operative mortality and long-term outcome ( Figure 20-10). In North America, the most common cause of MR is primary degenerative valve disease, and the most common pathophysiologic mechanism is leaflet prolapse. More than 95% of patients with leaflet prolapse can undergo surgery with low operative risk and high feasibility of repair (see Figure ON20-6), with a durability that approaches that of prosthetic replacement. In our clinic, operative risk for valve repair in patients 75 years or younger is less than 1%. Linearized risk of reoperation after repair of posterior leaflet prolapse is approximately 0.5% per year, and rates of reintervention after repair of anterior or bileaflet prolapse are similarly low (1.6% and 0.9% per year, respectively). Indeed, the durability of mitral repair for all subsets of patients with leaflet prolapse in the current era (0.74% per year overall) is similar to that following mitral valve replacement. 36 FIGURE 20-10 Trends in operative mortality for surgery for mitral regurgitation (MR) throughout four time periods (1980-1983, 1984-1987, 1988-1991, and 1992-1995). FIGURE ON20-2 Mortality associated with left atrial (LA) enlargement, stratified by regurgitant (REG) volume. (From Le Tourneau T, Messika-Zeitoun D, Russo A, et al. Impact of left atrial volume on clinical outcome in organic mitral regurgitation. J Am Coll Cardiol 2010;56:570–8.) FIGURE ON20-3 Mortality after diagnosis of mitral regurgitation in patients with markedly enlarged left atrium who underwent medical treatment and surgical management. (From Le Tourneau T, Messika-Zeitoun D, Russo A, et al. Impact of left atrial volume on clinical outcome in organic mitral regurgitation. J Am Coll Cardio. 2010;56:570–8.) FIGURE ON20-4 Percent of patients reaching combined end point (symptoms of heart failure, left ventricular systolic dysfunction or death [LVDSD]). FIGURE ON20-5 Receiver-operator curve (ROC) analysis showing incremental value of BNP levels of 105 pg/mL or greater when added to echocardiographic variables for the prediction of heart failure, left ventricular systolic dysfunction, or death. Mitral valve repair is preferred over prosthetic replacement because of low operative mortality and elimination of device-related complications such as ventricular rupture, thrombus formation, or mechanical malfunction.5,18 With valve repair, the chordal apparatus is preserved, and studies in patients undergoing valve replacement show that the preservation of mitral valve attachments preserves LV geometry and systolic function. 37 Also, valve repair has a much lower rate of late complications than prosthetic replacement. The survival advantage of repair over replacement extends to patients who undergo reoperation for late failure of initial repair. 36 There have also been improvements in outcome for patients who cannot undergo mitral valve repair but require mitral valve replacement. Studies have shown that preservation of the chordal apparatus at the time of valve insertion results in a smaller postoperative chamber size, prevents the postoperative increase in systolic stress, and maintains normal ejection performance.38–41 Thus, the preservation of the chordal apparatus has a lower risk of LV dysfunction following mitral valve operation than the resection of supporting mitral valve structures.38–41 The factors that have been shown to influence early mortality following mitral valve operation are the patient’s age and NYHA functional class. 42 Operative mortality continues to improve each decade and is related to surgical expertise.5,6,27 FIGURE ON20-6 Trends in feasibility of mitral valve repair. The major cause of death after surgical correction of MR is continued heart failure.2,11,19,42–44 The important clinical predictors of late mortality and heart failure following operation are older age, elevated serum creatinine, elevated systolic blood pressure, presence of coronary artery disease, and advanced functional class42,43 ( Figure 20-11). Echocardiographic parameters that predict late mortality after operation are EF and end-systolic dimension.5,16 FIGURE 20-11 Overall postoperative survival following operation for severe mitral regurgitation. As would be expected, postoperative LV dysfunction, as assessed by EF, remains a major predictor of poor outcome.2,11,19,42–44 A decreased EF postoperatively is highly associated with future mortality and the onset of heart failure. Thus, it is essential to attempt to determine factors associated with postoperative LV dysfunction. A multitude of studies have attempted to predict residual postoperative LV systolic dysfunction.9,12,20,22,24,25 The ejection phase indices of LV function (EF and fractional shortening) were not thought to be of benefit in evaluating intrinsic contractility of the left ventricle or patient outcome because of the changes in load on the ventricle from the severe MR (see Figure ON20-7). Thus, other parameters had been identified, such as preload-corrected EF, end-systolic volume index normalized to wall stress, and diastolic volume mass normalization of LV elastance. Despite the elegant pathophysiologic theoretical models underlying these parameters, these studies showed only that all these parameters demonstrated when it was “too late” for operation (see Figure ON20-8).9,12,20,22,24,25 The “cutoff” values from each study predicted when patients had a high risk of severe heart failure or death following operation but did not predict the optimal timing of operation. It must be noted that these prior studies might not be applicable to surgical outcomes today, because they included small number of patients, mixed valve disease, conservative selection bias, as well as the use of valve replacement with or without chordal sparing.9,12,20,22,24,25 Later studies have looked at the determinants of residual postoperative LV dysfunction in the era of mitral valve repair.2,3,18,42–46 Overall, EF drops by approximately 10% in patients with degenerative MR, on average from 58% to 50%.42,43 Several theories have been put forward to explain this observation, including acute increase in LV afterload and myocardial injury during operation as a result of global ischemia and reperfusion. An echocardiographic and hemodynamic study of LV function immediately after mitral valve repair demonstrated that indexes of global systolic function decreased significantly from preoperative values (P <0.001), primarily because of an increase in LV end-systolic size.47,48 At the same time, hemodynamic parameters, including cardiac output and forward stroke volume, were maintained after surgery, suggesting preservation of cardiac pump function. Indeed, control patients in the investigation, who were undergoing coronary artery bypass grafting and had cardioplegic arrest for intervals similar to or longer than those in patients undergoing MV repair, exhibited no change in postoperative LV systolic function and hemodynamic parameters except for increased heart rate. The best explanation for these data is that immediately after correction of MR, the LV undergoes volumetric adjustments to ensure constant forward stroke volume at the expense of decreased EF. With time, there is reverse remodeling with decrease in LV end-diastolic dimension and appropriate increase in EF to maintain stroke volume. An important issue for clinicians and their patients is the extent to which LV function and reverse remodeling occurs late after correction of MR. In a retrospective study from our clinic, Enriquez-Sarano et al 43 reported that in 217 patients with organic mitral valve disease, average EF 1 year after correction of MR was 52%, compared with 62% preoperatively (P < 0.001), and this decline was due to decreased LV end-diastolic dimension and minimal change in LV end-systolic dimension. Suri et al 48 extended these studies and reported that after an early decrease, the EF in patients undergoing mitral valve repair or replacement improved steadily throughout the follow-up period, which extended to 10 years. Predictors of recovery of EF included larger preoperative EF, smaller LV chamber size, mitral valve repair rather than replacement, and surgery during the 1990s versus operation in an earlier era. Taken together, these findings further support the advantage of early repair of severe MR, before there is an important drop in EF. Indeed, in this study the most important thresholds predicting recovery of normal LV EF were preoperative EF 65% or larger and LV systolic dimension less than 36 mm. Despite the limitations of the EF, this measurement has emerged as the best predictor for determining postoperative LV systolic dysfunction as well as the onset of heart failure and/or mortality ( Figure 20-12).2,3,18,42–46 Patients with a preoperative EF of less than 60% have a higher incidence of postoperative LV dysfunction as well as an increased incidence of poor outcome.2,42,43 Even those with EF between 50% and 60% had a poorer outcome than patients with EF greater than 60%. FIGURE 20-12 Late survival of patients undergoing operation for severe mitral regurgitation.
Mitral Regurgitation
Timing of Surgery
Recent Advances
Pathophysiology
Acute Volume Overload Stage
Chronic Compensated Stage
Decompensated Stage with Irreversible Left Ventricular Dysfunction
Transition Stage (From Compensated to Decompensated Stage)
Natural History
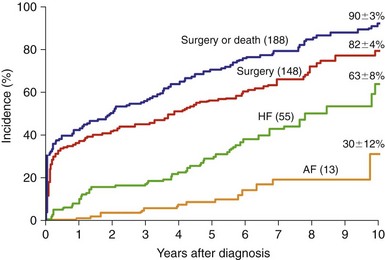
In 229 patients with isolated mitral regurgitation due to flail mitral valve leaflet between 1980 and 1989, there was a high event rate at 10-year follow-up. (From Ling LH, Enriquez-Sarano M, Seward JB, et al. Clinical outcome of mitral regurgitation due to flail leaflet. N Engl J Med 1996;335:1417–23.)
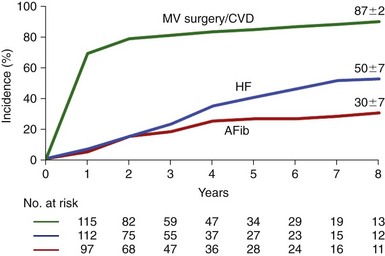
Note the high 8-year event rate, similar to the outcome seen in Figure 20-1. AFib, Atrial fibrillation; CVD, cardiovascular death; HF, heart failure; MV, mitral valve. (From Grigioni F, Tribouilloy C, Avierinos JF, et al. Outcomes in mitral regurgitation due to flail leaflets a multicenter European study. JACC Cardiovasc Imaging 2008:1:133–41.)
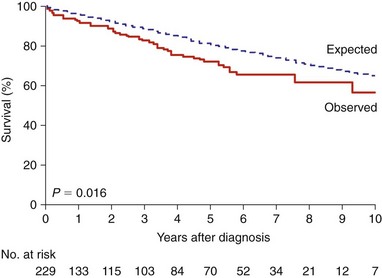
Survival in the patients with a flail mitral valve was lower than expected. (From Ling LH, Enriquez-Sarano M, Seward JB, et al. Clinical outcome of mitral regurgitation due to flail leaflet. N Engl J Med 1996;335:1417–23.)
Predictors of Outcome
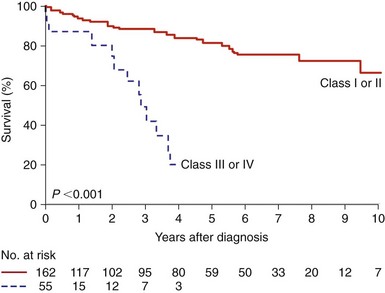
Patients are subdivided according to New York Heart Association functional class. (From Ling LH, Enriquez-Sarano M, Seward JB,et al. Clinical outcome of mitral regurgitation due to flail leaflet. N Engl J Med 1996;335:1417–23.)
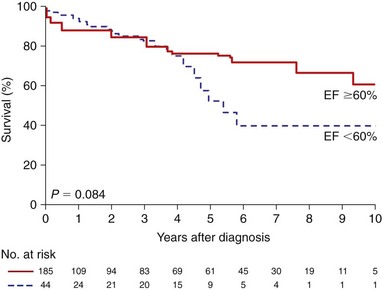
Patients are subdivided according to ejection fraction (EF) value. (From Ling LH, Enriquez-Sarano M, Seward JB, et al. Clinical outcome of mitral regurgitation due to flail leaflet. N Engl J Med 1996;335:1417–23.)
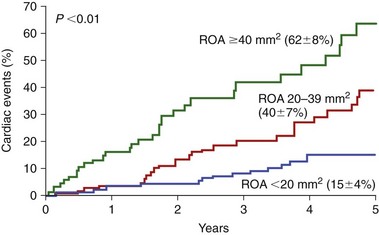
Patients are subdivided according to the regurgitant orifice area (ROA). Cardiac events were defined as death from cardiac causes, heart failure, or new atrial fibrillation. Values in parentheses are survival rates at 5 years. (From Enriquez-Sarano M, Avierinos J-F, Messika-Zeitoun D, et al. Quantitative determinants of the outcome of asymptomatic mitral regurgitation. N Engl J Med 2005;352:875–83.)
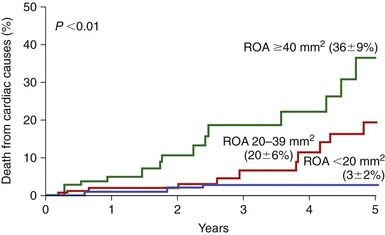
Patients are subdivided according to the regurgitant orifice area (ROA). Values in parentheses are survival rates at 5 years. (From Enriquez-Sarano M, Avierinos J-F, Messika-Zeitoun D, et al. Quantitative determinants of the outcome of asymptomatic mitral regurgitation. N Engl J Med 2005;352:875–83.)
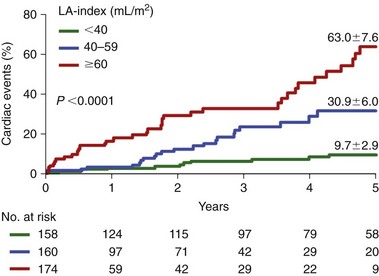
Patients are subdivided according to left atrial (LA) volume. (From Le Tourneau T, Messika-Zeitoun D, Russo A, et al. Impact of left atrial volume on clinical outcome in organic mitral regurgitation. J Am Coll Cardiol 2010;56:570–8.)
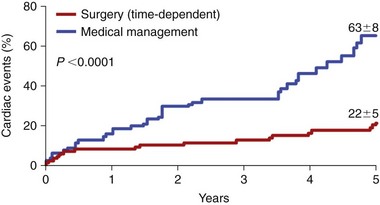
Patients receiving medical management are compared to those treated surgically. (From Le Tourneau T, Messika-Zeitoun D, Russo A, et al. Impact of left atrial volume on clinical outcome in organic mitral regurgitation. J Am Coll Cardiol 2010;56:570–8.)
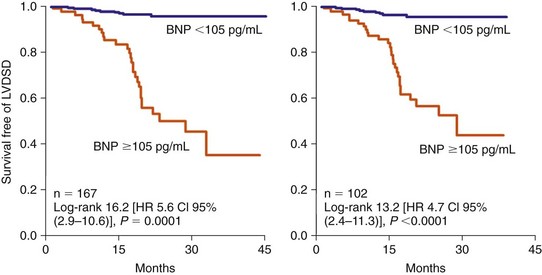
Left, derivation set of patients; Right, validation set of patients. CI, confidence interval; HR, hazard ratio. (From Pizarro R, Bazzino OO, Oberti PF, et al. Prospective validation of the prognostic usefulness of brain natriuretic peptide in asymptomatic patients with chronic severe mitral regurgitation. J Am Coll Cardiol 2009;54:1099–106.)
Advances in Surgical Intervention
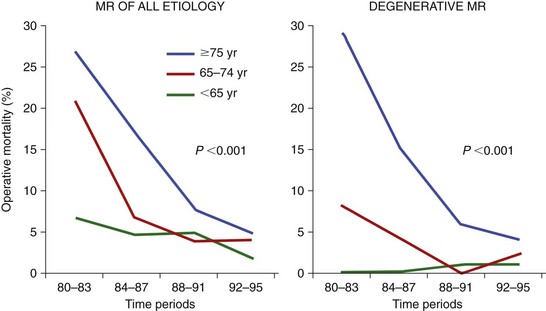
The operative mortality is shown for patients in three age ranges. Left, Trends in operative mortality for all causes of MR. Right, Trends in operative mortality for primary degenerative MR. The probability (P) values apply to the time trends for all patients irrespective of age. (From Detaint D, Sundt TM, Nkomo VT, et al. Surgical correction of mitral regurgitation in the elderly: outcomes and recent improvements. Circulation 2006;114:265–72.)
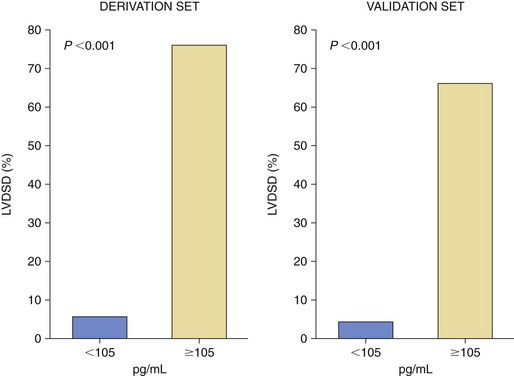
Patients are subdivided according to brain natriuretic peptide (BNP) values (in pg/mL). (From Pizarro R, Bazzino OO, Oberti PF, et al. Prospective validation of the prognostic usefulness of brain natriuretic peptide in asymptomatic patients with chronic severe mitral regurgitation. J Am Coll Cardiol 2009;54:1099–106.)
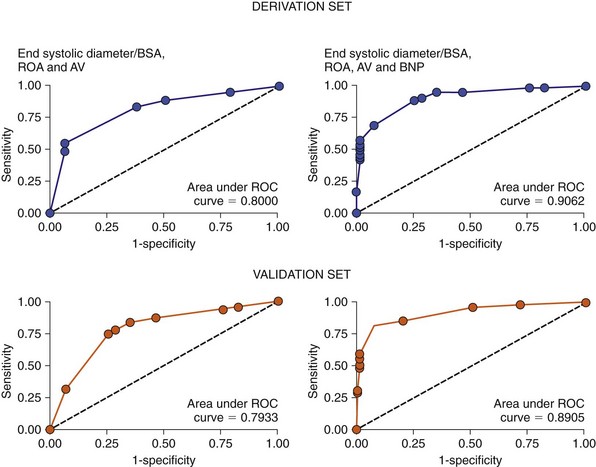
AV, atrial volume; BNP, brain natriuretic peptide; BSA, body surface area; ROA, regurgitant orifice area. (From Pizarro R, Bazzino OO, Oberti PF, et al. Prospective validation of the prognostic usefulness of brain natriuretic peptide in asymptomatic patients with chronic severe mitral regurgitation. J Am Coll Cardiol 2009:5;4:1099–106.)
Predictors of Surgical Outcome
Early Mortality
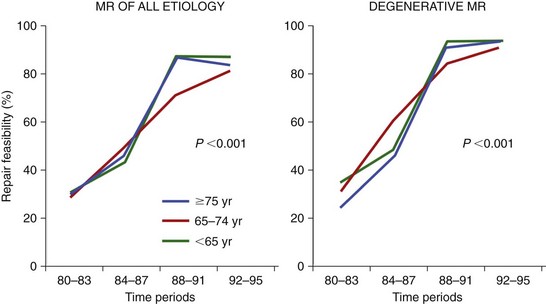
Trends in feasibility of mitral valve repair throughout four periods (1980-1983, 1984-1987, 1988-1991, 1992-1195) for patients in three age ranges. Left, Trends in valve repair for all causes of mitral regurgitation (MR). Right, Trends in valve repair for degenerative MR. The probability value applies to the time trends for patients in all age groups. (From Detaint D, Sundt TM, Nkomo VT, et al. Surgical correction of mitral regurgitation in the elderly: outcomes and recent improvements. Circulation 2006;114:265–72.)
Late Outcome
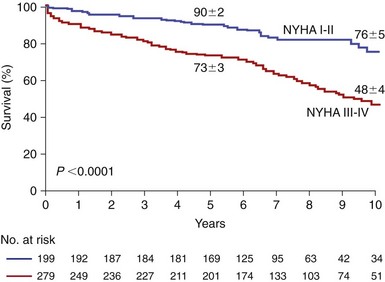
Patients in New York Heart Association (NYHA) functional classes I and II are compared to patients in NYHA functional class III and IV. (From Tribouilloy CM, Enriquez-Sarano M, Schaff HV, et al. Impact of preoperative symptoms on survival after surgical correction of organic mitral regurgitation: rationale for optimizing surgical indications. Circulation 1999;99:400–5.)
Prediction of Postoperative Left Ventricular Dysfunction
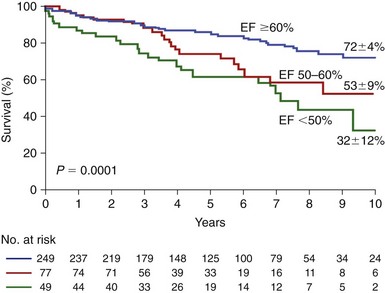
Patients are subdivided according to the preoperative echocardiographic ejection fraction (EF) value. Numbers of patients at risk for each EF and time interval are shown indicated under the graph. (From Enriquez-Sarano M, Tajik AJ, Schaff HV, et al. Echocardiographic prediction of survival after surgical correction of organic mitral regurgitation. Circulation 1994;90:830–7.)![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Mitral Regurgitation: Timing of Surgery
Only gold members can continue reading. Log In or Register to continue