The midterm clinical and functional benefits of percutaneous coronary intervention in patients aged ≥90 years have not been clearly defined. From January 2005 to June 2009, 173 patients aged ≥90 years underwent diagnostic cardiac catheterization, of whom 90 underwent percutaneous coronary intervention. There were 45 men (50%) and 45 women (50%), with a mean age of 92 years (range 90 to 101). Of these, 24 patients (27%) presented with ST-segment elevation myocardial infarction, 31 (34%) with non–ST-segment elevation myocardial infarction, 28 (31%) with unstable angina pectoris, and 2 (2%) with stable angina pectoris; 5 patients (6%) were studied for preoperative risk assessment. A total of 127 lesions were successfully treated using 102 drug-eluting stents and 37 bare-metal stents, with a mean of 1.5 stents per patient. Postprocedural complications included renal insufficiency in 5 patients (5.6%), heart failure in 6 patients (6.7%), and cardiogenic shock in 2 patients (2.2%). Seventy-seven patients (85.6%) experienced no postprocedural complications. In-hospital mortality was 7.8%, and actuarial survival was 61.5 ± 5.2% at 24 months and 31.6 ± 6.1% at 48 months. The SF-36 Health Survey was administered at follow-up, and results demonstrated a quality of life similar to that of the general population corrected for age and gender. In conclusion, this study demonstrates that percutaneous coronary intervention in nonagenarians can be accomplished with low mortality and morbidity and excellent midterm results. Moreover, functional improvement in nonagenarians supports enhanced quality of life comparable to that of the general population.
We reviewed the impact of percutaneous coronary intervention (PCI) in a cohort of nonagenarians and determined the influence of this therapeutic strategy on patients’ health-related quality of life.
Methods
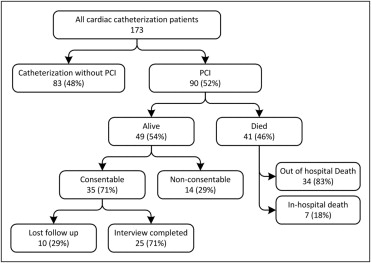
After receiving institutional review board approval, we performed a retrospective analysis of outcomes and complications using a database with >200 data points, including all patients aged ≥90 years who underwent cardiac catheterization and/or PCI at JFK Medical Center from January 1, 2005, to June 30, 2009. A search of the Social Security Death Index was conducted to discern patients’ current status (alive vs deceased). All surviving patients who were deemed capable of giving appropriate responses when contacted by telephone were qualified for the SF-36 Health Survey to assess quality of life ( Figure 1 ). English-speaking patients, those not in hospice care, and those with life expectancies ≥6 months were included in the study. After obtaining informed consent, these patients were questioned using an institutional review board–approved standard SF-36 survey, and responses were computed to determine their quality of life. The SF-36 measures 8 health domains and provides psychometrically based physical and mental component summary scores.
Results
A total of 173 patients aged ≥90 years underwent diagnostic cardiac catheterization, including 88 men and 85 women. Their age ranged from 90 to 101 years, with a mean age of 92 years. There were 32 patients (18.5%) with ST-segment elevation myocardial infarction, 50 (28.9%) with non–ST-segment elevation myocardial infarction, 59 (34.1%) with unstable angina pectoris, 4 (2.3%) with stable angina pectoris, 5 (2.9%) with atypical chest pain, and 23 (13.3%) who had undergone catheterization without intervention for preoperative risk assessment. Patient histories, co-morbidities, and presenting syndromes are listed in Tables 1 and 2 .
| Condition | Number (%) |
|---|---|
| History of hypertension | 148 (86%) |
| History of dyslipidemia | 89 (51%) |
| Smoker | 60 (35%) |
| Previous myocardial infarction (>7 days) | 59 (34%) |
| Current heart failure | 46 (27%) |
| Creatinine >1.4 mg/dl | 45 (26%) |
| Previous PCI | 42 (24%) |
| Cerebrovascular disease | 29 (17%) |
| History of heart failure | 27 (16%) |
| Diabetes mellitus | 25 (15%) |
| Peripheral artery disease | 25 (15%) |
| Previous coronary bypass | 22 (13%) |
| Chronic lung disease | 19 (11%) |
| Family history of coronary artery disease | 5 (3%) |
| Condition | Number (%) |
|---|---|
| ST-segment elevation myocardial infarction | 32 (19%) |
| Non–ST-segment elevation myocardial infarction | 50 (29%) |
| Unstable angina pectoris | 59 (34%) |
| Stable angina pectoris | 4 (2%) |
| Atypical chest pain | 5 (3%) |
| Asymptomatic (preoperative risk assessment) | 23 (13%) |
| Left ventricular ejection fraction (%) | 46 (15–75) |
Of the 173 patients, 83 underwent diagnostic catheterization alone, while 90 patients underwent PCI, with a total of 139 stents deployed ( Figure 1 ). There were 1.54 stents per patient, of which 102 were drug-eluting stents and 37 were bare-metal stents. There were 127 lesions attempted, and all but 3 were successfully dilated, the characteristics of which are listed in Table 3 . The total in-hospital mortality was 8.1% (13 of 173). The PCI group accounted for 7 of those 13 patients. A Kaplan-Meier survival curve of the PCI group ( Figure 2 ) demonstrates overall excellent survival. The incidence of various complications in the total cohort and the PCI group is listed in Table 4 .
| Variable | Value |
|---|---|
| Location of lesion | |
| Left main | 4 (3%) |
| Left anterior descending | 46 (36%) |
| Proximal | 27 |
| Mid | 16 |
| Distal | 3 |
| Right coronary artery | 45 (35%) |
| Proximal | 24 |
| Mid | 19 |
| Distal | 2 |
| Circumflex | 14 (11%) |
| Proximal | 7 |
| Mid | 5 |
| Distal | 2 |
| First diagonal | 6 (5%) |
| Obtuse marginal | 8 (6%) |
| First | 6 |
| Second | 1 |
| Third | 1 |
| Posterior descending | 2 (2%) |
| Ramus intermedius | 2 (2%) |
| Stent characteristics | |
| Total number of stents | 139 |
| Drug-eluting stents | 102 (73%) |
| Bare-metal stents | 37 (27%) |
| Total number of lesions | 127 |
| Lesions attempted | 127 |
| Lesions successfully dilated | 124 (98%) |
| Total length of lesions (mm) | 1,866 |
| Complication | All Patients (n = 173) | Patients Who Underwent PCI (n = 90) |
|---|---|---|
| Renal failure | 6 (4%) | 5 (6%) |
| Heart failure | 6 (4%) | 6 (7%) |
| Cardiogenic shock | 2 (1%) | 2 (2%) |
| Bleeding | 4 (2%) | 4 (4%) |
| Percutaneous entry site | 1 (1%) | 1 (1%) |
| Gastrointestinal | 1 (1%) | 1 (1%) |
| Genital/urinary | 1 (1%) | 1 (1%) |
| Other/unknown | 1 (1%) | 1 (1%) |
| Vascular complications | 4 (2%) | 3 (3%) |
| Dissection | 2 (1%) | 2 (2%) |
| Pseudoaneurysm | 2 (1%) | 1 (1%) |
| Stroke | 2 (1%) | 1 (1%) |
| Mortality | ||
| In-hospital | 13 (8.1%) | 7 (7.8%) |
| 0–30 days | 7 (4.0%) | 3 (3.3%) |
| 30 days to 6 months | 18 (10.4%) | 8 (8.8%) |
| 6 months to 1 year | 9 (5.2%) | 4 (4.4%) |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


