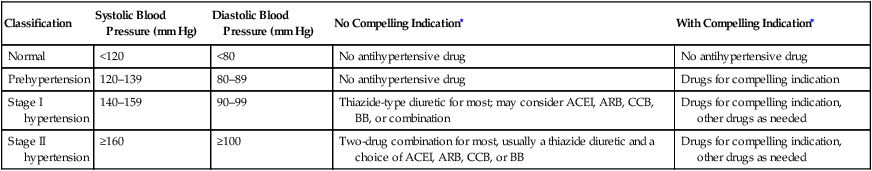
The distinction between a transient ischemic attack (TIA) and stroke is made by duration of symptoms: The duration of a TIA is less than 24 hours. A TIA is a harbinger of stroke in up to 17% of patients, most often during the first week after the event. Ischemic stroke accounts for 88% of all strokes. Classic subtypes of stroke have been well defined (Box 1). More than 75% of strokes are first events, allowing an opportunity for meaningful intervention. The risk for stroke and TIA is affected by various modifiable and nonmodifiable risk factors (Box 2). Treatment recommendations have been established (Table 1). TABLE 1 Medical Risk Factor Modification for Primary Stroke Prevention BP, Blood pressure; HbA1c, hemoglobin A1c; LDL, low-density lipoprotein cholesterol. Hypertension is related to stroke in a graded, continuous manner, and stroke risk is increased even when blood pressure levels are considered normal by current guidelines. Patients with prehypertension should be encouraged to control their pressure with nonpharmacologic lifestyle measures. The Joint National Committee (JNC) 7 guidelines for the classification and treatment of hypertension have been published (Table 2). TABLE 2 Classification and Treatment of Blood Pressure ∗Lifestyle modifications are encouraged for all and include weight reduction for overweight patients, limitation of ethanol intake, increased aerobic physical activity (30–45 minutes daily), reduction of sodium intake (2.34 g), maintenance of adequate dietary potassium (120 mmol/day), smoking cessation, and DASH diet (rich in fruits, vegetables, and low-fat dairy products and reduced in saturated and total fat). From Goldstein LB, Bushnell CD, Adams RJ, et al: Guidelines for the primary prevention of stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association, Stroke 42:517–584, 2011. Used with permission. ©2011 American Heart Association, Inc. EDIC (Epidemiology of Diabetes Interventions and Complications), the long-term follow-up of the DCCT (Diabetes Control and Complications Trial) examined the long-term effects of intensive glycemic control in patients with type 1 DM. Intensive treatment was administered as part of the DCCT over 6.5 years, and in EDIC patients were all treated in a similar, intensive, fashion. After 11 years of follow-up, patients who had received prior intensive treatment had a 57% reduced combined cardiovascular event rate including myocardial infarction, stroke, and death from a cardiovascular cause. In addition to controlling diabetes, other cardiovascular risk factors should be managed aggressively in diabetic patients (see Table 1). Antiplatelet agents have not been consistently shown to be of value for primary prevention of stroke in patients with diabetes and are discussed in more detail later.
Medical Treatment to Prevent Transient Ischemic Attacks and Ischemic Stroke
Modification of Risk Factors
Risk Factor
Recommendation
Comment
Hypertension
BP <140/90 mm Hg
BP lowering is more important than choice of medication; diabetic patients may benefit from further BP reduction
Diabetes mellitus
Multifactor risk factor modification may be better than focusing on targeting glucose alone
HbA1c <7% has not been shown to reduce risk of stroke
Hyperlipidemia
Patients with elevated cholesterol, atherosclerosis anywhere: LDL <100 mg/dL
Diabetics: LDL <70 mg/dL
First line: statins
Second line: bile-acid sequestrants and niacin
Tobacco abuse
Combined pharmacologic and behavioral smoking-cessation therapy
Lack of direct evidence
Hypertension
Classification
Systolic Blood Pressure (mm Hg)
Diastolic Blood Pressure (mm Hg)
No Compelling Indication∗
With Compelling Indication∗
Normal
<120
<80
No antihypertensive drug
No antihypertensive drug
Prehypertension
120–139
80–89
No antihypertensive drug
Drugs for compelling indication
Stage I hypertension
140–159
90–99
Thiazide-type diuretic for most; may consider ACEI, ARB, CCB, BB, or combination
Drugs for compelling indication, other drugs as needed
Stage II hypertension
≥160
≥100
Two-drug combination for most, usually a thiazide diuretic and a choice of ACEI, ARB, CCB, or BB
Drugs for compelling indication, other drugs as needed
Diabetes Mellitus
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Thoracic Key
Fastest Thoracic Insight Engine
