We performed a systematic review and meta-analysis comparing the all-cause mortality outcomes of successful percutaneous coronary intervention (PCI) for chronic total occlusions (CTOs) with unsuccessful CTO-PCI, using a stent-based strategy. Multiple studies comparing successful CTO-PCI with unsuccessful CTO-PCI have reported variable outcomes. No systematic review or meta-analysis has been performed after stenting became the default strategy for CTO-PCI. Searching major electronic databases, 64 studies were identified using the keywords “CTO,” “PCI,” and “mortality.” Using the Preferred Reporting Items for Systematic Reviews and Meta-analyses method, 13 studies met the criteria for inclusion in the present meta-analysis. The short-term (≤30 days) and long-term (≥1 year) mortality outcomes were analyzed comparing successful CTO-PCI and unsuccessful CTO-PCI. Coronary perforation and its association with CTO-PCI success was analyzed. A significant reduction in short-term mortality was noted with successful CTO-PCI compared to unsuccessful CTO-PCI (odds ratio 0.218, 95% confidence interval 0.095 to 0.498, Z = −3.61, p <0.001). A similar, significant reduction in long-term mortality was noted with successful CTO-PCI compared to unsuccessful CTO-PCI (odds ratio 0.391, 95% confidence interval 0.311 to 0.493, Z = −7.957, p <0.001). A significant association was present between coronary perforation and unsuccessful CTO-PCI (odds ratio 0.168, 95% confidence interval 0.104 to 0.271, Z = −7.333, p <0.001). In conclusion, successful CTO-PCI using a predominantly stent-based strategy is associated with a significant reduction in short- and long-term mortality compared to unsuccessful CTO-PCI. Coronary perforation was associated with CTO-PCI failure.
Recanalization of coronary chronic total occlusions (CTOs) using percutaneous catheter-based techniques has been called the “final frontier” of interventional cardiology. Its role in relieving symptoms attributable to the occlusion is intuitive, although its effect on the short- and long-term prognosis is not entirely clear. The procedural success rates of percutaneous coronary intervention (PCI) for CTOs have improved during the past several years, with improvements in operator experience and skill and technological advances, such as the increased availability of taper-tipped guidewires with better torque control and devices such as microcatheters, tornus catheters, and so forth. The advent and increase in application of the retrograde recanalization technique has also led to an increase in the CTO-PCI success rates. A previous meta-analysis revealed improved outcomes of those patients with CTOs who were successfully revascularized versus those in whom percutaneous recanalization was not successful, although had significant heterogeneity across populations, outcomes and modality of PCI. Also since that analysis was reported, significant advances have occurred in CTO-PCI techniques and technology, increasing procedural success and improving long-term patency by the increase in the use of coronary stents. We report the findings of a meta-analysis of published data, reporting the all-cause mortality outcomes of patients undergoing CTO-PCI with a predominantly stent-based strategy.
Methods
Our meta-analysis followed the method outlined in the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) statement. We searched the indexed studies using major databases, including PubMed, the Cochrane Library, and Google Scholar. The keywords included “chronic total occlusion,” “percutaneous coronary intervention,” and “outcomes.” Abstracts from major interventional cardiology meetings were searched using the same keywords.
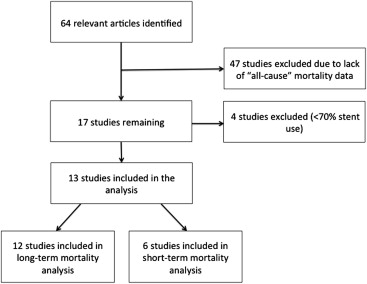
The titles and abstracts of 64 relevant studies were identified through the data search and reviewed independently by 3 investigators (S.P., P.B., and T.K.) to determine whether they met the eligibility criteria for inclusion. Discrepancies regarding whether to include or exclude a study were resolved by consensus with the other investigators (T.P. and I.A.).
Studies were eligible for inclusion in the analysis if a comparison between successful CTO-PCI and unsuccessful CTO-PCI using a stent-based strategy had been done and the all-cause mortality outcomes were reported. Studies with percutaneous transluminal coronary angioplasty alone without stenting or using stents in <70% of patients were excluded. Studies reporting cardiac mortality alone were also excluded. All-cause mortality was used as the end point, because some of the attributes of CTO-PCI, such as greater radiation exposure and contrast burden, can affect noncardiac mortality.
All data were independently abstracted by 3 investigators (S.P., P.B., and T.K.) using a standardized data collection form. Discrepancies were resolved through discussion with the other investigators (T.P., I.A.) and through reference to the original studies. We attempted to contact the study investigators for additional information when necessary. All-cause mortality data were collected, including short-term mortality (defined as ≤30 days after PCI) and long-term mortality (defined as ≥1years after PCI). In studies reporting mortality outcomes >1 year, the events at 2 years of follow-up were included in the analysis. This allowed us to eliminate some of the heterogeneity induced by the variable duration of follow-up.
The baseline characteristics for both groups were extracted from the studies and included age, gender, history of diabetes mellitus, history of myocardial infarction, and left ventricular ejection fraction. The proportions were calculated and weighted by study size. Absolute numbers of mortality events were used and, if not reported, were calculated from the percentages and, in 2 instances, were extracted from the survival curves.
The numbers of events and total number of patients in the successful and unsuccessful CTO-PCI groups were entered into the Comprehensive Meta-Analysis software (Biostat, Englewood, New Jersey). The short- and long-term mortality events were analyzed separately. Heterogeneity was assessed using the I 2 test, and an I 2 <25% was considered low heterogeneity. The results are reported as odds ratios (ORs) and 95% confidence intervals (CIs). Publication bias was assessed using the Begg-Mozumdar method, and funnel plots were generated.
Results
The search resulted in 64 studies. Of the 13 studies included in the present analysis, 6 had reported the mortality outcomes at ≤30 days of follow-up, and 12 studies had reported the mortality outcomes at ≥1 year of follow-up for patients with successful versus unsuccessful CTO-PCI. Of the 13 studies, 6 studies were prospective and 7 studies were retrospective. The studies reported by Suero et al and Safley et al were excluded, because a small (<10%) fraction of the total patients undergoing successful CTO intervention had received stents. The study by Prasad et al was excluded, because the data comparing successful versus unsuccessful CTO-PCI in the “stent era” were not reported separately. This process is graphically displayed in Figure 1 .
The study characteristics and baseline demographic and co-morbidity data of the included study populations are listed in Table 1 . CTO-PCI was successful in 70.8% of all patients. Stents were used in >70% of patients in all included study populations, with an average of 93.4% of patients receiving stents.
| Study | Mean Follow-up (yr) | Study Type | Stents (DES) | CTO (n) | Age (yr) | Men | Previous MI | Diabetes | EF (%) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| S | U | S | U | S | U | S | U | S | U | S | U | ||||
| Olivari et al, 2003 | 1 | P | 89.7% | 289 | 87 | 58 ± 9.9 | 59.4 ± 10.9 | 86% | 85% | 69% | 69% | 17% | 20% | 55.7 ± 9.6 | 56.3 ± 10.1 |
| Hoye et al, 2005 | 4.5 | R | 81% | 567 | 304 | 59.6 ± 10.8 | 60.5 ± 10.4 | 74% | 72% | 55% | 49% | 12% | 9.1% | — | — |
| Drozd et al, 2006 | 2.5 | R | 100% | 298 | 161 | 57 ± 9.6 | 57.7 ± 9.89 | 81% | 80% | 73% | 66% | 11% | 11% | — | — |
| Aziz et al, 2007 | 1.7 | R | 97.7% (17.3%) | 377 | 166 | 58.8 | 58.8 | 76% | 81% | 58% | 58% | 14% | 9% | 53.1 | 52.7 |
| Arslan et al, 2006 | 2.8 | R | 91.5% | 117 | 115 | 61.1 ± 10.4 | 60.3 ± 10.6 | 75% | 75% | 40% | 45% | 26% | 24% | 50 ± 13.8 | 49.7 ± 14.5 |
| Valenti et al, 2008 | 2 | R | 100% (100%) | 344 | 142 | 67.2 ± 11.2 | 69.8 ± 10.9 | 81% | 83% | 45% | 54% | 24% | 21% | 42 ± 13 | 41 ± 14 |
| de Labriolle et al, 2008 | 2 | P | 93.7% (84%) | 127 | 45 | 60.6± 11.6 | 63.6 ±10.1 | 72% | 87% | 21% | 22% | 19% | 41% | 50 ± 12 | 48 ± 15 |
| Chen et al, 2009 | 3 | P | 95.5% (100%) | 132 | 20 | 63.9 ± 14.7 | 67.68 ± 7.29 | 74% | 80% | 46% | 65% | 26% | 25% | 45 ± 11 | 42 ± 16 |
| Rathore et al, 2009 | In-hospital | R | 74.3% | 791 | 113 | 65.4 ± 10.7 | 66.01 ± 11.2 | 82% | 83% | 86% | 88% | 40% | 37% | — | — |
| Mehran et al, 2011 | 2.9 | P | 94.6% (66%) | 1,226 | 565 | 61.2 ± 10.7 | 62.1 ± 10.4 | 85% | 89% | 47% | 56% | 23% | 22% | 53.8 ± 10 | 52.6 ± 10.7 |
| Jolicouer et al, 2011 | 5.6 | R | 99.6% (51.6%) | 213 | 133 | 58 | 61 | 70% | 79% | 21% | 29% | 33% | 26% | 56 | 55 |
| Lee et al, 2011 | 3.6 | P | 100% (100%) | 251 | 82 | 59.2 ± 10.5 | 63.8 ± 9.2 | 77% | 23% | 18% | 29% | 31% | 31% | 56.2 ± 9.9 | 55 ± 11.2 |
| Jones et al, 2012 | 3.8 | P | 97% (76%) | 582 | 254 | 62.4 ± 11.5 | 63.7 ± 11.2 | 76% | 79% | 32% | 36% | 27% | 29% | 55.6 ± 9.2 | 53.5 ± 1.4 |
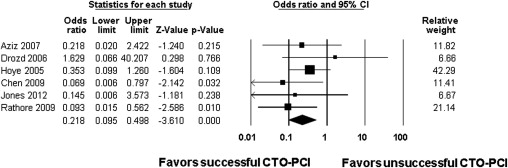
A Forest plot for short-term mortality analysis (total n = 3,932) is shown in Figure 2 . There were 9 deaths in the successful CTO-PCI group (n = 2,874) compared to 14 deaths in the unsuccessful CTO-PCI group (n = 1,058). A 78% relative risk reduction was observed with successful CTO-PCI (OR 0.218, 95% CI 0.095 to 0.498, Z-value = −3.61, p <0.001). The I 2 value was 0.00, consistent with low heterogeneity. The fixed-effects method was used.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


