Clinical studies have indicated the existence of an “obesity paradox” in patients with chronic heart failure (HF), that is, reduced mortality in patients who have elevated body mass index (BMI) scores compared with normal-weight reference groups. The aim of this study was to investigate the relation of BMI with all-cause and cardiovascular (CV) mortality and hospitalization in patients with chronic HF though a systematic review and meta-analysis of published research. PubMed, the Cumulative Index to Nursing and Allied Health Literature, Cochrane Central, Scopus, web of science and Embase were searched for studies reporting rates of total mortality, cardiac mortality, and risk for hospitalization in patients with HF in various BMI categories (<20 kg/m 2 [low], 20 to 24.9 kg/m 2 [normal reference], 25 to 29.9 kg/m 2 [overweight], 30 to 34.9 [obese], and ≥35 kg/m 2 [severely obese]). Event rates were compared using a forest plot of relative risk (RR) using a random-effects model assuming interstudy heterogeneity. Two study investigators independently reviewed the 124 reports retrieved and identified 6 for final analyses (n = 22,807). After a mean follow-up period of 2.85 years, the risk for adverse events was highest in patients with low BMIs: total mortality RR 1.27 (95% confidence interval [CI] 1.17 to 1.37), CV mortality RR 1.20 (95% CI 1.01 to 1.43), and hospitalization RR 1.19 (95% CI 1.09 to 1.30). Risk for CV mortality and hospitalization was lowest in overweight patients (RR 0.79, 95% CI 0.70 to 0.90, and RR 0.92, 95% CI 0.86 to 0.97, respectively). Increasing degree of obesity failed to achieve a statistically significant effect on CV mortality (RR 0.82, 95% CI 0.64 to 1.05, and RR 0.71, 95% CI 0.50 to 1.01, for obese and severely obese, respectively) and on hospitalization (RR 0.99, 95% CI 0.92 to 1.07, and RR 1.28, 95% CI 0.88 to 1.87, for obese and severely obese, respectively). In conclusion, risk for total mortality and CV mortality and hospitalization was highest in patients with chronic HF who were underweight as defined by low BMI, whereas risk for CV mortality and hospitalization was lowest in overweight subjects.
The association between body mass index (BMI) and all-cause and cardiovascular (CV) mortality and hospitalizations in patients with heart failure (HF) is not fully understood. Because of contradictory results in various studies and the lack of definitive data on prognostic value of BMI and its purposeful alteration in HF, the American College of Cardiology Foundation and American Heart Association do not provide any firm recommendations for purposeful weight loss in HF. In the present study, were systematically reviewed the available evidence to examine the association between the most commonly used anthropometric measure of the degree of adiposity, BMI, and all-cause and CV mortality and hospitalizations in patients with chronic HF.
Methods
A meta-analysis was performed in accordance with the Meta-Analysis of Observational Studies in Epidemiology guidelines. A checklist of each of these criteria and how they were handled in our study is contained in Supplementary Table 1 .
We systematically searched PubMed, the Cumulative Index to Nursing and Allied Health Literature, Cochrane Central, Scopus, Embase and the Web of Science for all studies that reported total mortality, cardiac mortality, and rate of hospitalization on the basis of BMI. All relevant combinations of keywords related to body mass (e.g., “BMI,” “body weight,” “obesity,” “overweight,” “central obesity”), total mortality, CV events (e.g., “cardiac death,” “CV death,” “mortality”), hospitalization, readmission, and presence of HF (“systolic HF,” “diastolic HF,” “cardiomyopathy,” and “cardiac failure”) were included for database search. The search was conducted from the inception of these databases to May 31, 2014. No language or age restrictions were applied.
Clinical studies were included if the studies met the following criteria: (1) inclusion of patients with chronic HF and (2) reported measures of total mortality, CV mortality, and/or rate of hospitalization secondary to congestive HF exacerbation according to BMI.
We could not use the standard categorization of BMI groups because of inconsistency across studies. Thus, we arbitrarily assigned the low-BMI group when BMI was the lowest and <20 kg/m 2 , normal BMI if it was identical or close to 20 to 24.9 kg/m 2 , overweight if the BMI group was identical or close to 25 to 29.9 kg/m 2 , obesity if it was close or identical to 30 to 34.9 kg/m 2 , and severe obesity if BMI was ≥35 kg/m 2 .
Two independent reviewers (AS and AV) screened titles and abstracts for relevance. Discrepancies between reviewers were discussed until consensus was reached. The full text of selected titles or abstracts was reviewed for inclusion. Using the aforementioned selection criteria, the same 2 reviewers independently determined the reports to be included or excluded. Data from the relevant reports were extracted using predefined extraction forms. The same 2 independent reviewers performed the data extraction. Any disagreements in data extraction were discussed until consensus was reached. Events for studies that reported outcomes separately for patients with BMIs >35 kg/m 2 and >40 kg/m 2 were combined and reported as severely obese (>35 kg/m 2 ).
MIX 2.0 Pro (Biostat XL; http://www.biostatxl.com ) software was used to analyze the data. A random-effects model with inverse variance weighting was used to calculate pooled relative risks (RRs) (and 95% confidence intervals [CI]). We assessed 3 outcomes: total mortality, CV mortality, and rate of hospitalization. Heterogeneity among studies was assessed using Cochran’s Q test and the I 2 statistic, which denotes the percentage of total variation across studies that is a result of heterogeneity rather than chance. Heterogeneity was considered significant if the p value was <0.05. Publication bias was assessed using Begg’s test and Egger’s regression test. The influence of individual studies was examined by removing each study sequentially to assess the degree to which the meta-analysis estimate depends on a particular study (exclusion sensitivity analysis).
Results
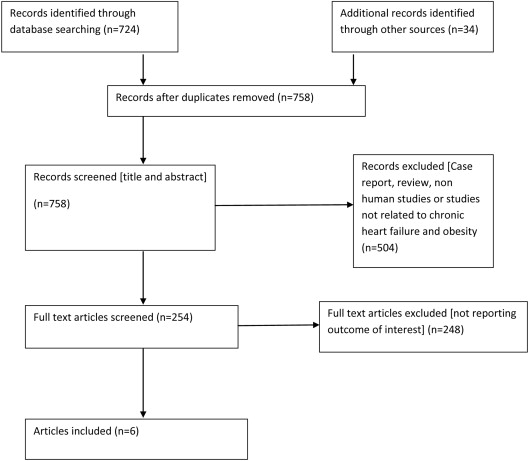
Six studies met the inclusion and exclusion criteria (n = 22,807) ( Figure 1 ). Follow-up duration ranged from 1.5 to 4.1 years. Details of the studies are listed in Table 1 . Obese patients were younger than normal- and low-BMI patients on average by 4 and 7 years, respectively ( Table 2 ).
| Author | Sample Size | Mean Age (years) | Male | Follow up (years) | NYHA Class | Study population | Post hoc analysis |
|---|---|---|---|---|---|---|---|
| Kenchaiah et al | 7599 | 66 | 68% | 3 | II-IV | CHARM † | + |
| Lavie et al | 206 | 54 | 81% | 1.5 | I-III | Single center study | ∗ |
| Curtis et al | 7767 | 64 | 75% | 3 | I-IV | DIG ‡ | + |
| Hamaguchi et al | 2488 | 70 | 60% | 2.1 | I-IV | JCARE-CARD § | + |
| Nochioka et al | 972 | 68 | 65% | 3.4 | I-IV | CHART ‖ | + |
| Haass et al | 4109 | 72 | n/a | 4.1 | II-IV | I-PRESERVE ¶ | + |
∗ single center study. + Yes (Post hoc analysis).
† Candesartan in Heart failure – Assessment of mortality and morbidity (CHARM).
‡ Digitalis Investigation Group (DIG) trial.
§ Japanese Cardiac Registry of Heart Failure in Cardiology (JCARE-CARD).
‖ Japanese HF patients in the Chronic Heart Failure Analysis and Registry in the Tohoku District (CHART) study.
¶ Irbesartan in HF and PRESERVed Ejection fraction (I-PRESERVE).
| BMI group | Mean age (in years) |
|---|---|
| <20 | 70.6 |
| 20–24·9 | 67.7 |
| 25-29.9 | 66.2 |
| 30-34.9 | 63.1 |
| ≥35 | 64.3 |
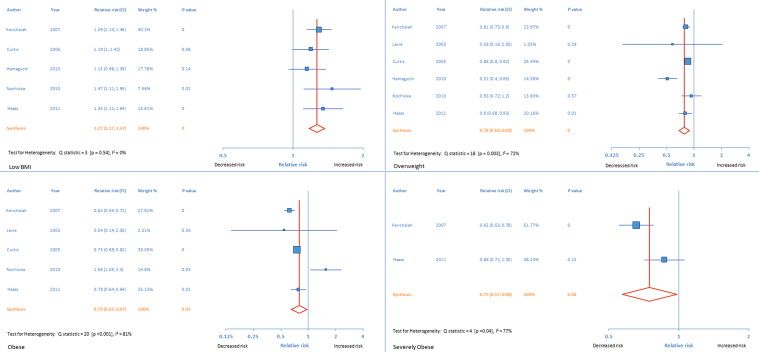
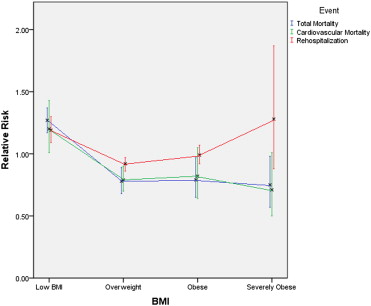
The low-BMI group had the greatest risk for total mortality, with an RR of 1.27 (95% CI 1.17 to 1.37), while the overweight, obese, and severely obese groups had lower RRs of 0.78 (95% CI 0.68 to 0.89), 0.79 (95% CI 0.65 to 0.97), and 0.75 (95% CI 0.57 to 0.98), respectively ( Figures 2 and 3 , Table 3 ). Heterogeneity analysis was significant across the overweight (p = 0.003, I 2 = 72%), obese (p <0.001, I 2 = 81%), and severely obese (p = 0.04, I 2 = 77%) groups. There was no heterogeneity across the low-BMI group (p = 0.54, I 2 = 0%).
| BMI | <20 | 20-24.9 | 25-29.9 | 30-34.9 | ≥35 |
|---|---|---|---|---|---|
| Total mortality | 1.27 [1.17 – 1.37] | 1 | 0.78 [0.68-0.89] | 0.79 [0.65-0.97] | 0.75 [0.57-0.98] |
| CV mortality | 1.20 [1.01 -1.43] | 1 | 0.79 [0.70-0.90] | 0.82 [0.64-1.05 | 0.71 [0.50-1.01] |
| Hospitalization | 1.19 [1.09 – 1.30] | 1 | 0.92 [0.86-0.97] | 0.99 [0.92-1.07] | 1.28 [0.88-1.87] |
The low-BMI group had the greatest risk for CV mortality (RR 1.20, 95% CI 1.01 to 1.43), while overweight patients had decreased risk compared with normal-weight patients (RR 0.79, 95% CI 0.70 to 0.90) and did not differ significantly from the obese and severely obese groups (RR 0.82, 95% CI 0.64 to 1.05, and RR 0.71, 95% CI 0.50 to 1.01, respectively) ( Figures 3 and 4 , and Table 3 ). Heterogeneity analysis was significant across the overweight (p = 0.03, I 2 = 60%), obese (p <0.001, I 2 = 82%), and severely obese (p = 0.04, I 2 = 77%) groups. There was no heterogeneity across the low-BMI group (p = 0.57, I 2 = 0%).
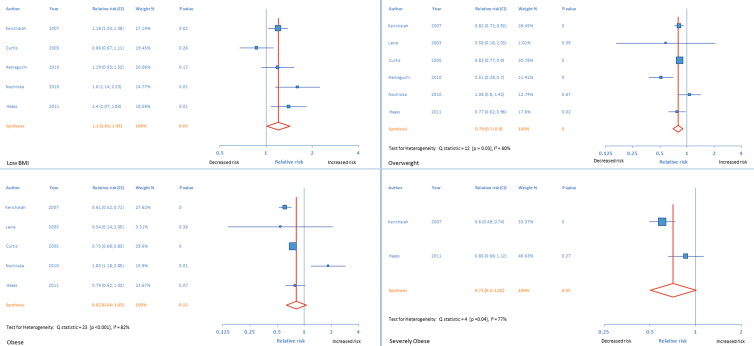
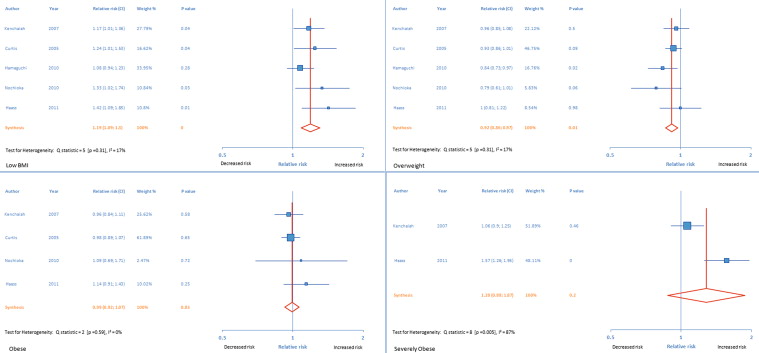
The risk for hospitalization secondary to HF exacerbation was highest in the low-BMI group (RR 1.19, 95% CI 1.09 to 1.30) and lowest in the overweight group (RR 0.92, 95% CI 0.86 to 0.97). The obese (RR 0.99, 95% CI 0.92 to 1.07) and severely obese (RR 1.28, 95% CI 0.88 to 1.87) groups did not have significantly different risk ( Figures 3 and 5 , Table 3 ). There was no significant heterogeneity among the low-BMI (p = 0.31, I 2 = 17%), overweight (p = 0.31, I 2 = 17%), and obese (p = 0.59, I 2 = 0%) groups, but significant heterogeneity was present across the studies in the severely obese group (p = 0.005, I 2 = 87%).