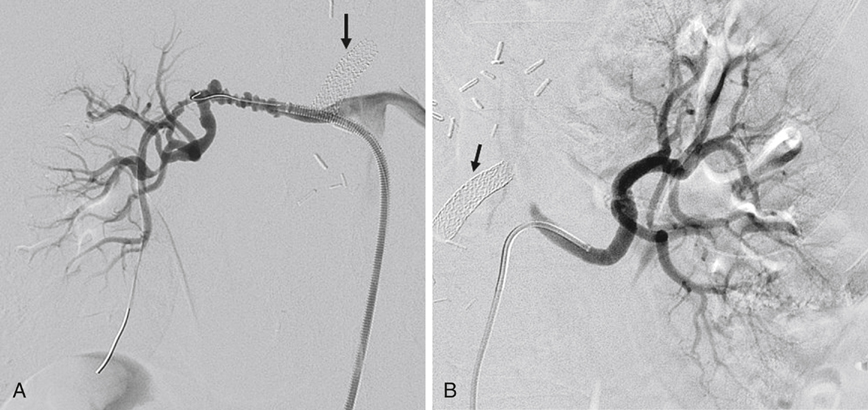
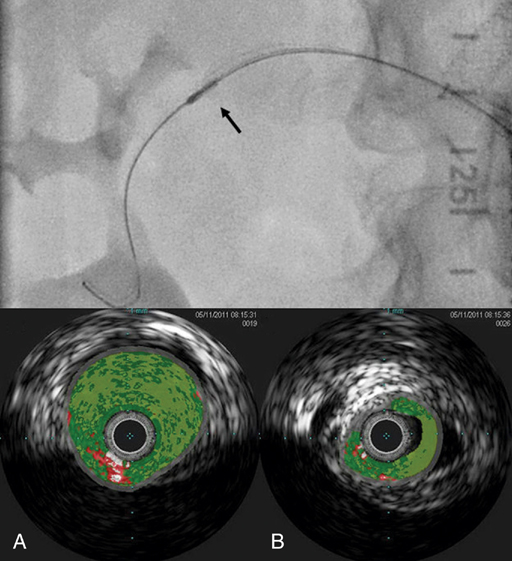
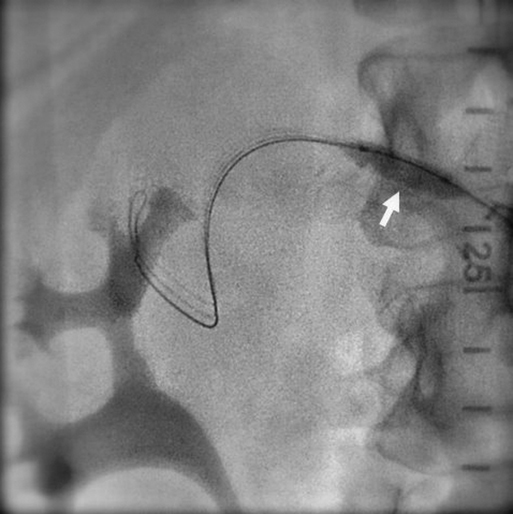
Javier E. Anaya-Ayala, Daynene Vykoukal, Alan B. Lumsden and Mark G. Davies Percutaneous transluminal renal angioplasty (PTRA) has become the treatment of choice for patients with renal artery FMD that is limited to the main renal artery (Figures 1 to 4). The majority of these patients have medial fibroplasia. Before the advent of percutaneous transluminal angioplasty, open surgical revascularization was the primary therapeutic modality for these patients. Overall, the technical success rates of the open surgical approach ranged from 89% to 97%; arterial hypertension was cured in approximately 33% to 63% of patients and improved in 24% to 57%. Several factors such as prolonged duration of hypertension, concomitant atherosclerotic disease, and complex branch-vessel repair can all adversely affect the outcomes of surgical revascularization. Although stents have been used extensively to treat atherosclerotic renal artery stenosis, the use of these devices for FMD has been reserved as a bailout procedure in cases in which there are suboptimal results with balloon angioplasty or in which renal artery dissection occurs.
Percutaneous Arterial Dilation for Fibrodysplastic Renovascular Hypertension
Treatment
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



