Fig. 15.1
The anatomical relationship defined by Goss [1] consisting of a bone and soft tissue “ring” at the end of a superior and inferior bony strut. The ring contains the distal clavicle, acromioclavicular ligaments, acromial process, glenoid process, coracoid process, and coracoclavicular ligaments. The superior strut is the clavicle proximal to the coracoclavicular ligaments, while the inferior strut is the scapula (Reproduced with permission. Source: Goss TP: Double disruptions of the superior shoulder suspensory complex. J Orthop Trauma. 1993;7(2):99–106)
Scapular and clavicle fractures are often associated with other injuries [2–5]. Commonly, they occur in conjunction with injuries to the chest wall, other portions of the SSSC, and ipsilateral fractures and dislocations. The increasing use of multidirectional CT in trauma patients has increased the detection and understanding of injuries to the shoulder girdle as well as other associated injuries. A recent review of the National Trauma Databank [6] compared patients with scapula fractures to a control group and found that the Injury Severity Score was nearly double in patients with scapula fractures (19.2 vs. 9.9). Interestingly, they found that the rate of associated rib fractures was 52.9 %, a similar rate to that found in a 1985 study [2] in which the proportion was 53.6 %.
Clavicle Fractures
Background
History
Clavicle fractures have been diagnosed and treated since antiquity. In 400 bc Hippocrates recommended a period of recumbence for those who had sustained a fracture of the clavicle: “It is of great importance, however, that the patient should lie in a recumbent posture. Fourteen days will be sufficient if he keep quiet, and twenty at most.” [7] However, modern treatment has advanced considerably since this recommendation.
Epidemiology
Clavicle fractures are the most common fracture in adults at 2–10 % [8–10]. In men, the incidence of clavicle fractures begins to decline after the age of 20; however, for women, the incidence is more constant with a tendency toward a bimodal distribution in adolescence and elderly age groups [8]. Mid-shaft fractures, representing over 75 % of the total, are most common and have a declining incidence with age [9].
Development
After birth, the clavicle continues to grow in length until the ossification centers fuse. The clavicle grows most rapidly in length prior to age 9 in girls and age 12 in boys [11, 12]. In the modern era, clavicles have been found to fuse at the age of 15 years on the average in women and 16 years of age in men.
Anatomy
Osteology
The clavicle is an S-shaped bone with unique anatomical features. The name is derived from the Latin name for a similarly shaped musical instrument. The apices of the bone are anteromedial and posterolateral with a transition occurring approximately two thirds of the way from the sternal attachment. There is not a discrete medullary cavity associated with the bone as there is a capacious medial shape, tubular mid-portion, and flatter lateral portion (Fig. 15.2a–c). The two joints at either end are both diarthrodial joints, which have little inherent bony stability. They derive most of their stability from strong ligamentous and capsular attachments. The sternoclavicular joint is responsible for the majority of motion associated with the clavicle, with at least 35° of elevation-depression, 35° of protraction-retraction, and 50° of rotation. This contrasts with the acromioclavicular joint, which is responsible for much less motion [13, 14].
Fig. 15.2
Clavicle morphology viewed from superior to inferior (a) and anterior to posterior (b) with cross-sectional slices through medial, middle, and lateral segments (c). This morphology must be taken into account during implant placement and instrumentation
Attaching Muscle Groups/Deforming Forces
The carotid artery, vagus nerve, and jugular vein pass deep to the medial clavicle en route to the head and neck. The brachial plexus travels inferoposterior to the clavicle en route to the upper extremity. Deforming forces to the clavicle after injury include the sternocleidomastoid muscle which attaches to the superior border of the medial clavicle and the pectoralis major which attaches to the inferior border. The trapezius attaches to the superior border of the distal clavicle, while the deltoid originates from the distal/inferior clavicle. The conoid and trapezoid ligaments attach to the distal third of the clavicle and anchor it to the coracoid [15, 16]. The mid-portion is free of these muscular attachments and represents a weaker area of the bone. The different deforming forces lead to characteristic displacement patterns after fracture [17, 18].
Operative Dangers
With the anterior approach to the clavicle, the first structures encountered that should be identified are branches of the supraclavicular nerves (Fig. 15.3). These course from superior to inferior over the platysma musculature. The brachial plexus and subclavian artery and vein run inferior to the clavicle and are very closely approximated in the middle third of the bone (Fig. 15.4a, b). Inferior to the distal clavicle, the subacromial artery is encountered as well. This is relevant in the cases of inferior exposure of the bone in ensuring that inferiorly directed drills and screws are safely applied [19]. Knowledge of these anatomical relationships is critical during drill trajectory and orientation of instrumentation and implants (Fig. 15.5a, b) [20].
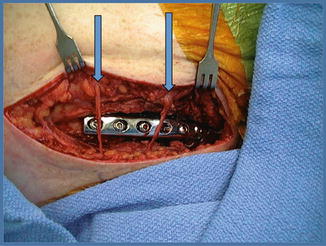
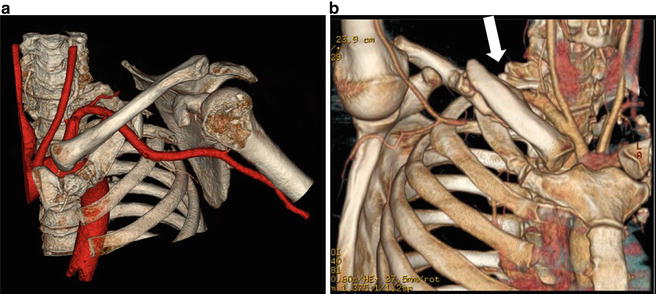
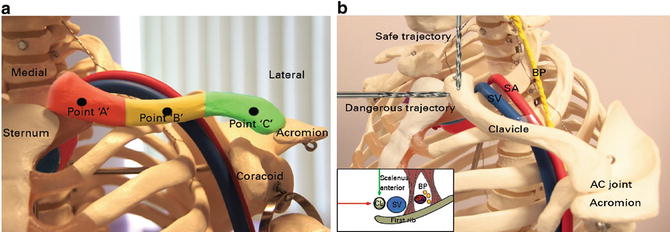
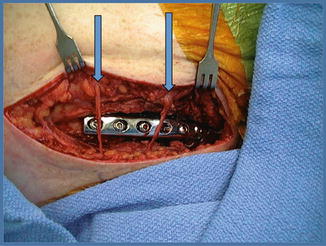
Fig. 15.3
An incision made for an open reduction and internal fixation of a clavicle fracture. The clavicle is post fixation, and crossing the wound, overlying the plate, are the two supraclavicular nerves (arrows), which have been protected. Sacrificing these nerves causes a patch of numbness inferior to the incision and is of little other consequence
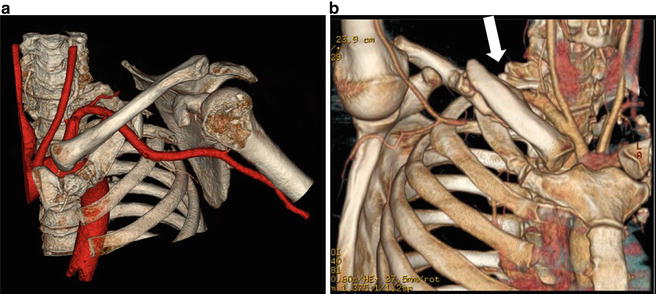
Fig. 15.4
Appreciate the intimate relationship of the subclavian artery in these arteriographic studies. (a) The artery is in red and the subclavian artery takeoff from the brachiocephalic trunk is easy to appreciate. (b) There is a middle one-third clavicle fracture, and the vulnerability during surgery to the subclavian vessels is easy to appreciate. The white arrow points to the crossover of the fractured clavicle and the subclavian artery
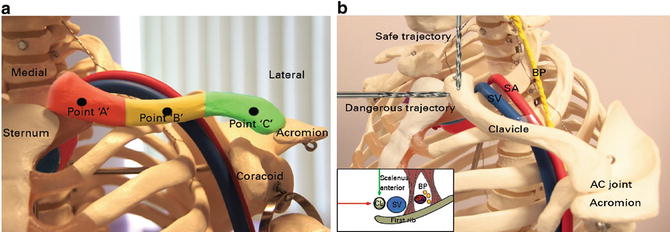
Fig. 15.5
This anatomical illustration details the relationship of the subclavian vessels to the clavicle. (a) An anterior to posterior orientation is shown in which a posteriorly directed drill puts the vessels at risk at the junction middle-distal 1/3rd and most medial 1/3rd of the clavicle. (b) A lateral to medial view illustrates both a safe and dangerous drill trajectory. Also shown with a green arrow (safe) and a red arrow (dangerous) in the inset illustration (Reproduced with permissions. Source: Sinha A, Edwin J, Sreeharsha B, Bhalaik V, Brownson P. A radiological study to define safe zones for drilling during plating of clavicle fractures. J Bone Joint Surg Br. 2011;93(9):1247–1252. doi:10.1302/0301-620X.93B9.25739)
Classification
The Allman classification is most frequently used for clavicle shaft fractures. It divides the clavicle into anatomical thirds with the middle third being group I, the distal third group II, and the proximal third group III. These are in order of the frequency of appearance, with group I fractures representing 81 % of injuries, group II representing 17 % of injuries, and group III representing 2 % of clavicle fractures [9]. The Neer classification for distal third (Allman group II) fractures is based on whether or not the coracoclavicular ligaments are intact (Fig. 15.6) [21]. If they are intact, the fracture is at less risk for nonunion, but if torn, wider displacement is allowed and hence a higher risk of nonunion results.
Fig. 15.6
Illustrated is Neer’s lateral third clavicle fracture classification. Note the importance of the relationship to the coracoclavicular ligaments that distinguishes different patterns (Reproduced with permissions. Source: Banerjee R, Waterman B, Padalecki J, Robertson W. Management of distal clavicle fractures. J Am Acad Orthop Surg. 2011;19(7):392–401)
Acromioclavicular Joint Dislocations
The acromioclavicular (AC) joint subluxates or dislocates when there is injury to one or more of the three important ligamentous structures which attach the lateral clavicle to the upper extremity. The coracoclavicular (CC) and coracoacromial ligaments as well as the AC joint capsule are responsible for the stability of the joint and when ruptured lead to characteristic injury patterns. Tossy and Allman developed classification schemes that describe the ligamentous injury and degree of displacement. Type I injuries represent partial tearing of the ligaments and are characterized by local AC joint tenderness: radiographs are normal. Type II injuries represent rupture of the capsule and AC ligament, but intact CC ligaments. There may be deformity and elevation of the clavicle, but this is limited to less than 1 cm. Type III injuries represent rupture of the AC capsule, and CC ligaments with pain, point tenderness, and plain films reveal complete dislocation. Rockwood later described three more severe injury patterns which are described according to the direction of displacement of the distal clavicle [22]. A type IV is complete disruption with the clavicle displaced posteriorly penetrating the trapezius. A type V is a more displaced version of a type III, where a type VI is when the clavicle is displaced and trapped caudal to the coracoid (Fig. 15.7) [22].
Fig. 15.7
Illustrated is the Allman acromioclavicular (AC Separation) classification which was expanded by Rockwood. Type IV and V separations are absolute indications for surgery, whereas type III surgery is controversial and probably suited only for young and active patients or to accomplish cosmetic goals (Reproduced with permissions. Source: Galatz LM, Williams Jr GR. Acromioclavicular Joint Injuries. In: Bucholz RW, Heckman JD, Court-Brown CM, eds. Rockwood & Green’s Fractures in Adults. 6th ed. Lippincott Williams & Wilkins; 2006:1331–1364)
Clinical Evaluation
Clavicle fractures can occur with low- or high-energy trauma. Associated injuries (such as to the chest wall or scapula) should be ruled out. Given the relationship between the clavicle and the subclavian vessels and brachial plexus, close attention should be paid to a detailed distal neurovascular examination. The skin should be examined for the presence of an open fracture, severe tenting, or abrasions.
Initial radiographic imaging should consist of plain films, including a chest radiograph, which should be examined for associated thoracic injuries, including hemo- or pneumothorax and rib fractures. Clavicular films should be obtained. If patient comfort and absence of other injuries necessitating supine positioning allows, dedicated upright clavicle films should be obtained. Usually, advanced imaging modalities to assess the clavicle itself are not necessary. A CT scan can be useful to assess for other injuries in patients with a high-energy mechanism or in cases where a pathologic fracture is suspected. The protocol we use at our institution includes a supine and upright 15° caudal tilt view and a bilateral clavicle view to include both AC joints (Fig. 15.8a–c). Radiographic protocols for clavicle fractures continue to evolve.
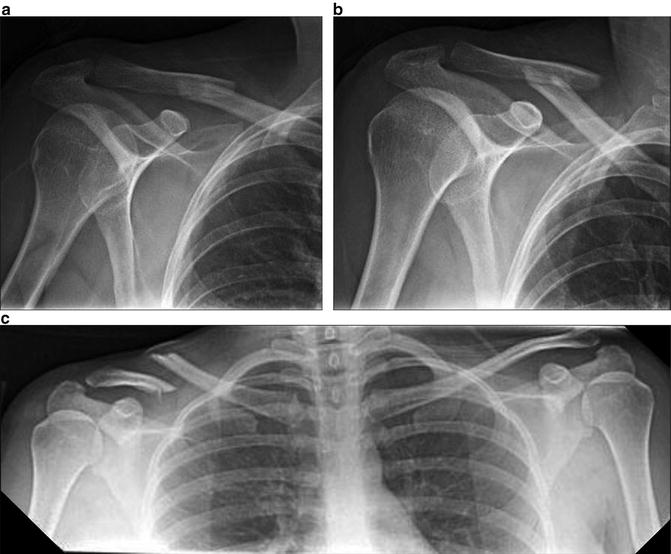
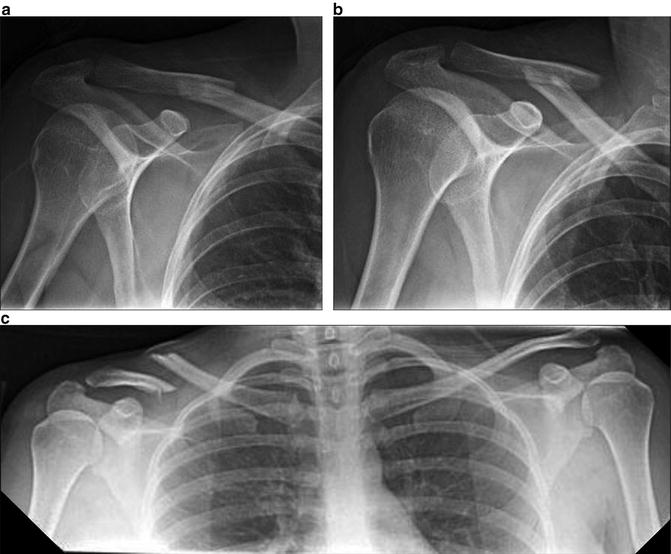
Fig. 15.8
Examples of plain radiographic imaging techniques with the patient in the supine position (a) and upright (b). (b) Shows increased displacement on upright films performed just after supine imaging (a). (c) Demonstrates medialization that is comparable and measurable on a bilateral upright clavicle film
Nonoperative Treatment
Nonoperative treatment has been the mainstay of treatment for the majority of clavicle fractures until recently. Improved clinical outcomes have not been demonstrated for any strategy over simple sling immobilization with early shoulder and elbow range of motion. Specifically, sling versus figure of eight brace immobilization have been proven to result in no difference in outcome [23].
There have been several recent randomized studies demonstrating lower symptomatic nonunion rates and better functional outcomes with reduction and operative fixation of displaced mid-shaft clavicle fractures in young (16–60 years of age), active patients, though this carries the risk of hardware irritation and the possibility of wound complications. Another relative indication for surgery is the displaced “floating shoulder” with dual injuries to the SSSC. It is important to be aware of the risk/benefit ratio for both operative and nonoperative treatment and discuss these issues with patients in a combined decision-making process.
Patients should be followed closely until the fracture consolidates with repeat upright clavicle films at weekly intervals for 3 weeks to ensure displacement remains within acceptable parameters because progressive displacement has been shown (Fig. 15.9a–c) [24]. During this period, elbow and shoulder range of motion should be encouraged.
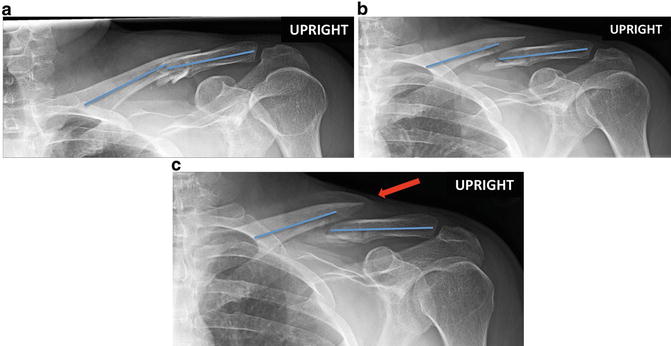
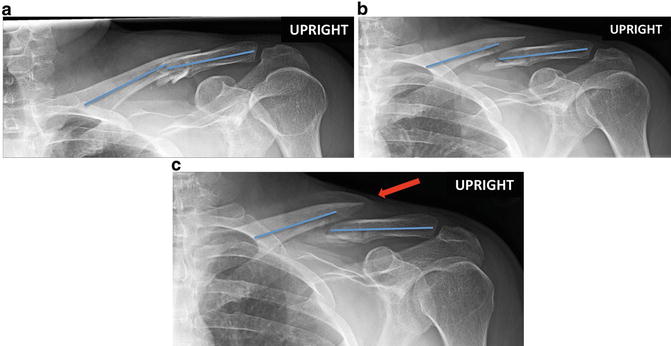
Fig. 15.9
(a) is an X-ray of an injury showing a middle 1/3rd clavicle fracture with minimal angular deformity or medialization. (b) and (c) demonstrate incremental displacement at 7 and 14 days after injury, respectively. This sequence shows the importance of serial radiographs at weekly intervals to assess displacement and determine surgical indications
Operative Treatment
Indications
For completely displaced mid-shaft clavicle fractures, several recent randomized studies have shown lower rates of nonunion, symptomatic nonunion, and higher functional outcome scores with open reduction and internal fixation [25, 26]. The rate of nonunion after the nonoperative treatment of mid-shaft clavicle fractures has been reported to range from 5 to 25 %. A 2013 retrospective review of 941 patients with nonoperatively treated displaced mid-shaft clavicle fractures by Murray and Robinson found a nonunion rate of 13.3 %. In multivariate analysis, smoking, comminution, and fracture displacement were most predictive of nonunion [27].
Functional outcomes have been shown to be better at most time points overall for patients treated with primary operative fixation [25]; however, these differences diminish when symptomatic nonunions are excluded [26]. Symptomatic malunion rates are also higher in nonoperatively treated patients [28]. An example of clavicular malunion with clinical deformity following nonoperative treatment is shown in Fig. 15.10. However, some have argued that good outcomes can be achieved in this setting by late reconstructive surgery and that the higher attendant costs and risks of primary operative fixation are not justified [29]. An understanding of the indications for operative treatment will continue to improve as further randomized studies delineate prognostic factors for poor outcome following closed treatment [30].


Fig. 15.10
Cosmetic deformity associated with clavicle malunion. One can appreciate a common complaint, in which straps slip down the shoulder
Medial third clavicle fractures are relatively rare accounting for <5 % of injuries to the clavicle; however, the degree of displacement is also linked to the risk for nonunion. Lateral third clavicle fractures with ruptured coracoclavicular ligaments are also associated with higher nonunion rates [28]. The precise degree of displacement associated with an unacceptably high risk of symptomatic nonunion and diminished function remains to be determined: patient selection is highly relevant in the proper decision for surgery.
Surgical Technique
The surgeon should preoperatively analyze the fracture pattern and displacement with the plan to restore length, alignment, and rotation. The patient is positioned in the beach chair position with all bony prominences well padded. The ipsilateral limb should be prepped to aid in fracture reduction and allow for easier restoration of length, alignment, and rotation. The patient’s anatomy is marked for a proper incision which should be just caudal to the bony prominence so hardware is not directly beneath the incision.
Plate Fixation
The length of plate fixation depends on the quality of the bone, the degree of comminution, the type of plate, the age of the patient, and their anticipated compliance. Plate placement can be in the superior or anterior position. Anterior plate placement was shown in one biomechanical cadaveric study to provide greater stiffness [31], and it has been associated with less prominence of the plate and diminished risk of injury to nerve or vessels and failure of fixation [32, 33]. However, superior plating remains more common in clinical practice [33], is familiar for most surgeons, and may yield a biomechanical advantage in middle third clavicle fractures over anterior plating.
The incision is taken down through subcutaneous tissue to expose the fascia surrounding the platysma musculature. The platysma is then cut directly to the periosteum, and cautery is useful for this vascular plane. A thick cuff is preserved to facilitate later repair. Any identified cutaneous branches of the supraclavicular nerve, usually present more medially within the platysma muscle, are preserved to prevent peri-incisional numbness. The patient should be warned of this potential for numbness preoperatively so expectations are managed. Minimal, but sufficient, periosteal dissection to allow for fracture exposure, reduction, and plate placement is performed. Careful retraction should respect posterior and inferior vital structures. Bone reduction forceps can be placed on either end of the fracture and used to manipulate the bone fragments back into position. Free draping of the arm allows elevation and rotation to achieve the appropriate alignment is useful and minimizes soft tissue trauma in obtaining reduction. Once aligned, bone reduction forceps placed in pilot holes on each side of the fracture can be used when stable bone ends allow for compression. K-wires can be used to provisionally hold large butterfly fragments. Greater comminution should be bridged, and devascularization and exposure of the comminution zone should be avoided. In such cases, the fracture is fixed distally first, and the plate used as a reduction aid to restore length and rotation. With the fracture reduced, lag screw fixation is employed when possible. Small, comminuted fragments that cannot be captured with lag screw fixation can be fixed in location with suture, and such fractures should be spanned with a plate in the bridging mode (Fig. 15.11a, b). A plate of the appropriate size is selected and contoured to the patient’s anatomy. The goal should be a minimum of three bicortical screws on each side of the fracture. Straight dynamic compression plates are often prominent, while pelvic recon plates may not be strong enough for the forces acting on the fracture: for these reasons, the implant of choice is a pre-contoured compression plate designed specifically for clavicular fixation.
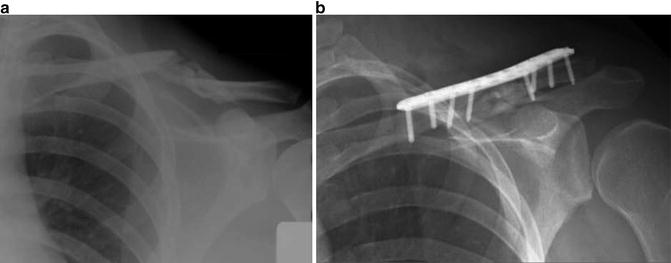
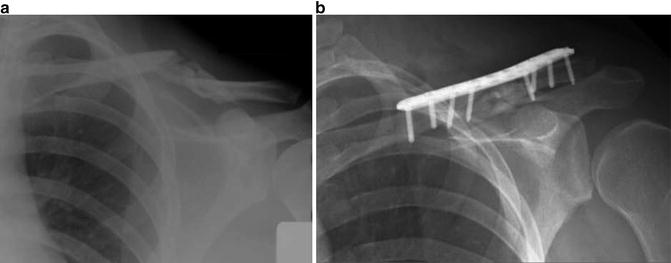
Fig. 15.11
(a–b) Bridge plating technique for a shortened comminuted clavicle fracture. Using this technique, the surgeon must preserve blood supply and employ a low strain zone over a longer working length of the plate; otherwise, the plates will be too stiff for the anatomy prescribed for this technique
A single flat-plate radiograph or C-arm image should be obtained prior to closure to ensure that no screw tips are prominent as brachial plexus irritation or trauma to the subclavian artery or vein has been reported. It can be helpful to place a flat plate behind the patient’s shoulder prior to prepping and draping, so that the cassette is in position for good imaging without disruption of the sterile field after fixation. Closure of the platysma and fascia as one layer is performed using 2-0 braided sutures. The subcutaneous tissues are re-approximated with inverted sutures, and the skin is best approximated with subcuticular absorbable monofilament suture that provides a cosmetic closure.
Intramedullary Nail Fixation
For simple, non-comminuted fracture patterns, intramedullary fixation is an attractive option as it requires less operative dissection [34]. Historically, Rockwood [35, 36], Hagie [37–40], and Knowles [41] pins were used for intramedullary fixation of clavicle fractures, but particularly in comminuted or rotationally unstable fracture patterns, they have been associated with high rates of implant failure and infection due to hardware prominence at the insertion site [36, 37]. Intramedullary nailing is demonstrated in Fig. 15.12a, b. Another technique is the use of titanium elastic nails [41]. The technique described for this includes the use of a medial opening point on the clavicle using an awl or a drill, followed by closed or mini-open reduction of the fracture and advancement of the nail past the fracture site. Nails are removed after fracture union. These have good results in several small case series and retrospective studies [41–43]. Other nailing systems have recently been developed and allow for locking and length-stable fixation which is an attractive option: it remains to be seen what their exact role will be in this area.
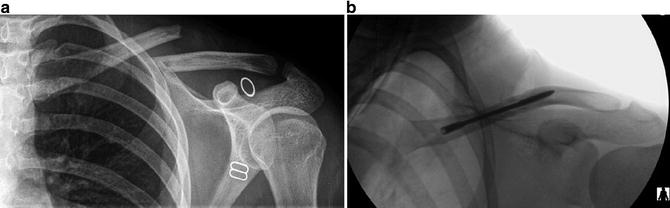
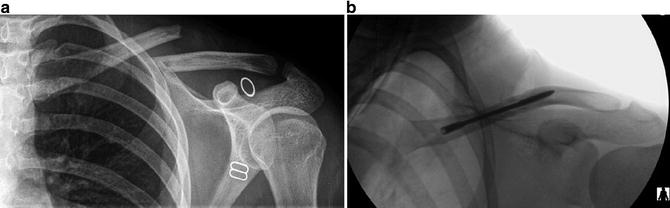
Fig. 15.12
Pre- (a) and postoperative (b) images of a clavicle fracture fixed with a nail. This transverse mid-shaft clavicle fracture is perfectly suited, because it can be reduced closed or with a mini-open technique minimizing the scar. Comminuted clavicle fractures may be rotationally and axially unstable after nailing and lead to malunion
Distal Third Clavicle Fractures
Distal clavicle fractures and acromioclavicular separations represent a surgical challenge to treat due to the frequent lack of bone to support fixation at the end of the clavicle. Furthermore, the deforming forces are strong and differ depending on whether the injury is a pure dislocation of the AC joint or a distal clavicle fracture with disrupted CC ligaments. The deforming forces cause superior migration of the proximal segment, while the distal segment often caudally displaces because of the force of gravity and muscular contractions across the shoulder. Pre-contoured locking plates which allow for fixation in osteoporotic bone can be useful as well [41]. These implants take advantage of multiple distal clavicular screws at different vectors to maximize purchase in the short distal segment. These plates can also be augmented with a repair of the coracoclavicular ligaments, a treatment combination which may enhance stability [44]. Alternatively, simple reconstruction of the coracoclavicular ligaments in isolation with tape or an endobutton technique has also been used successfully in isolation [45, 46] but may be more vulnerable to failure (Fig. 15.13a, b).
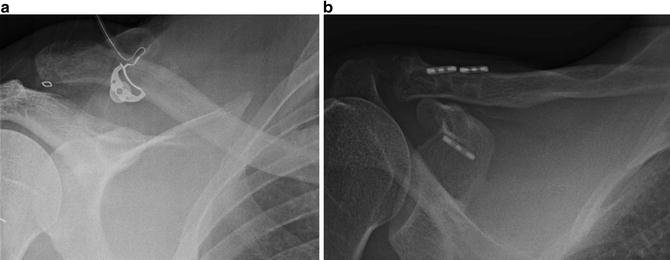
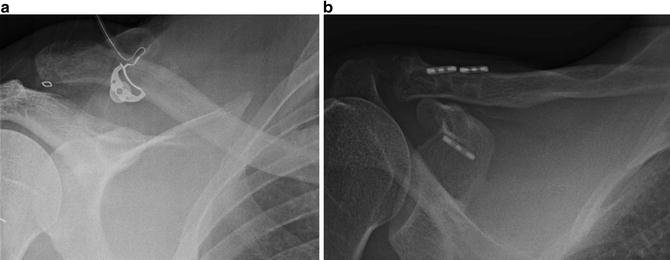
Fig. 15.13
A pre- (a) and postoperative (b) image of an acromioclavicular dislocation which was fixed with a tightrope technique in which two heavy fiber wire suture are passed through the clavicle and coracoid, both tethered to their respective bones and tied over small metal stays to help prevent cutout
For far lateral clavicle fractures, it is often difficult to obtain sufficient purchase in the distal fragment with plate fixation: in such cases, a specially contoured hook plate (Synthes Depuy, USA, Paoli, PA) has been used [47] which is slid beneath the acromion posterior to the AC joint. This implant allows for screw fixation into the clavicle, while the distal hook levers under the neck of the acromion (Fig. 15.14a–c). These typically need to be removed after fracture union because the implant does cross a mobile joint, and osteolysis and fracture of the acromion has been reported [48]. The hook plate is also a viable treatment option for isolated AC joint dislocations.
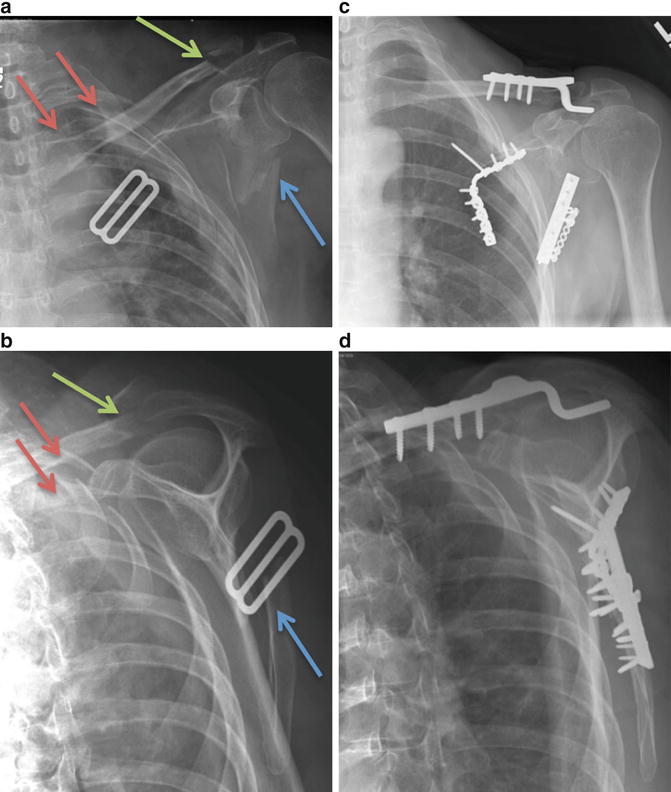
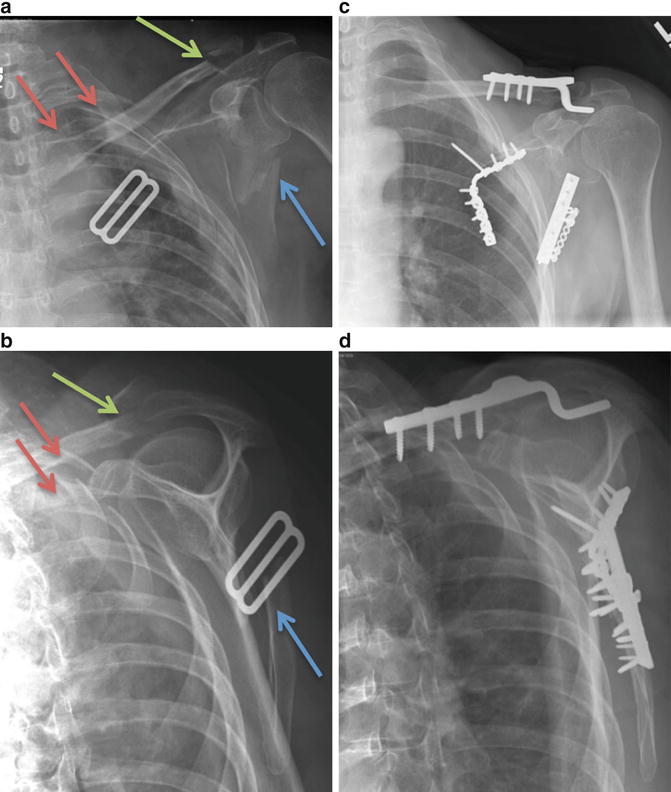
Fig. 15.14
Illustrative example of a hook plate (Synthes USA, Paoli, PA) fixation of a lateral third clavicle fracture (green arrow) with ipsilateral scapula (blue arrow) and no. 2 and no. 3 rib fractures (red arrows) as seen preoperative anterioposterior (a) and scapula Y (b) radiographs. Following consolidation of all fractures as seen on the anterioposterior (c) and scapula Y (d) follow-up radiographs, the patient underwent hook plate removal
Sternoclavicular Dislocations [49–53]
Sternoclavicular dislocations occur as a result of direct trauma or indirect forces through the shoulder. In skeletally immature patients up to approximately 20 years, medial physeal fractures can be mistaken for dislocations. Dislocations are either anterior or posterior. Concomitant injury to mediastinal structures in posterior dislocations must be ruled out. These may include injuries to the trachea or larynx, and esophagus. The brachiocephalic trunk and neurologic injury to the phrenic nerve should be ruled out with a thorough history and physical examination. A CT angiogram or arteriography is indicated in posterior dislocations to assess the great vessels for injury that may include intimal damage, pseudo-aneurysm, or simple compression. These findings will help guide treatment.
When attempting manipulation of the posterior dislocation, it is important to have communicated directly with a cardiac surgeon so that they can be on standby in the event of a major arterial hemorrhage. This is imperative if a preoperative arteriographic radiography has not been done or has shown any abnormality. Postreduction clinical examination and observation are mandatory. In the acute setting, closed reduction and stabilization is recommended for both anterior and posterior dislocations to restore anatomy, reduce deformity, and improve long-term function. The decision to proceed with open reduction if closed reduction is unsuccessful depends on the health and activity level of the patient. Physeal disruptions are also amenable to operative fixation. In such cases, a plate is used to capture the medial fragment, ideally with locked fixation to avoid loosening and pullout (Fig. 15.15a–e). Suture fixation alone with heavy-braided suture is possible. These patients must be immobilized for approximately 2 weeks because they can experience cutout due to deforming forces.
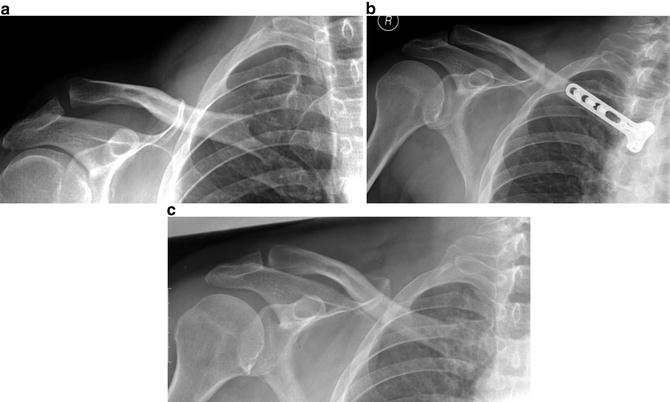
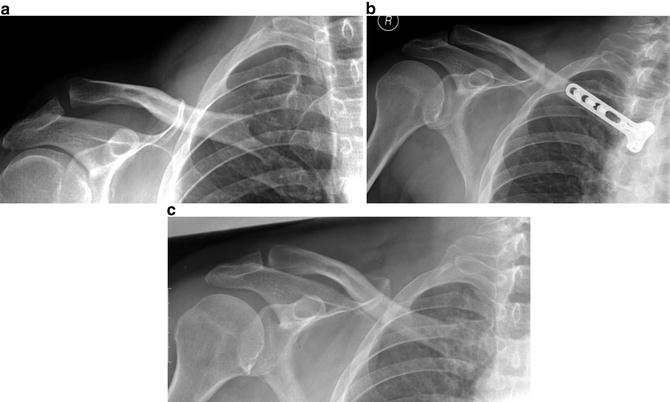
Fig. 15.15
Example of locking plate fixation of a medial third clavicle fracture dislocation injury (a), postfixation (b), and healed following hardware removal (c) anterioposterior X-rays
For closed reduction of anterior dislocations, the patient is placed supine with a pad between the shoulders, and direct pressure is applied on the medial clavicle in a posterior direction. These can be quite stable after reduction: if not, an open reduction may be indicated in a high-demand patient. The technique for posterior dislocation involves the placement of a pad between the scapulae; traction is applied to an extended/abducted arm with counter traction or posterior pressure applied to the shoulder. A sterile towel clip can also be used percutaneously to grasp the medial clavicle and reduce it (Fig. 15.16a). Posterior dislocations are frequently stable once reduced, but if closed reduction fails, open reduction and stabilization is performed with heavy-braided suture repair of the capsule and periosteum (Fig. 15.16b, c). Ligamentous reconstruction has been described, but typically for chronic dislocation variants and they are fraught with high failure rates. The authors’ preferred management strategy for painful chronic dislocations is medial clavicle resection with imbrication of the scar tissue and capsule. Generally patients are very satisfied with resolution of both deformity and pain. The use of smooth pins for stabilization of dislocations is to be avoided due to the potentially catastrophic complication of pin loosening and migration.
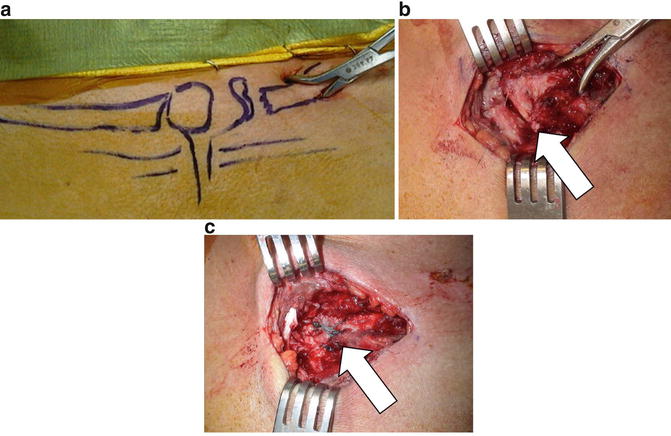
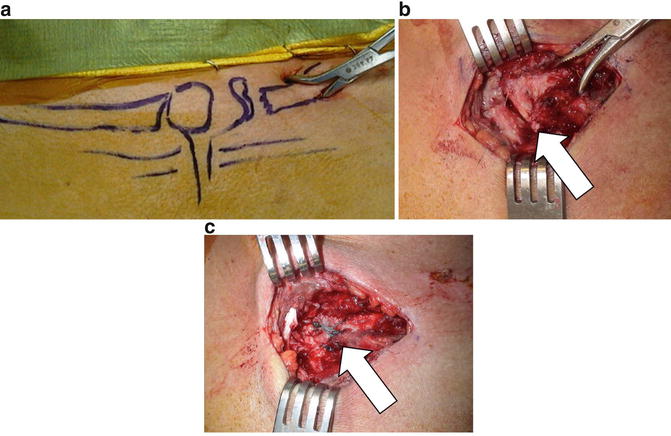
Fig. 15.16
An 18-year-old patient with proximal clavicle physeal dislocation. Closed reduction was possible with percutaneous application of a towel clip, as shown (a). Due to instability, the dislocation was exposed (b) and heavy-braided suture used in repair (c). The dislocation (b) and suture repair (c) are indicated by the white arrows
Scapula Fractures
Background
History
In the first description of a scapula fracture in 1579, Dr. Ambroise Pare wrote, “When the fracture involves the neck of the scapula the prognosis is almost always fatal, as was also the case of some famous people, for instance the King of Navarre.” It is unclear whether it was the fracture itself that he thought the mortality was attributable to or to the likely associated injuries. Other French surgeons such as Jean-Louis Petit, Joseph Guichard Duverney, and Pierre-Joseph Desault furthered the classification and treatment considerations of scapula fractures. Albin Lambotte is credited with the first internal fixation of a scapula fracture in 1911 [54].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


