Studies examining coronary computed tomographic angiography (CCTA) have demonstrated increased mortality related to coronary artery disease (CAD) severity but are limited to relatively nondiverse ethnic populations. The aim of this study was to evaluate the prognostic significance of CAD on CCTA according to ethnicity for patients without previous CAD in a prospective international CCTA registry of 11 sites (7 countries) who underwent 64-slice CCTA from 2005 to 2010. CAD was defined as any coronary artery atherosclerosis and obstructive CAD as ≥50% stenosis. All-cause mortality and nonfatal myocardial infarction (MI) were assessed by ethnicity using Kaplan-Meier and Cox proportional hazards, controlling for baseline risk factors, medications, and revascularization. A total of 16,451 patients of mean age 58 years (55% men) were followed over a median of 2.0 years (interquartile range 1.4 to 3.2). Patients were 60.1% Caucasian, 34.4% East Asian, and 5.5% African. Death or MI occurred in 0.5% (38 of 7,109) among patients with no CAD, 1.6% (91 of 5,600) among those with nonobstructive CAD, and 3.8% (142 of 3,742) among those with ≥50% stenosis (p <0.001 among all groups). The annualized incidence of death or MI comparing obstructive to no obstructive CAD among Caucasians was 2.2% versus 0.7% (adjusted hazard ratio [aHR] 2.77, 95% confidence interval [CI] 1.73 to 4.43, p <0.001), among Africans 4.8% versus 1.1% (aHR 6.25, 95% CI 1.12 to 34.97, p = 0.037), and among East Asians 0.8% versus 0.1% (aHR 4.84, 95% CI 2.24 to 10.9, p <0.001). Compared to other ethnicities, East Asians had fewer than expected events (aHR 0.25, 95% CI 0.16 to 0.38, p <0.001). In conclusion, the presence and severity of CAD visualized by CCTA predict death or MI across 3 large ethnicities, whereas normal results on CCTA identify patients at very low risk.
Coronary computed tomographic angiography (CCTA) has emerged as a highly accurate and prognostically useful noninvasive test for the diagnosis or exclusion of coronary artery disease (CAD). Although CCTA has been evaluated in large patient cohorts, there is sparse information about its ability to predict future cardiovascular events across ethnic subgroups. The assessment of CAD using CCTA in patients of different genetic and environmental backgrounds is important because it is proposed that the pathology, epidemiology, and prognosis of CAD may vary across ethnicities. Given the limited data currently available on coronary computed tomographic angiographic findings and their prognostic implications stratified by ethnicity, we sought to examine the prevalence of cardiovascular risk factors and the prognostic value of CCTA among ethnic subgroups in a large, prospective, multicenter international CCTA registry.
Methods
The Coronary CT Angiography Evaluation for Clinical Outcomes: An International Multicenter (CONFIRM) registry is an ongoing, prospective, international, multicenter registry designed to evaluate the relation of coronary atherosclerosis and clinical risk factors to adverse outcomes among patients who have undergone at least 64-slice CCTA for clinically referred indications ( ClinicalTrials.gov identifier NCT01443637 ). The rationale and design of the CONFIRM registry have been previously reported. In brief, the registry uses an identical standardized data collection form and data dictionary at all participating sites to prospectively collect baseline risk factors, symptoms, and medications before CCTA, as well as detailed coronary computed tomographic angiographic results and clinical outcomes. Patient symptoms were assessed before they underwent CCTA and defined using the criteria of Diamond and Forrester according to American College of Cardiology guidelines for chest pain assessment, and pretest cardiovascular risk was defined using the Morise score. Ethnicity was assessed by investigators at the time of CCTA and coded as Caucasian, African, Hispanic, East Asian, Middle Eastern, South Asian, or other. Patients with known previous CAD (previous myocardial infarction [MI], percutaneous coronary intervention, or coronary artery bypass surgery) were excluded from this analysis. Phase 1 of the CONFIRM registry enrolled 27,125 patients at 12 cluster sites in 6 countries in North America, Europe, and Asia. Phase 2 of the registry enrolled 4,682 patients from 5 sites in 4 countries. The study protocol was approved by all centers’ institutional review boards, and when required, all patients provided written informed consent.
CCTA was performed using a single- or dual-source ≥64-slice computed tomographic scanner according to Society of Cardiovascular Computed Tomography guidelines by highly experienced imagers, as previously described. Coronary atherosclerotic lesions were graded as normal (no atherosclerosis), mild (1% to 49% stenosis), or obstructive (≥50% stenosis) in epicardial coronary arteries of ≥2 mm in diameter.
The primary end point was time to all-cause death or nonfatal MI. Patient follow-up was performed as approved at each local participating institution using telephone interviews, available medical records, contact with attending physicians, mailed questionnaires, and, where available, a national death registry. From within the entire CONFIRM registry, only patients with complete information regarding ethnicity, severity of CAD on CCTA, and clinical follow-up for the outcomes of all-cause mortality and nonfatal MI after CCTA were included in this analysis.
Continuous variables are presented as mean ± SD or as median (interquartile range), as appropriate. Categorical variables are presented as frequencies with percentages. Means were compared using Student’s t tests or Mann-Whitney U tests, and intergroup comparisons were assessed using analysis of variance or Kruskal-Wallis tests, as indicated. Proportions were compared using chi-square tests. Ethnicity was evaluated for the prediction of ≥50% stenosis using logistic regression in univariate analysis and multivariate analysis controlling for baseline cardiovascular risk. All-cause mortality and nonfatal MI were assessed using Kaplan-Meier and Cox proportional hazards to calculate adjusted hazard ratios, controlling for baseline cardiovascular risk factors. Cardiovascular risk factors and symptoms were adjusted in multivariate analysis using a composite Morise score. Failure events modeled included a combined major adverse cardiovascular event end point that included all-cause death and nonfatal MI. The same analysis as performed for the entire cohort was conducted stratified by ethnicity. Univariate predictors based on known cardiovascular risk factors were evaluated, including age, gender, diabetes, hypertension, hyperlipidemia, and current smoking. In addition, differences in baseline medication use and the occurrence of coronary revascularization performed <90 days after CCTA (presumably driven by the results of CCTA) were explored and also used to account for potential ethnicity-related differences in patient management. Hazard ratios were first calculated in a Cox proportional-hazards model limited to each ethnicity, and then each ethnicity was compared to all other ethnicities in a multivariate model, adjusted for baseline symptoms and risk factors (Morise score), baseline medications (aspirin, statins, and antihypertensive medications), and coronary revascularization. Model overfitting procedures were carefully considered and postestimation analysis was performed to ensure that the proportional-hazards assumption was met. Excess risk was calculated, after adjusting the hazard ratio for ≥50% CAD for baseline symptoms and risk factors, within each ethnic subgroup for the prediction of major adverse cardiovascular events. Excess risk was defined as 1 – (ln HR A /ln HR u ), where HR u is the unadjusted hazard ratio and HR A is the risk-adjusted hazard ratio (using the Morise score). All p values are 2 sided, with significance set at p <0.05. Statistical analysis was conducted using STATA version 11 (StataCorp LP, College Station, Texas) and SPSS version 13.0 (SPSS, Inc., Chicago, Illinois).
Results
Ethnicity data were coded for 16,451 patients at 11 sites (7 countries). The mean age was 58 ± 12 years (55% men), and patients were followed over a median of 2.0 years (interquartile range 1.4 to 3.2 years). Middle Eastern (n = 67), South Asian (n = 72), Hispanic (n = 534), and other (n = 127) ethnicities were each coded during data collection but were excluded because they were individually underpowered for analysis. Baseline demographics are listed in Table 1 . Patients were 60.1% Caucasian, 34.4% East Asian, and 5.5% African. There were significant differences in baseline risk factors, symptoms, and baseline medication use across all ethnic subgroups. Caucasians and East Asians were more likely to be older and male. East Asians had the highest prevalence of diabetes (26.9%) and Morise scores, the highest use of baseline statins and aspirin, but the lowest prevalence of a family history of premature CAD. Coronary revascularization performed <90 days after CCTA was significantly more frequent in Caucasians (7.99%) than East Asians (6.52%) and Africans (2.56%) (p <0.001; Table 1 ). When restricted to only patients with any obstructive disease on CCTA, these relative differences in coronary revascularization decreased but remained significant: Caucasians (32.4%) versus East Asians (28.5%) versus African (24.7%) (p = 0.033).
| Variable | Caucasian (n = 9,898) | East Asian (n = 5,654) | African (n = 899) | Total (n = 16,451) | p Value |
|---|---|---|---|---|---|
| Age (yrs) | 57.9 ± 12.1 | 58.9 ± 10.7 | 52.4 ± 12.7 | 57.9 ± 11.7 | <0.001 |
| Men | 57.2% | 55.0% | 39.6% | 55.5% | <0.001 |
| Body mass index (kg/m 2 ) | 27.9 ± 5.4 | 25.0 ± 3.0 | 31.1 ± 6.5 | 27.1 ± 5.1 | <0.001 |
| Hypertension ∗ | 48.1% | 51.9% | 63.5% | 50.3% | <0.001 |
| Diabetes mellitus | 11.2% | 26.9% | 18.5% | 17.0% | <0.001 |
| Hyperlipidemia ∗ | 53.4% | 55.3% | 41.7% | 53.4% | <0.001 |
| Family history of premature CAD | 39.5% | 9.3% | 32.9% | 28.8% | <0.001 |
| Smokers | 19.2% | 14.1% | 16.9% | 17.4% | <0.001 |
| Anginal status | |||||
| Asymptomatic | 39.0% | 33.5% | 26.3% | 36.5% | <0.001 |
| Nonanginal | 14.5% | 4.7% | 4.9% | 10.7% | <0.001 |
| Atypical | 36.1% | 46.3% | 58.2% | 40.7% | <0.001 |
| Typical | 10.4% | 15.5% | 10.6% | 12.1% | <0.001 |
| Morise score | 12.9 ± 4.0 | 13.5 ± 3.6 | 11.5 ± 4.8 | 13.0 ± 4.0 | <0.001 |
| Baseline statin | 30.4% | 42.5% | 29.7% | 36.1% | <0.001 |
| Baseline aspirin | 33.0% | 51.2% | 37.5% | 40.9% | <0.001 |
| Baseline antihypertensive medication | 46.7% | 59.4% | 64.4% | 52.7% | <0.001 |
| Coronary revascularization † | 7.99% | 6.52% | 2.56% | 7.18% | <0.001 |
∗ Hypertension and hyperlipidemia were ascertained at the time of CCTA and confirmed, when available, with patient medical records for these diagnoses, medical therapy of such diagnoses, or blood pressure >140/90 mm Hg and total cholesterol >240 mg/dl, respectively.
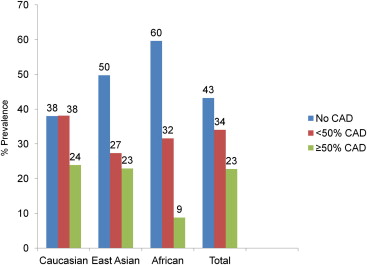
The unadjusted prevalence of CAD on CCTA according to ethnicity is shown in Figure 1 . Caucasians and East Asians had a significantly higher prevalence (24% and 23%, respectively) of obstructive disease (worst stenosis ≥50%) compared to Africans (9%) (p <0.0001). The univariate hazards ratios for obstructive disease were 1.20 (95% confidence interval [CI] 1.12 to 1.28) for Caucasians (p <0.001), 0.40 (95% CI 0.33 to 0.49) for Africans (p <0.001), and 0.98 (95% CI 0.91 to 1.06) for East Asians (p = 0.60). Adjusting for baseline Morise score and using Caucasian as the index ethnicity, the adjusted hazard ratios for obstructive disease were 1.0 (95% CI 0.90 to 1.10) for East Asians (p = 0.96) and 0.33 (95% CI 0.25 to 0.44) for Africans (p <0.001).
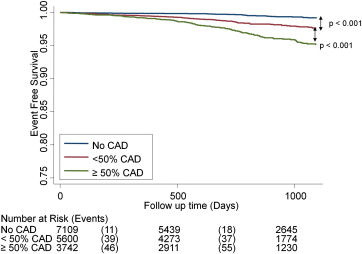
Univariate Kaplan-Meier survival curves for death and nonfatal MI among the entire 16,451-patient cohort are shown in Figure 2 . There was significantly decreased event-free survival among patients with nonobstructive and obstructive CAD on CCTA compared to patients with no coronary atherosclerosis. Clinical outcomes including absolute number of all-cause mortality and nonfatal MI events among each ethnicity, unadjusted for baseline Morise score or follow-up duration, are listed in Table 2 . The unadjusted annualized incidence rates for death and MI according to ethnicity and presence versus the absence of ≥50% stenosis on CCTA are shown in Figure 3 . Compared to patients without obstructive CAD, the presence of obstructive CAD on CCTA conferred a significantly increased rate of death or nonfatal MI among Caucasians, East Asians, and Africans (p <0.05 for all ethnicities). Patients of African ethnicity had the highest relative increase in the combined rate of death or MI related to the presence of obstructive CAD compared to those without obstructive CAD (3.76%, 95% CI −0.15% to 7.66%) on CCTA (p = 0.007 for comparison to other ethnicities).
| Ethnicity | Adverse Event | Coronary Narrowing (Diameter Stenosis) | |||||
|---|---|---|---|---|---|---|---|
| None | <50% | ≥50% | |||||
| n | % | n | % | n | % | ||
| Caucasian (n = 9,898) | Death | 24 | 0.64 | 56 | 1.49 | 65 | 2.75 |
| Nonfatal MI | 3 | 0.08 | 26 | 0.69 | 50 | 2.11 | |
| East Asian (n = 5,654) | Death | 8 | 0.28 | 5 | 0.32 | 24 | 1.85 |
| Nonfatal MI | 0 | 0.00 | 3 | 0.19 | 4 | 0.31 | |
| African (n = 899) | Death | 2 | 0.37 | 7 | 2.46 | 4 | 5.06 |
| Nonfatal MI | 2 | 0.37 | 2 | 0.70 | 3 | 3.80 | |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


