We read an article by Santarpino et al regarding clinical and cost data after transcatheter aortic valve implantation (TAVI) versus sutureless aortic valve replacement (AVR). The authors concluded that TAVI entailed higher follow-up mortality than sutureless AVR (overall survival rate 93% vs 99%; p = 0.025). Meanwhile, we have demonstrated in a recent meta-analysis of 7 observational comparative studies that sutureless (including rapid deployment) AVR is associated with a statistically significant reduction in early (inhospital or 30-day) all-cause mortality (2.5% vs 7.3%; odds ratio 0.33; 95% confidence interval [CI] 0.16 to 0.69; p = 0.003; risk difference −5.23%; 95% CI −8.12% to −2.33%; p = 0.0004) and postoperative paravalvular aortic regurgitation (PAR) compared with TAVI. To determine whether sutureless AVR reduces not merely early but also midterm mortality compared with TAVI, we here would like to perform a meta-analysis of comparative studies.
Databases including MEDLINE, EMBASE, and the Cochrane Central Register of Controlled Trials were searched through November 25, 2015, using Web-based search engines (PubMed and OVID). Search terms included “sutureless,” “rapid-deployment,” “Enable,” “Intuity,” “Perceval,” or “Trilogy”; “percutaneous,” “transcatheter,” “transluminal,” “transarterial,” “transapical,” “transaortic,” “transcarotid,” “transaxillary,” “transsubclavian,” or “transfemoral;” and “aortic valve.” Studies considered for inclusion met the following criteria: the design was a comparative study; the study population was patients with severe aortic valve stenosis, patients were assigned to TAVI versus sutureless AVR; and main outcomes included midterm (≥1 year) all-cause mortality (or overall survival). A hazard ratio (HR) with its 95% CI of midterm all-cause mortality for TAVI versus sutureless AVR was abstracted from each individual study. For studies that did not report an HR with corresponding variance, this was calculated from Kaplan-Meier curve or summary data using a HR calculation spreadsheet provided by Tierney et al based on statistical methods reported by Parmar et al and Williamson et al. Study-specific estimates were combined using inverse variance-weighted averages of logarithmic HRs in the random-effects model.
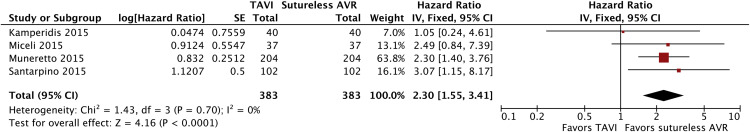
Of 97 potentially relevant articles screened initially, no randomized controlled trial and 4 eligible propensity score–matched studies were identified. These included median 1.5-year, median 13-month, mean 42.5-month, and mean 24.5-month all-cause mortality (or overall survival) by Kamperidis et al, Miceli et al, Muneretto et al, and Santarpino et al, respectively. Two of the 4 individual studies demonstrated a statistically significant benefit of sutureless AVR over TAVI for midterm all-cause mortality. A pooled analysis of the 4 studies (representative 766 patients) demonstrated a statistically significant increase in midterm all-cause mortality with TAVI relative to sutureless AVR (HR 2.30; 95% CI 1.55 to 3.41; p <0.0001; Figure 1 ).