Management of Nonneoplastic Diseases of the Trachea
Robert E. Merritt
Douglas J. Mathisen
A wide spectrum of benign conditions that affect the trachea are described under the general headings of lesions that are caused by infection; posttraumatic lesions, including iatrogenic injuries; extrinsic lesions compressing the trachea; and miscellaneous, including a variety of lesions largely of unknown origin.
Infection
Tuberculosis
Tuberculosis of the upper airway appears principally to involve the lower trachea, main bronchi, or both. Acute ulcerative tuberculous tracheitis should be treated pharmacologically. As the acute inflammatory process resolves, a stenosis requiring surgical intervention may evolve. Typically, the stenosis shows a pattern of submucosal fibrosis occurring in a circumferential manner with marked narrowing or occlusion of the distal trachea and main bronchi. The tracheal cartilages appear to be grossly intact, although peribronchial or peritracheal fibrosis can occur. The lesions may be quite lengthy and thus present an enormous surgical challenge. Active tuberculosis should be completely treated and controlled before surgical resection and reconstruction is performed. Repeated dilation is the preferred method of treating inflammatory strictures. The use of stents (especially expandable) must be considered with caution because of the propensity to create granulations and further stricture formation. Gaissert15 described the complications caused by self-expanding metal stents used for benign tracheal strictures.
Histoplasmosis
Histoplasmosis may affect the airways in several ways. It may produce massive mediastinal fibrosis with involvement of the distal trachea, carina, and main bronchi, or it may involve principally the right bronchial tree in relation to the masses of lymph nodes in the right paratracheal and pretracheal area and in the middle lobe sump. The fibrosing process may extend centrally to involve the right pulmonary artery up to its point of origin even within the pericardium. The lesions may be a composite of airway compression plus intrinsic fibrotic involvement. Massive histoplasmoma at the carina may compress the airway. In such lesions there may be central caseation with a fibrotic capsule that actually involves one or both main bronchial walls intimately. Another presentation is with densely fibrotic and calcified subcarinal and precarinal lymph nodes, which may invade and erode through the wall of the trachea, carina, or bronchi. Broncholiths also occur peripherally in the lobar bronchi. Secondary infection and hemorrhage may follow. More recently, broncholithiasis in general has been associated with histoplasmosis rather than with tuberculosis, as it was in an earlier era. These clinical manifestations have been described by Mathisen and Grillo.33
The organism Histoplasma capsulatum is more often identified by special stains in pathologic material removed at surgery rather than on cultures. Organisms have been identified in fewer than 50% of patients who are presumed to have disease originating from this source. It has been theorized that the continuing fibrotic process is a reaction to products of the infection rather than to viable organisms. Thus, diagnosis is often presumptive, based on pathologic and radiologic findings as well as on a history of exposure and clinical evolution of the disease.
Other Inflammatory Disease Processes
A small number of patients have been seen who have suffered from diphtheria in childhood and presented many years later with tracheal stenosis or laryngotracheal stenosis. Because most of these patients had tracheostomies in infancy or early childhood for treatment of the acute disease, it is difficult to differentiate whether the late stenoses were caused by the disease or the treatment. Reconstruction may be possible.
Scleroma is a rare disease from infection with Klebsiella rhinoscleromatis that may involve the airways as well as the nasopharynx. It is found in Mexico and Central America. A rare case of necrosing mucormycosis involving the trachea or carina as well as the lungs may be seen in diabetic patients or in people who are immunosuppressed or undergoing chemotherapy, particularly for lymphomas. Prompt and radical surgical excision with vigorous and prolonged treatment with amphotericin may save some of these patients, as noted by Tedder and associates.42
Posttraumatic Lesions
Blunt Trauma
Ruptures of the trachea, carina, or main bronchi caused by blunt trauma may go unrecognized. Such patients almost always have a history of pneumothorax treated by tube drainage, often bilateral in the case of tracheal rupture. They present with shortness of breath or wheezing. The trachea or bronchus may be reduced to only a tiny opening when the diagnosis is made at last. Treatment consists of prompt excision of stenosis and surgical repair. When the bronchus is injured, every effort is made to salvage the distal lung. This is usually possible unless severe infection has developed in the airway. Deslauriers and associates10 have demonstrated adequate function of reimplanted lungs. Functional return appears to be roughly inversely proportional to the length of time that the lung was compromised.
In patients who have suffered tracheal separation caused by blunt injury in the neck and have been treated by tracheostomy only, total stenosis of the area of separation follows. Both recurrent laryngeal nerves are usually at least temporarily paralyzed and often permanently. Such patients must be evaluated carefully some months after their injury when the local inflammation has subsided. Laryngeal reconstruction, when necessary, with stabilization of the glottic aperture, is generally accomplished first. The larynx is then reconnected to the trachea, as described by Mathisen and Grillo.32 An effective although unmodulated voice is obtained. Pharyngoesophageal separation that was not repaired initially is reconstructed at the same time.
Inhalation Burns
Inhalation burns of the larynx, trachea, and bronchi are particularly difficult injuries to manage. The agent may have been chemical, thermal, or a combination of both. These patients often show little damage to the pharynx or supraglottic larynx once the immediate injury has subsided. Persistent damage often commences in the subglottis just below the vocal cords and extends down the airway in a gradually diminishing intensity of injury. The depth of injury and the length of airway injured probably relate to the dose received as well as to the actual injury potential of the agent. Gaissert and Grillo (14) found that in 18 patients treated for tracheal stenosis caused by inhalation injury, 14 had subglottic strictures as well and 2 had main bronchial stenosis. Although it is sometimes difficult to differentiate later injuries from the intubation with which the patients were treated acutely, three of our patients had laryngotracheal strictures without any history of intubation.
In most cases, the tracheal rings were not destroyed and the injuries were confined to various depths of mucosal and submucosal damage. Attempts at resection of injuries should not be made, especially in the early phase. First, involvement often commences immediately below the cords and involves the entire subglottic larynx, making repair almost impossible. Second, the burned airway responds poorly to early surgery, even where the lesion appears to be limited, much in the way that burned skin elsewhere in the body does (i.e., by the reformation of massive scarring). With appropriately placed splinting, silicone T-tubes, and a great deal of patience, a stable and open airway may usually be obtained in most of these patients in time. If resection is required, it should be deferred until the acute inflammatory response to airway injury has subsided completely.
Postoperative Stenosis
Stenosis of the trachea after tracheal reconstruction in most cases is caused by excessive tension on the anastomosis, and this is related to overzealous resection of too great a length of trachea. Dangerous tensions in tracheal resection may be reached at approximately above the 50% level of length of resection in the adult and above the 30% level in the child. Carinal resections are particularly at risk because of their complex nature. Patients chronically on high doses of prednisone are especially at risk if extensive tracheal resection is performed. Unnecessary disturbance of the blood supply to the trachea by extensive circumferential dissection also leads to stenosis or separation. Profuse, hypertrophic granulations at the anastomosis, which were seen when nonabsorbable sutures were used for tracheal repair, have vanished since the introduction of Vicryl sutures.
Stenosis of the airway also may result from radiation therapy and laser injury. Brachytherapy has contributed to a number of main bronchial stenoses. The contribution of laser therapy to tracheal damage is more difficult to assess because the laser is often applied for attempted treatment of preexisting lesions and in conjunction with a tracheostomy performed to safeguard the airway. Whereas laser injury may often be dealt with by subsequent resection and reconstruction, irradiation injuries may either be surgically uncorrectable when first seen or correctable only with considerable risk.
The special problem of obtaining healing after reconstruction in a previously irradiated trachea (when the dosage has exceeded 4,000 cGy approximately 1 year or more earlier) has been largely successfully met by advancement of an omental buttress, as described by Muehrcke and colleagues.37
Postintubation Damage
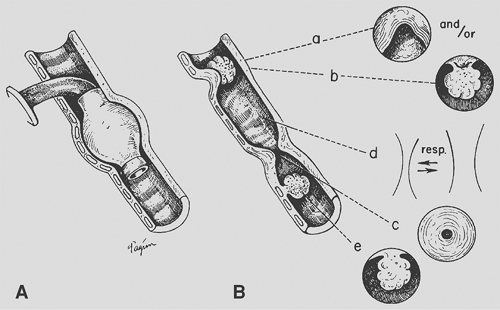
Intubation either with oral or nasal endotracheal tubes or with tracheostomy tubes is most commonly used to deliver mechanical ventilatory support in respiratory failure. Assistance supplied through cuffed tubes has thus far proved to be the only effective method of management for adults with poor pulmonary or chest wall compliance. High-flow respirators with uncuffed tubes, electrophrenic respirators, and negative-pressure tank respirators have not been satisfactory for managing these severe problems. High-frequency ventilation for long-term use remains developmental. A whole spectrum of tracheal lesions resulting from such treatment (Fig. 80-1) was discerned by Andrews and Pearson39 and by Grillo.17,18 The most common lesions and those most amenable to definitive treatment are those responsible for airway obstruction. Because a single patient may have more than one lesion and because the treatment of these lesions differs, precise definition of the pathologic state is essential in planning treatment.
Lindholm30 showed that endotracheal tubes may cause injury at the laryngeal level even after only 48 hours of intubation: glottic edema; vocal cord granulomas; erosions, particularly over the arytenoids; formation of granulation tissue; polypoid obstructions; and actual stenosis, particularly at the subglottic intralaryngeal level. Subglottic injury is produced also by cricothyroidotomy and by cricoid erosion caused by high tracheostomy in the presence of kyphosis. Subglottic stenosis may be more difficult to correct than tracheal stenosis.36
At the tracheostomy site, granulomas that can obstruct the airway may form during healing. If the tracheostomy stoma has
been made too large by turning a large flap or excising a large window in the initial tracheostomy, or if erosion is caused by sepsis and heavy prying equipment, cicatricial healing may produce an anterior A-shaped stenosis that can severely compromise the airway. The posterior wall of the trachea may be relatively intact in these patients. At the level of the inflatable cuff, whether placed on a tracheostomy tube or an endotracheal tube, circumferential erosion of the tracheal wall may occur. If this erosion is deep enough, all the anatomic layers of the trachea may be destroyed, so that cicatricial repair results in a tight circumferential stenosis (Fig. 80-2). Malacia may result also. Below this level, at the point where the tip of the tube may pry against the tracheal wall, additional erosion may occur with formation of granuloma, especially in children, for whom uncuffed tubes are used. In the segment between the stomal and cuff level, varying degrees of chondromalacia with resulting tracheomalacia may occur. Here, the cartilages are not totally destroyed but only thinned. Bacterial infection in this segment of the trachea during the period of ventilatory support probably contributes to this process.
been made too large by turning a large flap or excising a large window in the initial tracheostomy, or if erosion is caused by sepsis and heavy prying equipment, cicatricial healing may produce an anterior A-shaped stenosis that can severely compromise the airway. The posterior wall of the trachea may be relatively intact in these patients. At the level of the inflatable cuff, whether placed on a tracheostomy tube or an endotracheal tube, circumferential erosion of the tracheal wall may occur. If this erosion is deep enough, all the anatomic layers of the trachea may be destroyed, so that cicatricial repair results in a tight circumferential stenosis (Fig. 80-2). Malacia may result also. Below this level, at the point where the tip of the tube may pry against the tracheal wall, additional erosion may occur with formation of granuloma, especially in children, for whom uncuffed tubes are used. In the segment between the stomal and cuff level, varying degrees of chondromalacia with resulting tracheomalacia may occur. Here, the cartilages are not totally destroyed but only thinned. Bacterial infection in this segment of the trachea during the period of ventilatory support probably contributes to this process.
The etiologic basis of the cuff stenosis has been variously attributed to pressure necrosis by the cuff, the irritating quality of materials in rubber and plastic cuffs and tubes, irritant materials produced by gas sterilization, hypotension, and bacterial infection. Studies by Cooper and Grillo,4 and earlier by Florange and colleagues,13 of autopsy specimens of patients who had been on ventilators with inflated cuffs (Fig. 80-3), prospective studies of similar patients by Andrews and Pearson,1 and analysis of surgically removed lesions caused by cuffs and experimental reproduction of these lesions under controlled conditions by Cooper and Grillo,4,5 point to pressure necrosis as the principal etiologic agent. As Grillo and associates23 showed, if standard Rusch cuffs are inflated to just provide a seal at ventilatory pressures of approximately 25 cm H2O, intracuff pressures increase to 180 to 250 mm Hg. The trachea has an elliptic form, so it becomes deformed at the point where a seal is obtained. If perfusion pressures in the patient are lower than normal, necrosis can occur even more easily. The mucosa overlying the cartilage is initially destroyed. The bared cartilages become necrotic and ultimately slough. Attempts at repair after full-thickness damage to the tracheal wall lead only to scar formation. Because the erosion is circumferential, the resultant strictures are also. Even further erosive damage can lead to tracheoesophageal fistula posteriorly or to perforation of the innominate artery anteriorly.
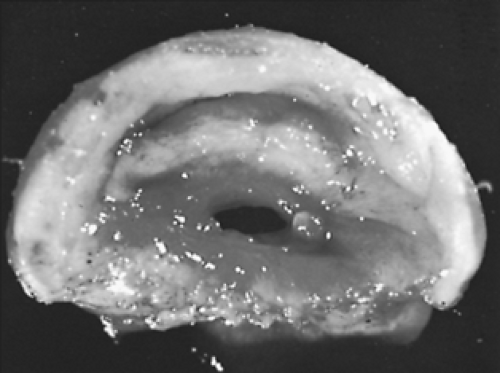 Figure 80-2. Circumferential stenosis at cuff level. This surgical specimen shows the narrow size to which the lumen may be reduced before recognition of symptoms. |
Patients with stenosis and malacia develop symptoms and signs of airway obstruction consisting of dyspnea on exertion, stridor, cough, and obstructive episodes. Hemoptysis does not occur. In a few patients, pneumonia, sometimes bilateral, has been noted. On occasion, a patient, while still intubated, begins to develop obstruction from formation of granulations around
the tip of the tube. In most instances, the obstruction appears only after extubation, because the tube splints a cuff stenosis or potential stomal stenosis as long as it remains in place. Any patient developing symptoms of airway obstruction who has been intubated for over 24 hours within the previous 2 years must be considered to have organic obstruction until proved otherwise. Many such patients have been treated for varying lengths of time with the incorrect diagnosis of asthma. Such errors resulted from lack of awareness of these lesions and the fact that in most patients routine radiography of the chest shows normal lung fields.
the tip of the tube. In most instances, the obstruction appears only after extubation, because the tube splints a cuff stenosis or potential stomal stenosis as long as it remains in place. Any patient developing symptoms of airway obstruction who has been intubated for over 24 hours within the previous 2 years must be considered to have organic obstruction until proved otherwise. Many such patients have been treated for varying lengths of time with the incorrect diagnosis of asthma. Such errors resulted from lack of awareness of these lesions and the fact that in most patients routine radiography of the chest shows normal lung fields.
Symptoms occurred in a few patients within 2 days of extubation; most demonstrated symptoms between 10 and 42 days after extubation, and a few at greater intervals, usually within a few months. If a patient remains sedentary while recovering from the original disease, the airway may shrink to a critical diameter of 4 to 5 mm before symptoms become obvious. At this aperture, fatal obstruction may occur at any time.
Although general improvement has occurred with design of large-volume cuffs, most of these cuffs can still produce tracheal injury if slightly overinflated beyond their resting maximal volume, because of their relatively inextensible materials. Stomal injuries continue to occur for the reasons described. Cricothyroidotomy may lead to severe or irreparable subglottic injury.
Three additional and particularly severe injuries to the airway may occur from intubation. These are tracheoesophageal fistula, tracheoinnominate artery fistula, and subglottic laryngeal or laryngotracheal stenosis. Tracheoesophageal fistula occurs most commonly in patients who have a ventilating cuff in the trachea for a long period of time along with a feeding tube in the esophagus. The two foreign bodies compress the common wall between trachea and esophagus, leading first to inflammation, which seals one against the other, and then perforation, which may enlarge to include the entire membranous wall of the trachea. Concomitant circumferential injury to the trachea is usually present as well, as pointed out by Grillo and colleagues,21 because this is basically a cuff lesion.
Anterior erosion of the trachea may lead to a fistula into the innominate artery. A small number of anterior erosions were seen in the past that were caused by angulation of a tube tip or a high-pressure cuff itself directly eroding through into the artery. More common, although still rare, are erosions of the artery that occur at the inferior margin of a low-placed tracheostomy stoma that is in immediate contiguity with the artery. The inner curve of the tube erodes its way through the arterial wall. It is seen most often in children and young adults in whom tracheostomy is placed too low, because on hyperextension more than one-half of the trachea rises up into the neck. If the stoma is placed with respect to the sternal notch rather than to the cricoid cartilage, the tracheostomy then resides just above the elevated innominate artery. Deslauriers and colleagues9 called attention to this complication.
Stenosis of the upper trachea may be associated with a severe subglottic stenosis as well. Stenosis of the subglottic larynx arises from three causes. The principal one is erosion, which is caused by an endotracheal tube that has been left in place for some time. The principal factor at fault may be use of a tube that has a bore too large for the patient. One of the narrowest parts of the upper airway is at the level of the cricoid cartilage. The second most common cause is erosion by a tracheostomy tube upward through the cricoid cartilage to affect the lower anterior larynx. It occurs most commonly in older patients who are kyphotic and in whom the cricoid cartilage is close to the sternal notch. A third cause of subglottic stenosis is the deliberate use of cricothyroidotomy for ventilation. If damage occurs at the stomal level, it is by surgical selection within the larynx. Lesions that involve the subglottic larynx as well as the upper trachea are much more difficult to repair surgically, although single-staged techniques have been devised by Grillo19 as well as by Pearson40 and Couraud7 and their associates.
Tracheoesophageal fistula becomes manifest by a sudden increase in tracheal secretions and the appearance of any ingested material in the trachea. If the patient is on a respirator, gastric distention may appear. Tracheoinnominate arterial fistulae are rare but may be announced by premonitory hemorrhage or by massive initial hemorrhage. In treating bleeding from a tracheostomy, it is important to differentiate between erosion of tracheal granulations or mucosa and arterial fistula. Sometimes angiography demonstrates a false aneurysm that soon bleeds massively. A review of the literature by Wright46 demonstrated 70 survivors of operations for tracheoinnominate artery fistulae but with only 40 surviving more than two months. About 25% of the patients with tracheoinnominate arterial fistulas who reach the operating room survive. Most of them died as a result of the underlying disease or other complications.
Extrinsic Lesions
Goiter
Large goiters, either cervical or mediastinal, may gradually compress the airway sufficiently to cause symptoms. The slow growth of the goiter may deform cartilaginous rings without destroying them. When the goiter is removed, the trachea may remain distorted in shape and narrowed, but clinically significant airway obstruction is rarely present. Quite frequently, removal of the goiter leads to immediate improvement in respiratory symptoms. If, however, sufficient softening of the cartilages has occurred that was caused by the prolonged compression, removing the supporting mass of thyroid tissue actually allows the trachea to collapse with respiratory effort. This is determined by intraoperative bronchoscopy, local examination and palpation in the operative field, and, finally, by observation of the patient in the operating room after extubation. Several methods of managing this problem have evolved, including intubation with an uncuffed tube followed by tracheostomy, preferably with insertion of a silicone T-tube several days later when the wound is sealed, immediate buttressing of the trachea with specially made polypropylene plastic rings, or in the past, by using traction sutures from the tracheal wall tied over either internal or external buttons.
An anterior substernal goiter usually does not exert pressure on the trachea because of its position in front of the great vessels. Katlic and colleagues29 reported that the trachea was more likely to be compressed by posterior descending goiters that enter the thoracic strait lateral to the esophagus and trachea.
Vascular Compression
Symptoms of tracheal compression may be produced by congenital vascular rings or by aneurysms of the innominate artery or
an anomalous subclavian artery that passes behind the trachea and esophagus. In children, compression may be produced by the innominate artery itself.
an anomalous subclavian artery that passes behind the trachea and esophagus. In children, compression may be produced by the innominate artery itself.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree