Dilatation of the superficial veins and/or venules of the leg, referred to as varicose veins, is the most common disorder of the superficial venous system of the lower extremity. This is a highly prevalent disorder, particularly in industrialized countries, with estimates of prevalence varying from 2% to 56% for males and 1% to 73% for females. Despite these facts, superficial venous disease receives relatively little attention in medical school curricula and during residency training (1–3). This chapter will summarize the anatomy of the superficial venous system, describe the pathogenesis of varicose veins, and provide an overview of the interventional therapies for the treatment of superficial venous disease.
LOWER EXTREMITY VENOUS ANATOMY
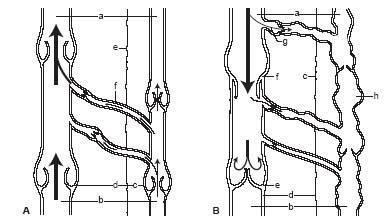
The venous system of the lower extremity can be divided into three different systems (Fig. 30.1):
- the deep venous system that runs close to the tibia and the femur in the deep compartments;
- the superficial venous system that runs in the superficial compartments;
- the perforating veins or communicating veins that connect the superficial venous system to the deep venous system.
The deep venous system within the calf is composed of paired anterior tibial, posterior tibial, and peroneal veins that run parallel to the respective arteries. Soleal and gastrocnemius veins are the sinusoidal veins within the muscular compartment of the calf. All the calf veins drain into the popliteal vein below the level of the knee. The popliteal vein then ascends to become the femoral vein (previously called the “superficial femoral vein,” a term that has been abandoned) (4). The profunda femoral vein joins the femoral vein to become the common femoral vein below the inguinal ligament.
The superficial system is mainly composed of the great saphenous vein (GSV) and the small saphenous vein (SSV) (4). These start on the medial and lateral aspects of the superficial dorsal venous arch of the foot, respectively. The GSV courses anterior to the medial malleolus on to the medial aspect of the calf and knee and then to the anteromedial thigh to join the common femoral vein just below the inguinal ligament. Proximal to the confluence of the GSV and the saphenofemoral junction, the anterior accessory saphenous vein (AASV) and posterior accessory saphenous vein (PASV) collecting the blood from the anterior thigh and posterior thigh, respectively, drain into the GSV. There is variability in the anatomy of this confluence. This anatomy is important to understand in order to avoid complications during endoluminal ablative procedures. The SSV courses behind the lateral malleolus and ascends posterior in the calf to join the popliteal vein behind the knee. Intersaphenous anastomoses can connect the GSV and SSV networks in the thigh or the leg, as illustrated in Figure 30.2. The most common of these is the Giacomini vein, which is found in the thigh and represents an extension of the SSV that joins the GSV.
The perforating veins connect the superficial venous system to the deep venous system. There are several perforators connecting the GSV and SSV to the deep venous system. There are medial ankle, calf, and thigh perforators connecting GSV to the deep veins and lateral calf perforators connecting the SSV to the deep veins.
NORMAL VENOUS BLOOD FLOW
Deoxygenated blood is collected from the skin and subcutaneous tissues by an extensive subpapillary vein network. This network drains into the reticular veins, which in turn drain into the larger superficial veins such as the GSVs and the SSVs. These veins lie in the low-pressure chamber of the superficial compartment of the leg and flow is directed proximally toward the saphenofemoral and saphenopopliteal junctions, respectively. The deep veins lie in the high-pressure deep compartment of the leg due primarily to the pumping action of the calf muscles directing blood back to the heart. Perforator veins penetrate the muscle fascia and provide a communication between the deep and superficial venous systems (Fig. 30.3A). Under normal circumstances, the valves in the perforating system prevent the high pressure from the deep venous system from being transmitted to the low-pressure superficial venous system. During relaxation of the calf muscles, blood may flow from the superficial to the deep venous system when the pressure in the deep system is temporarily lower than the superficial compartment. Vein valves maintain the direction of flow.
PATHOPHYSIOLOGY OF CHRONIC VENOUS INSUFFICIENCY AND DEVELOPMENT OF VARICOSE VEINS
The pathophysiology of superficial venous disease can be divided broadly into the following major categories:
- Reflux: Valvular incompetency within superficial, deep, or perforating veins can occur as either a primary event due to an inherent issue with the valve structure or secondary to dilatation of the vein wall. Reflux, as a primary cause, is more common in superficial veins rather than deep veins. Reflux results in monocyte-induced vein wall distension, retrograde flow, and distal venous hypertension within the involved veins.
- Obstruction: Thrombosis in deep or superficial veins can result in subsequent fibrosis or obstruction of the venous outflow. This can result in venous reflux distal to the obstruction and result in further damage of the vein valves. Thrombosis can also result in scarring of the vein valves (without obstruction or fibrosis) and cause secondary venous reflux. This syndrome is referred to as “post-thrombotic syndrome (PTS).” Chronic venous insufficiency due to reflux and obstruction is more difficult to manage than chronic venous insufficiency from either reflux or obstruction alone.
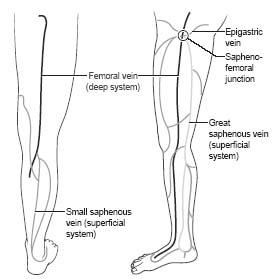
Figure 30.1 • Anatomy of superficial venous system of the lower extremity.
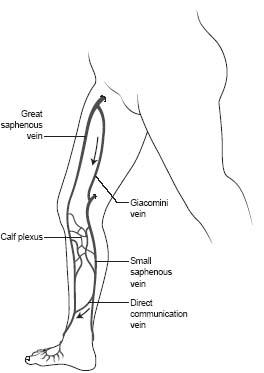
Figure 30.2 • Inter-saphenous communications between the great and small saphenous veins.
At a cellular level, venous hypertension causes white cell sequestration and activation and red cell sludging. This also results in capillary dilation, increased permeability, and protein leakage leading to edema. Hemosiderin deposition results in hyperpigmentation. Fibrin cuff formation is also seen in the interstitium. Subcutaneous thickening also results from fat necrosis and liposclerosis. Venous ulcerations eventually result if venous hypertension continues. Venous ulcerations are typically seen in the medial or lateral malleolar area. Reflux within the GSV generally results in ulceration over the medial malleolus ulceration, while reflux within the SSV results in ulceration over the lateral malleolus.
SIGNS, SYMPTOMS, AND CLINICAL HISTORY
Symptoms of venous claudication include aching, tiredness, heaviness, pain, throbbing, burning or stabbing sensation, or cramping in the affected extremity. These symptoms are generally associated with peripheral edema and some patients may have associated itching, restless legs, or numbness. The symptoms typically occur with prolonged standing and improve with leg elevation or walking.
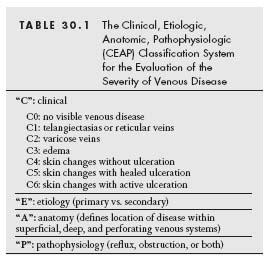
Objective scoring systems such as the Clinical, Etiologic, Anatomic, Pathophysiologic (CEAP) classification or the Venous Severity Scoring (VSS) have been used. The CEAP system developed by the American Venous Forum (5) is the most commonly used system (Table 30.1).
On examination, the earliest stages of venous disease may consist of reticular veins or telangiectasias. Telangiectasias are also called spider veins (Fig. 30.4A) and mostly these are asymptomatic but may represent underlying more extensive venous disease. Reticular veins (Fig. 30.4B), also known as feeder veins, are the dilated blue and green veins beneath the skin surface. Reticular veins are usually considered a cosmetic problem since these medium-sized veins generally do not lead to substantial medical symptoms or complications. Varicose veins are the larger ropelike veins that may be present in the great saphenous vein, small saphenous vein, AASV, and PASV (Fig. 30.4C). They may also be present as branch varicosities, particularly in patients several years after surgical stripping.
Figure 30.3 • A: Illustration of normal vein flow in the lower extremity (see text for details). (a) Proximal; (b) distal; (c) superficial compartment and vein; (d) deep compartment and vein; (e) muscle fascia; (f) flow from superficial to deep veins. B: Illustration of venous flow when chronic venous insufficiency occurs (i.e., abnormal flow from deep to superficial veins) (see text for details). (a) Proximal; (b) distal; (c) muscle fascia; (d) deep compartment and vein; (e) normal competent valve; (f) abnormal incompetent valve in deep venous system; (g) abnormal flow from the deep to the superficial vein; (h) abnormal dilated superficial vein. (Adapted from Beebe-Dimmer JL, Pfeifer JR, Engle JS, et al. The epidemiology of chronic venous insufficiency and varicose veins. Ann Epidemiol. 2005;15:175–184.)
An initial history should include documentation of the timing of the onset of varicosities to differentiate primary varicose veins versus secondary varicose veins. A history of deep venous thrombosis (DVT), superficial phlebitis, and trauma should be elicited. Any prior history of sclerotherapy, ablative therapy, and surgical therapy is important to note. Other systemic causes of leg edema and leg discomfort need to be ruled out. Appropriate assessment should be planned if other systemic causes of edema are noted. Realistic expectations must be discussed with the patient if other causes of edema are coexistent.
NON-INVASIVE VASCULAR TESTING
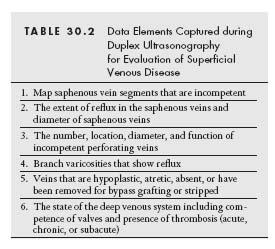
Non-invasive ultrasound plays a very important role in the assessment of superficial venous disease. Understanding and interpreting the duplex ultrasound findings prior to planning a procedure is crucial. In addition, duplex ultrasound is vital in guiding these procedures.
Table 30.2 summarizes the data elements that need to be captured during duplex ultrasound testing of superficial venous disease. This will help the interventionalist in determining the appropriate endoluminal procedure (s). A color duplex ultrasound machine should be used. A highfrequency linear array transducer of 7 to 13 MHz is the most appropriate probe for lower extremity superficial vein evaluation, but a curvilinear array transducer of 3.5 to 5 MHz may be needed for obese patients. B-mode machine images of the superficial (Fig. 30.5) and deep veins are obtained in both longitudinal and transverse views. Knowledge of variation in lower extremity vein anatomy and appearance on ultrasound is important (6).
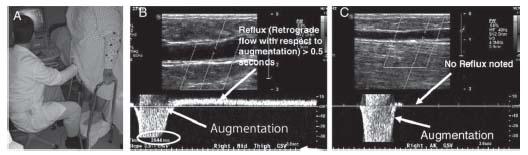
Venous Incompetence or Venous Reflux Testing
Incompetence within the vein can be tested with the patient positioned in the reverse Trendelenburg position, applying distal calf compression (i.e., provides augmentation of venous flow), and assessing for the presence of distal reflux. Distal reflux on ultrasound lasting more than 2 seconds is considered to be diagnostic of reflux in most laboratories. The Valsalva maneuver is also used to detect reflux. The diagnostic feature of reflux is the presence of distal flow in the vein during the Valsalva maneuver.
Figure 30.4 • A: Clinical appearance of spider veins or telangiectasias. B: Clinical appearance of reticular veins. C: Varicose vein in the distribution of the great saphenous vein.
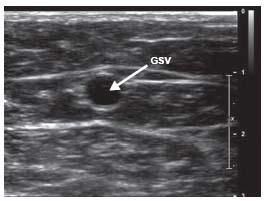
Figure 30.5 • Great saphenous vein (GSV) in transverse section within the saphenous fascia.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree