Clinical outcomes for unprotected left main coronary artery (ULMCA) disease between coronary artery bypass grafting (CABG) and drug-eluting stents (DESs) remain controversial. We aimed to compare the safety and efficacy of percutaneous coronary intervention (PCI) using DESs with CABG in patients with ULMCA disease. Databases were searched for clinical studies that reported outcomes after PCI with DESs and CABG for treatment of ULMCA disease. End points of this meta-analysis were mortality; composite of death, myocardial infarction (MI), or stroke; and target vessel revascularization at 1-year follow-up. Pooled effects were calculated using fixed-effects model (Mantel–Haenszel method) or random-effects models (Dersimonian–Laird method). Twelve clinical studies (3 randomized trials and 9 observational studies) with 5,079 patients were involved in this study. At 1-year follow-up, there were trends toward lower risk of death (odds ratio [OR] 0.68, 95% confidence interval [CI] 0.45 to 1.02) and the composite end point of death, MI, or stroke (OR 0.70, 95% CI 0.49 to 1.00) in the DES group compared to the CABG group. However, target vessel revascularization was significantly higher in the DES group compared to the CABG group (OR 3.52, 95% CI 2.72 to 4.56). In conclusion, PCI with DESs is associated with favorable outcomes for mortality; composite end point of death, MI, or stroke; and a higher risk of target vessel revascularization compared to CABG in patients with ULMCA disease.
Coronary artery bypass grafting (CABG) is traditionally considered the standard revascularization strategy for patients with unprotected left main coronary artery (ULMCA) disease and current practice guidelines recommend CABG as the treatment of choice. Many recent studies have shown that patients receiving drug-eluting stents (DESs) have developed comparable mortality rates and major adverse cardiac and cerebrovascular events when compared to patients undergoing CABG despite a significantly higher rate of repeat revascularization in percutaneous coronary intervention (PCI) using DESs. However, these studies have been limited by their retrospective nature, small number of patients, and/or single-center design. Therefore, we performed an updated meta-analysis of randomized trials and observational studies to assess the safety of efficacy of PCI with DESs and CABG in patients with ULMCA disease.
Methods
We identified relevant studies through electronic searches of MEDLINE, EMBASE, and the Cochrane Central Register of Controlled Trials from 2001 through July 31, 2011. Medical subject headings and keyword searches included the terms “coronary artery bypass surgery,” “drug-eluting stent,” “sirolimus-eluting stent,” “paclitaxel-eluting stent,” paired with “left main coronary artery.”
Studies included in this meta-analysis were based on predetermined criteria: (1) studies comparing the efficacy and safety of DES to those of CABG in patients with ULMCA disease and (2) follow-up duration ≥12 months. Studies using only bare-metal stents or combination of bare-metal stents and DESs were excluded from analysis. We assessed the quality of the retrieved studies to ensure minimization of biases ( Table 1 ). Two independent reviewers (J.-S.J. and Y.-H.K.) extracted relevant information from the articles including data on authorship, study period, publication year, study design, study region, baseline characteristics of patients, sample size, clinical events, and duration of follow-up.
| Study | Prospective Design | Multicenter Enrollment | Selection Bias | Performance Bias | Attrition Bias | Detection Bias | Multivariate Adjustment for Potential Confounders |
|---|---|---|---|---|---|---|---|
| Lee et al | 0 | 0 | B | B | D | B | probably adequate |
| Chieffo et al | 0 | 0 | B | B | A | B | probably adequate |
| Sanmartín et al | 0 | 0 | A | B | A | B | probably adequate |
| MAIN-COMPARE | + | + | A | B | A | B | probably adequate |
| Mäkikallio et al | 0 | 0 | C | B | D | B | probably adequate |
| Cheng et al | 0 | 0 | C | B | D | B | probably adequate |
| SYNTAX left main coronary artery disease | + | + | A | B | A | B | probably adequate |
| Wu et al | 0 | 0 | B | B | D | B | probably adequate |
| Kang et al | 0 | + | B | B | A | B | probably adequate |
| PRECOMBAT | + | + | A | B | A | B | probably adequate |
| Boudriot et al | + | + | A | B | A | B | none reported |
| CUSTOMIZE | + | + | B | B | D | B | probably adequate |
Primary end points were mortality; composite of death, myocardial infarction (MI), or stroke; and target vessel revascularization at 1 year follow-up. Secondary end points were MI and stroke. Death was defined as death from any cause. Causes of noncardiac death included renal/hepatic failure, solid organ cancer, and pancreatitis. MI included Q-wave MI and non–Q-wave MI. Stroke was defined as a sudden neurologic deficit resulting from vascular lesions of the brain including hemorrhage, embolism, or thrombosis. Target vessel revascularization was defined as repeat PCI of the treated vessel including any segment of the left anterior descending and/or left circumflex coronary artery.
We used fixed-effects or random-effects models to produce across-study summary odds ratios (ORs) with 95% confidence intervals (CIs). Where no significant statistical heterogeneity was identified, the fixed-effects estimate was used preferentially as the summary measurement. All p values were 2-tailed, with statistical significance set at 0.05. For comparison of registry studies with matched pairs by propensity analysis, adjusted risk estimates were pooled after logarithmic transformation according to random-effects models with the generic inverse variance method. We assessed statistical heterogeneity between trials with I 2 statistic, which is derived from the Cochran Q and the degree of freedom (100 × [{Q – degree of freedom}/Q]). I 2 values <25%, >25%, 50%, and 75% were considered evidence of no, low, moderate, and severe statistical heterogeneity, respectively. For heterogeneity across studies, we performed sensitivity analyses, serially excluding studies to determine the source of heterogeneity. In addition, sensitivity analyses were conducted to examine heterogeneity by ethnicity among study populations, study design (randomized controlled trials vs observational cohort studies), and burden of coronary artery disease. Publication bias was examined by visual inspection of a constructed funnel plot for composite end point of death, MI, or stroke and mathematically by Egger test (p for significant symmetry <0.1). For specific evaluation of the presence and extent of publication bias, we used the trim-and-fill method according to Duval and Tweedie, which imputes missing studies in the funnel plot based on symmetry assumptions. All statistical analyses were performed using Review Manager 5.1 (Nordic Cochrane Center, Copenhagen, Denmark) and MIX 2.0 (BiostatXL, Sunnyvale, California).
Results
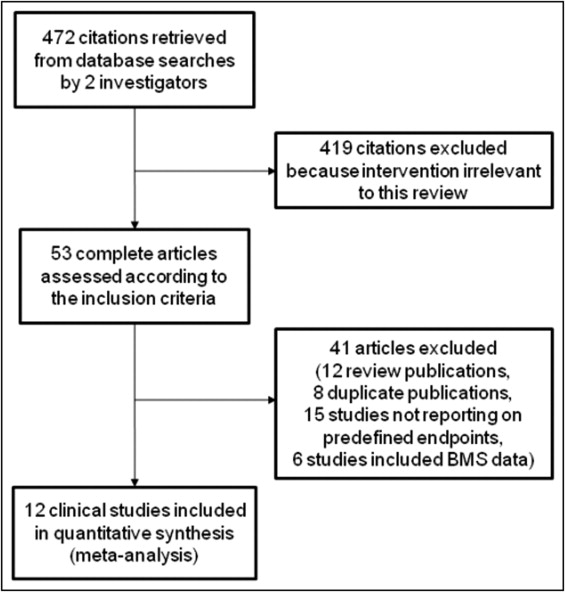
Figure 1 shows the process of inclusion and exclusion in the study. From 472 initial citations, we excluded 460 publications for various reasons. Therefore, 12 studies met our inclusion criteria. Characteristics of included studies are presented in Table 2 . Of 5,079 patients, 2,107 patients underwent PCI with DESs and 2,972 underwent CABG.
| Study | Year | Study Period | Design | Number (DES/CABG) | Stent Type | Study Region | Follow-Up (months) |
|---|---|---|---|---|---|---|---|
| Lee et al | 2006 | 2003∼2005 | observational cohort | 50/123 | SES/PES | USA | 12 |
| Chieffo et al | 2006 | 2002∼2004 | observational cohort | 107/142 | SES/PES | Europe (Italy) | 12, 60 |
| Sanmartín et al | 2007 | 2000∼2005 | observational cohort | 96/245 | SES/PES | Europe (Spain) | 12 |
| MAIN-COMPARE | 2008 | 2003∼2006 | observational cohort | 396/396 | SES/PES | Asia (Korea) | 36, 60 |
| Mäkikallio et al | 2008 | 2005∼2007 | observational cohort | 49/238 | SES/PES | Europe (Finland) | 12 |
| Cheng et al | 2009 | 2000∼2007 | observational cohort | 94/216 | SES/PES | Asia (Taiwan) | 36 |
| SYNTAX left main coronary artery disease | 2010 | 2005∼2007 | RCT | 357/348 | PES | USA/Europe | 12 |
| Wu et al | 2010 | 2003∼2006 | observational cohort | 131/245 | 126 SES/5 ZES | Asia (China) | 48 |
| Kang et al | 2010 | 2003∼2006 | observational cohort | 205/257 | SES/PES/ZES | Asia (Korea) | 36 |
| PRECOMBAT | 2011 | 2004∼2009 | RCT | 300/300 | SES | Asia (Korea) | 24 |
| Boudriot et al | 2011 | 2003∼2009 | RCT | 100/101 | SES | Europe (Germany) | 12 |
| CUSTOMIZE | 2011 | 2002∼2008 | observational cohort | 222/361 | various | Europe (Italy) | 12 |
A trial by Boudriot et al, the Premiere of Comparison of Bypass Surgery and Angioplasty Using Sirolimus-Eluting Stents in Patients with Unprotected Left Main Coronary Artery Disease (PRECOMBAT) trial, and the Synergy between Percutaneous Coronary Intervention with Taxus and Cardiac Surgery (SYNTAX) trial were multicenter randomized trials that compared the efficacy and safety of PCI with DESs to CABG for ULMCA disease. The other 9 studies were observational cohort studies with matched cohorts or consecutive patients. To identify possible differences between groups, preoperative prevalence of risk factors (diabetes, hypertension, hyperlipidemia, current smoking, previous MI or PCI, and history of stroke) and proportion of patients with acute coronary syndrome were extracted and compared ( Table 3 ). Probabilities of end points were estimated from Kaplan–Meier curves in 4 studies, where the actual rates of events were not reported.
| Study | Age | Male Gender (%) | Hypertension (%) | Diabetes (%) | Hyperlipidemia (%) | Current Smokers (%) | Renal Failure (%) | ACS (%) | Previous MI (%) | Previous PCI (%) | Previous CVA (%) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Lee et al | 72/70 | 50/76 ⁎ | 88/81 | 36/31 | 74/72 | 12/19 | 16/5 ⁎ | 66/45 ⁎ | NA/NA | NA/NA | 16/8 |
| Chieffo et al | 64/68 ⁎ | NA/NA | 59/76 ⁎ | 23/19 | 69/70 | 50/59 | 2/8 ⁎ | 32/22 | NA/NA | NA/NA | NA/NA |
| Sanmartín et al | 66/66 | 81/87 | 44/60 ⁎ | 19/32 ⁎ | 42/46 | 39/46 | 2/3 | 51/62 | NA/NA | 15/9 | NA/NA |
| MAIN-COMPARE | 62/64 ⁎ | 71/73 | 50/49 | 30/35 | 29/33 ⁎ | 26/30 ⁎ | 3/3 | 65/79 ⁎ | 8/12 ⁎ | 19/11 ⁎ | 7/7 |
| Mäkikallio et al | 72/70 ⁎ | 59/80 ⁎ | 46/46 | 20/17 | NA/NA | 20/18 | NA/NA | NA/NA | NA/NA | 6/3 | NA/NA |
| Cheng et al | 68/67 | 75/76 | 73/73 | 35/51 ⁎ | 72/46 ⁎ | 20/31 | 19/26 | 76/90 ⁎ | 19/29 | 39/23 ⁎ | 12/15 |
| SYNTAX left main coronary artery disease | 65/66 | 72/76 | 67/62 | 24/26 | 81/75 ⁎ | 18/24 ⁎ | 1/1 | 31/29 | 29/25 | NA/NA | 5/4 (TIA) |
| Wu et al | 62/64 | 76/83 | 65/62 | 27/29 | 32/31 | 39/39 | 2/7 | 28/69 | 12/15 | NA/NA | 8/11 |
| Kang et al | 64/66 | 70/74 | 63/67 | 38/44 | 55/60 | 43/49 | 10/11 | 45/65 ⁎ | 4/3 | 22/4 ⁎ | 15/11 |
| PRECOMBAT | 62/63 | 76/77 | 54/51 | 34/30 | 42/40 | 30/28 | 1/0 | 43/48 | 4/7 | 13/13 | NA/NA |
| Boudriot et al | 66/69 | 72/77 | 82/82 | 40/33 | 68/64 | 35/28 | NA/NA | NA/NA | 19/14 | NA/NA | NA/NA |
| CUSTOMIZE | 67/66 | 76/79 | 72/74 | 36/40 | 55/53 | 44/45 | 5/1 ⁎ | 100/100 | 36/37 | 27/14 ⁎ | NA/NA |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


