Hypercholesterolemia, hypertension, diabetes, and smoking are the major modifiable risk factors for atherosclerotic cardiovascular disease (ASCVD), the leading cause of morbidity and mortality in the United States (US). With the exception of hypercholesterolemia, drug therapy is recommended when specific targets (e.g., blood pressure ≤140/90 mm Hg, Hemoglobin A1C ≤7%, and smoking cessation) are not achieved with lifestyle modifications. In contrast, the 2013 American College of Cardiology/American Heart Association cholesterol treatment guidelines provide a class I recommendation for drug treatment only in the presence of established ASCVD, profound hypercholesterolemia, diabetes, or an estimated 10-year risk ≥7.5%. Although based on evidence from randomized controlled trials, we believe that these recommendations result in undertreatment of many subjects who would benefit from earlier intervention to halt the ASCVD process. To illustrate this point, we estimated the nationwide impact on ASCVD events if risk-based criteria, similar to those in the current cholesterol treatment guidelines, were extended to the treatment of hypertension.
Using data from the National Health and Nutrition Examination Surveys (NHANES) from 2007 to 2012, we compared 2 scenarios: first, implementation of current hypertension guidelines; and second, implementation of hypothetical hypertension guidelines that approximate the risk-based criteria of the current cholesterol guidelines. We included NHANES participants aged ≥20 years in whom all covariates required for the American College of Cardiology/American Heart Association pooled cohort risk equations were available. We first identified those participants (group A) who were either receiving or recommended to receive drug therapy for hypertension according to American Society of Hypertension guidelines. We then applied the following hypothetical risk-based criteria for drug therapy to this group: (1) clinical ASCVD; (2) systolic blood pressure ≥160 mm Hg (selected to represent profound hypertension); (3) diabetes in those aged 40 to 75 years; or (4) estimated 10-year ASCVD risk ≥7.5% (group B).
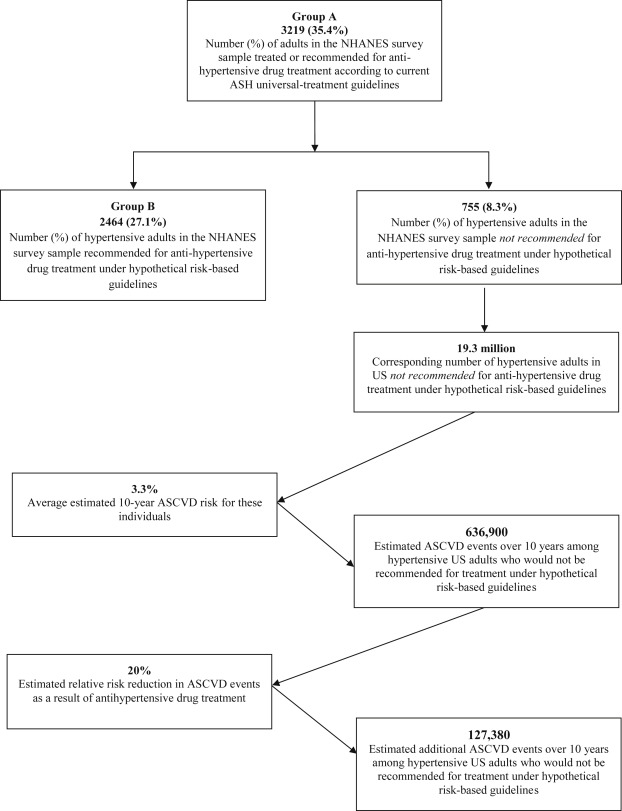
Complete data were available for 9,088 adult NHANES participants. Group A consisted of 3,219 participants (35.4%), and group B consisted of 2,464 participants (27.1%). The difference between these 2 groups (755 participants, or 8.3%) represents those NHANES participants who would no longer be recommended for drug treatment of hypertension under risk-based guidelines (the “undertreated” group). The average 10-year ASCVD risk in this group was calculated to be 3.3%. Using appropriate weighting to extrapolate these findings to the general US population, the proportion of undertreated subjects corresponds to approximately 19.3 million adults. Under the conservative assumption that drug therapy for hypertension results in a 20% relative decrease in ASCVD events, application of risk-based guidelines rather than universal treatment guidelines would result in the occurrence of approximately 127,380 additional hard ASCVD events nationwide over a 10-year period ( Figure 1 ).