Epidemiologic studies evaluating the association of whole-grain intake with risk for coronary heart disease (CHD) have produced inconsistent results. The aim of this meta-analysis was to summarize the evidence from observed studies regarding the association between whole-grain intake and risk for CHD. Pertinent studies were identified by searching the Web of Knowledge and PubMed up to July 2014. A random-effects model was used to combine the results. Publication bias was estimated using Begg’s funnel plot and Egger’s regression asymmetry test. Ultimately, fourteen reports of 18 studies (15 cohort studies and 3 case-control studies) involving 14,427 patients with CHD and 400,492 participants were used in this meta-analysis. Pooled results suggested that highest whole-grain intake amount compared with the lowest amount was significantly associated with reduced risk for CHD (summary relative risk 0.787, 95% confidence interval 0.743 to 0.833), with no between-study heterogeneity observed (I 2 = 0%, p = 0.537). The association was significant in cohort studies but not in case-control studies. Inverse associations were also found in the United States and Europe. No publication bias was found. In conclusion, this meta-analysis indicates that higher whole-grain intake has a protective effect against CHD.
Coronary heart disease (CHD) is the leading cause of death in industrialized countries, accounting for up to 40% of all lethal events, and it is expected to be the leading cause of disease burden worldwide by 2020. Health behaviors, including nutrition, should be taken into account to reduce the risk for CHD, according to the American Heart Association. Whole grains include dark bread, whole-grain breakfast cereal, popcorn, cooked oatmeal, wheat germ, brown rice, bran, and other grains. Whole-grain foods contain fiber, vitamins, minerals, phenolic compounds, phytoestrogens, and other unmeasured constituents, which may have favorable effects on health by lowering serum lipids and blood pressure, improving glucose and insulin metabolism, improving endothelial function, and alleviating oxidative stress and inflammation. To date, a number of epidemiologic studies have been published that explored the relation between whole-grain intake and CHD. However, the results are not consistent. Therefore, we conducted a meta-analysis to (1) assess CHD risk for the highest versus lowest amount of whole-grain intake and (2) assess heterogeneity among studies and publication bias.
Methods
We performed a search of published research up to July 2014 using the databases of PubMed and the Web of Knowledge. The following search string was used: “[cardiovascular disease (CVD) OR myocardial infarction (MI) OR coronary heart disease (CHD) OR ischemic heart disease (IHD)] AND (whole grain OR diet OR lifestyle).” Results were restricted to studies conducted in humans. Moreover, we reviewed the reference lists from retrieved reports to search for further relevant studies.
Two investigators independently reviewed all identified studies, and studies were included if they met the following criteria: (1) a case-control or prospective design was used; (2) the exposure of interest was whole grains; (3) the outcome of interest was CHD, myocardial infarction, CVD, or ischemic heart disease; and (4) relative risk (RR) with 95% confidence intervals (CIs) was provided. If data were duplicated in >1 study, we included the study with the largest number of cases.
The following data were extracted from each study by 2 investigators: first author’s last name, year of publication, study design, geographic locations, sample source, the age range of study participants, the duration of follow-up, and the numbers of cases and participants. From each study, we extracted the RR that reflected the greatest degree of control for potential confounders. If there was disagreement between the 2 investigators about the eligibility of data, it was resolved by consensus with a third reviewer.
The pooled measure was calculated as the inverse variance–weighted mean of the logarithm of the RR with its 95% CI to assess the strength of association between whole-grain intake and the risk for CHD. A random-effects model was used to combine study-specific RRs (95% CIs), which considers within- and between-study variation. The I 2 statistic was used to assess heterogeneity, and I 2 values of 0%, 25%, 50%, and 75% represent no, low, moderate, and high heterogeneity, respectively. Publication bias was evaluated using Begg’s funnel plot and Egger’s regression asymmetry test. A study of influence analysis was conducted to describe how robust the pooled estimator was to the removal of individual studies. All statistical analyses were conducted with Stata version 11.0 (StataCorp LP, College Station, Texas). Two-tailed p values ≤0.05 were accepted as statistically significant.
Results
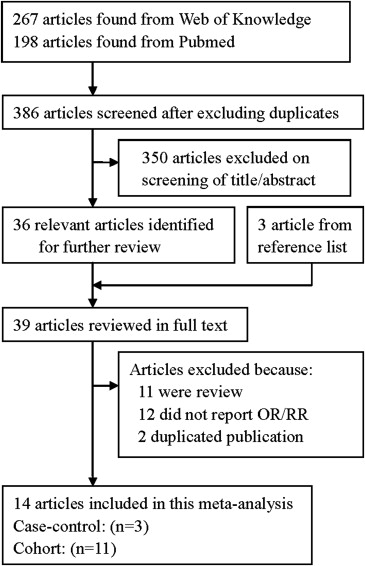
The detailed steps of our search are shown in Figure 1 . Fourteen reports of 18 studies (15 cohort studies and 3 case-control studies) involving 14,427 patients with CHD and 400,492 participants were used in this meta-analysis. Thirteen studies assessed whole-grain intake with a food-frequency questionnaire, and 5 studies assessed whole-grain intake with a semiquantitative food-frequency questionnaire. Twelve studies were conducted in the United States, 3 in Norway, 1 in Portugal, 1 in Sweden, and 1 in Italy. The characteristics of these studies are listed in Table 1 .
| Study, year | Study design | Country, Study cohort | Disease outcome | Participants (cases) | Follow-up (years) | Age (years) | Category | RR (95%CI) for highest versus lowest category |
|---|---|---|---|---|---|---|---|---|
| He et al. 2010 | Cohort | United States Nurses’ Health Study | CVD | 7822 (295) | 26 | 30-55 | 32.6 g/d vs. 4.8g/d | 0.70(0.46-1.06) |
| Jacobs et al. 1999 | Cohort | United States Iowa Women’s Health Study | CVD, CHD | 38740 (1779) | 9 | 55-69 | 22.5 ser/week vs. 1.5 ser/week | 0.82(0.66-1.01) for CVD 0.82(0.63-1.06) for CHD |
| Jacobs et al. 1998 | Cohort | United States Iowa Women’s Health Study | IHD | 34492 (438) | 9 | 55-69 | 22.5 ser/week vs. 1.5 ser/week | 0.70(0.50-0.98) |
| Jacobs et al. 2001 | Cohort | Norwegian Norwegian County Study | CVD, CHD | 33848 (1311) | 11 | 35-56 | 2.25 -5.40 vs. 0.05 – 0.60 | 0.77(0.60-0.98) for CVD 0.76(0.56-1.02) for CHD |
| Jacobs et al. 2007 | Cohort | United States Iowa Women’s Health Study | CVD, CHD | 27312 (2934) | 17 | 55-69 | ≥19 ser/week vs. 0-3.5 ser/week | 0.73(0.62-0.86) for CVD 0.72(0.57-0.90) for CHD |
| Jensen et al. 2004 | Cohort | United States Health Professionals Follow-Up Study | CHD | 42850 (1818) | 14 | 40-75 | 42.4 g/d vs. 3.5g/d | 0.87(0.70-0.96) |
| Liu et al. 1999 | Cohort | United States Nurses’ Health Study | CHD | 75521 (761) | 10 | 38-63 | 2.7 ser/d vs. 0.13 ser/d | 0.79(0.62-1.01) |
| Liu et al. 2003 | Cohort | United States Physicians’ Health Study | CVD, MI | 86190 (1869) | 5.5 | 40-84 | ≥1 ser/d vs. Rarely | 0.80(0.66-0.97) for CVD 0.71(0.51-0.98) for MI |
| Lockheart et al. 2007 | Case-control | Norwegian – | MI | 211 (106) | — | 45-75 | 240 g/d vs. 94 g/d | 0.89(0.35-2.26) |
| Oliveira et al. 2010 | Case-control | Portugal – | MI | 3016 (820) | — | ≥18 | ≥ 6 g/d vs. < 6 g/d | 0.74(0.62-0.90) |
| Rautiainen et al. 2012 | Cohort | Sweden Swedish Mammography Cohort | MI | 32561 (1114) | 10 | 49-83 | ≥4.7 ser/d vs. ≤2.3 ser/d | 0.89(0.74-1.07) |
| Sahyoun et al. 2006 | Cohort | United States Community-living persons | CVD | 535 (89) | 10 | 60-98 | 2.9 ser/d vs. 0.31 ser/d | 0.48(0.25-0.96) |
| Steffen et al. 2003 | Cohort | United States Atherosclerosis Risk in Communities Study | CHD | 15792 (535) | 11 | 45-64 | 3 ser/d vs. 0.1 ser/d | 0.72(0.53-0.97) |
| Tavani et al. 2004 | Case-control | Italy – | MI | 1602 (558) | — | 18-79 | >2 ser/week vs. <2 ser/week | 1.3(0.9-1.8) |
Inverse associations of whole-grain intake and the risk for CHD were reported in 11 studies, and no significant association was reported in 7 studies. Pooled results suggested that the highest whole-grain intake amount compared with the lowest amount was significantly associated with reduced risk for CHD (summary RR 0.787, 95% CI 0.743 to 0.833), with no between-study heterogeneity observed (I 2 = 0%, p = 0.537) ( Figure 2 ).
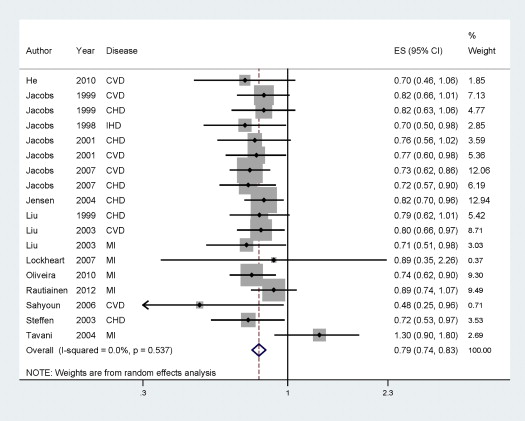
In subgroup analyses for study design, the pooled RRs of CHD for the highest category of whole-grain intake compared with the lowest category were 0.779 (95% CI 0.733 to 0.828) and 0.946 (95% CI 0.605 to 1.478) for cohort studies and case-control studies, respectively. When we conducted the subgroup analysis by geographic location, significant associations were found between whole-grain intake and CHD in the United States and Europe. In subgroup analyses for disease outcome, inverse associations of whole-grain intake and risk for CHD were found for CHD (summary RR 0.782, 95% CI 0.712 to 0.859) and CVD (summary RR 0.762, 95% CI 0.693 to 0.838), but not for myocardial infarction. When we conducted the subgroup analysis by follow-up duration (<10 and ≥10 years) and gender, the results was consistent with the overall data. The details results are summarized in Table 2 .
| Subgroups | No. (cases) | No. studies | RR (95% CI) | Heterogeneity test | |
|---|---|---|---|---|---|
| I 2 (%) | P-value | ||||
| All studies | 14427 | 18 | 0.787(0.743-0.833) | 0.0 | 0.537 |
| Study design | |||||
| Cohort | 12943 | 15 | 0.779(0.733-0.828) | 0.0 | 0.928 |
| Case-control | 1484 | 3 | 0.946(0.605-1.478) | 74.7 | 0.019 |
| Geographic locations | |||||
| America | 10518 | 12 | 0.767(0.716-0.821) | 0.0 | 0.935 |
| Europe | 3909 | 6 | 0.847(0.728-0.985) | 45.4 | 0.103 |
| CHD outcome | |||||
| CHD | 5383 | 6 | 0.782(0.712-0.859) | 0.0 | 0.934 |
| CVD | 5520 | 6 | 0.762(0.693-0.838) | 0.0 | 0.708 |
| MI | 3086 | 5 | 0.864(0.709-1.054) | 56.9 | 0.054 |
| Follow-up duration | |||||
| <10 | 4086 | 5 | 0.787(0.704-0.878) | 0.0 | 0.892 |
| ≥10 | 8857 | 10 | 0.776(0.722-0.834) | 0.0 | 0.739 |
| Sex | |||||
| Females | 7879 | 9 | 0.807(0.730-0.891) | 33.0 | 0.154 |
| Males | 3687 | 3 | 0.799(0.712-0.895) | 0.0 | 0.739 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


