Lung Tumors in the Immunocompromised Host
Philip G. Robinson
Joseph LoCicero III
Several situations may lead to the development of an immunocompromised state that could last for life or for an extended period of time. Iatrogenic immunosuppression (solid-organ transplantation or autoimmune diseases), chronic infections (human immunodeficiency virus), new malignancies, or anticancer therapy may cause altered immunocompetence (Table 127-1). Patients with these altered states have a greater incidence of certain malignancies that do not often occur in the general population and, according to Buell and colleagues,12,13 these include Kaposi’s sarcoma and posttransplantation lymphoproliferative disorder as well as cancers in other organs (Table 127-2). In some cases, immunocompromised patients may develop pulmonary neoplasms that are not necessarily related to their immune status but may be due to other influences. Autoimmune diseases do not cause immunosuppression, but many of these patients are treated with immunosuppressive agents to control the inflammatory response. Each specific situation has been analyzed individually by various investigators. Some of the mechanisms whereby malignancy develops now appear to be similar. To show the significance of lung tumors in the immunocompromised host, we review the broader spectrum of tumor biology in these patients.
Posttransplant Malignancies
Patients on immunosuppressive drugs after organ transplantation have a higher incidence of certain malignancies. This observation was made within a few years of the routine use of cadaver renal transplantation for kidney failure. Penn83 pointed out in 1994 that a variety of neoplasms may develop a short time after transplantation. Kaposi’s sarcoma appeared at an average of 21 months, and non-Hodgkin’s lymphomas appeared at an average of 32 months after transplantation. According to Buell and colleagues,12 malignancies may play a greater role in transplant patients for two reasons. First, graft and patient survival have lengthened the observation period of immunosuppressed recipients. Second, the mean age of recipients has increased by 10 years. The change in both of these variables may increase the number of malignancies occurring in transplant recipients. The most common malignancies in transplanted patients are lymphomas or posttransplant lymphoproliferative diseases (PTLDs).
In 2007, the International Society of Heart and Lung Transplantation49 listed cumulative 15-year data from the International Transplant Registry. A total of 12,089 lung transplant recipients are in the registry. Of those followed for at least 1 year, the incidence of new malignancies is 3.7%; at 5 years, 12.4%; and at 10 years, 25.0%. The most common neoplasm in the early follow-up is lymphoproliferative disorders, at 46%, but this rapidly decreases to around 20% by 10 years. Skin cancers are the overall most common at 38%, starting off at 23.7% after the first year and rising to a stunning 58.4% by the 10th year of follow-up. The two factors most significant for developing a malignancy are increasing age and history of a prior malignancy.
In a single-institution series, Mihalov and associates70 reported in 1996 on 674 recipients, including 305 renal, 307 heart, 54 lung, and 8 heart–lung transplants. They noted a 3.7% incidence of cancer in lung transplants and also that thoracic organ transplant recipients, in contrast to renal transplant recipients, had a significantly higher rate of lymphomas. Spiekerkoetter and colleagues96 reported in 1998 that of 219 patients who underwent lung transplantation, 1 patient developed pulmonary squamous cell carcinoma. However, the chance for developing lung cancer after solid-organ transplantation, as reported in 2003 by De Perrot and associates,22 is very low (0.3%) and usually occurs in continuing smokers.
Not all new pulmonary nodules are posttransplant malignancies. End and associates33 looked at pulmonary nodules in 64 lung transplant recipients in 1995 and found that nodules developed in eight patients (12.5%) an average of 5.8 months after transplantation. In two patients, the nodules spontaneously resolved over 3 weeks. Of the remaining six patients, three had posttransplant PTLD, two had aspergillosis, and one had a mixed bacterial abscess.
Proposed Causal Mechanisms of Posttransplant Malignancies
Concepts about the development of posttransplant tumors have varied over the years. Patients with congenital defects in antibody production or cellular immunity have experienced a higher
incidence of non-Hodgkin’s lymphoma, leukemia, and other malignancies. Buell and colleagues12 summarized the various potential causes: (a) a disruption in antitumor immune surveillance and antiviral activity resulting in a loss of detection and elimination of neoplastic cells; (b) chronic antigenic stimulation from transplanted organs, infections or transfusions that may result in PTLD; (c) infections (Table 127-3); (d) immunosuppressive agents that may potentiate the carcinogenic effects of other agents; or (e) immunosuppressive agents, such as azathioprine and cyclosporine, that may promote carcinogenesis.
incidence of non-Hodgkin’s lymphoma, leukemia, and other malignancies. Buell and colleagues12 summarized the various potential causes: (a) a disruption in antitumor immune surveillance and antiviral activity resulting in a loss of detection and elimination of neoplastic cells; (b) chronic antigenic stimulation from transplanted organs, infections or transfusions that may result in PTLD; (c) infections (Table 127-3); (d) immunosuppressive agents that may potentiate the carcinogenic effects of other agents; or (e) immunosuppressive agents, such as azathioprine and cyclosporine, that may promote carcinogenesis.
Table 127-1 Frequent Malignancies in Immunocompromised Hosts | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
Penn82 in 1986 noted that among 65 female transplant patients with cancers of the vulva, vagina, uterine cervix, or anus, several had a history of condyloma acuminatum (human papillomavirus) or herpes genitalis (herpesvirus). He suggested that these viruses might be contributing to cancer development. Subsequently, other viruses, such as Epstein–Barr virus (EBV), human herpesvirus-8 (HHV-8), and hepatitis B and C viruses were implicated in lymphomagenesis and carcinogenesis (Table 127-3).
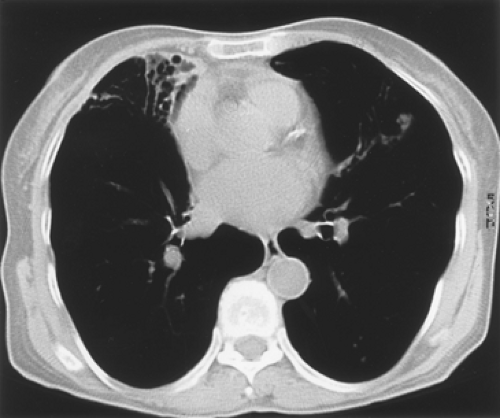
Berger and Delecluse7 postulated in 1993 that PTLD is the result of the interaction between the virus and the host cells. After infection, there is a primary response, which is initially mediated by natural killer cells and CD4 suppressor T cells. Later, the secondary immune response is mediated by human leukocyte antigen (HLA)–restricted CD8 cytotoxic T cells, which are specific for EBV. Also, there is an immunoglobulin M (IgM) and later an IgG response to the viral capsid antigen, early antigen, and EBV nuclear antigens. EBV by-products, such as nuclear antigens and latent membrane proteins, upregulate gene series. This leads to proliferation and transformation of EBV-infected cells. This enlarged pool of proliferating cells carries an additional risk for mutation of an oncogene or a tumor suppressor gene. In an immunosuppressed patient, the EBV-infected cells are not controlled; this leads to the spectrum of PTLD, which ranges from hyperplasia to lymphoma (Fig. 127-1).
Table 127-2 Incidence of de Novo Neoplasms in Renal Transplant Recipients | ||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||
Table 127-3 Infectious Agents Implicated in the Development of Cancers in Transplant as Well as Immunocompetent Patients | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Gottschalk and colleagues41 claimed in 2005 that 90% of PTLDs contain EBV. Taylor and associates101 have pointed out that 85% of PTLDs in the United States and Europe are of B-cell lineage and most (80%) are associated with an EBV infection. Further, around 10% to 15% of PTLDs are of T-cell lineage, and around 30% of these cases are associated with EBV. Consequently a great deal of effort has been expended to understand the mechanism by which EBV produces PTLD. EBV is a gamma herpes virus, which has a worldwide distribution and establishes a latent infection in more than 90% of individuals. Taylor and colleagues101 believe that it infects over 95% of the world’s population in childhood or early adolescence. EBV-infected B cells differentiate into memory cells (which downregulate the EBV and allow a latent infection) or are killed by cytotoxic T-cell lymphocytes. In immunosuppressed patients with decreased cytotoxic T cells, the proliferation of EBV infected B cells may
exceed their clearance by cytotoxic T cells or their differentiation into memory B cells. Further, B cells that are not normally infected with EBV may become infected and lose their ability to escape the EBV growing phase, or they may not be destroyed by cytotoxic T cells. In addition to these changes, other stimuli are thought to be required for the development of PTLD. These may consist of the local cytokine environment and chronic antigenic stimulation. Zhang and colleagues115 noted in 2001 that patients experiencing chronic rejection exhibited high levels of both interferon-gamma (IFN-γ) and interleukin-10 (IL-10), suggesting the importance of these cytokines in the modulation of PTLD. Biopsies of PTLD show that CD4 suppressor T cells infiltrate into the proliferation. Also, there are elevated levels of IL-4, IL-6, and IL-10. A genetic decrease production of interferon alpha (IFN-α) is more common in patients with PTLD.
exceed their clearance by cytotoxic T cells or their differentiation into memory B cells. Further, B cells that are not normally infected with EBV may become infected and lose their ability to escape the EBV growing phase, or they may not be destroyed by cytotoxic T cells. In addition to these changes, other stimuli are thought to be required for the development of PTLD. These may consist of the local cytokine environment and chronic antigenic stimulation. Zhang and colleagues115 noted in 2001 that patients experiencing chronic rejection exhibited high levels of both interferon-gamma (IFN-γ) and interleukin-10 (IL-10), suggesting the importance of these cytokines in the modulation of PTLD. Biopsies of PTLD show that CD4 suppressor T cells infiltrate into the proliferation. Also, there are elevated levels of IL-4, IL-6, and IL-10. A genetic decrease production of interferon alpha (IFN-α) is more common in patients with PTLD.
Taylor and associates101 describe the EBV proteins EBV nuclear antigen (EBNA-1) and latent membrane protein (LMP1) as particularly important in oncogenesis. EBNA-1 allows the replication of viral DNA and its distribution to daughter cells. LMP1 inhibits apoptosis by upregulating the antiapoptotic genes BCL2 and A20. These changes may result in a polyclonal EBV-driven proliferation of lymphocytes with continued immunosuppression. Some cells may acquire additional changes, such as BCL6 mutation, C-myc rearrangements, or disruption of p53 tumor suppressor genes. The etiology of non–EBV-related PTLD is unclear.
Boyle and colleagues10 in 1997 studied 120 children receiving thoracic organ transplants and found a 19.5% incidence of PTLD in heart–lung and lung recipients and only a 7.7% incidence in heart recipients. They also discovered that recipients who were EBV-positive before transplantation did not develop PTLD. Only those who developed a primary EBV infection developed PTLD. Because of this, Verschuuren and associates109 suggested in 2001 that an EBV polymerase chain reaction (PCR) test be administered to patients before and after lung transplantation. Wong and coworkers113 urged in 2001 that recipients and donors should be matched in a similar manner as they are matched for HLA and cytomegalovirus status.
Autoimmune Diseases
Autoimmune diseases do not produce a compromised immune system until patients are treated. Patients with these diseases usually receive steroids and anticancer agents, such as azathioprine or cyclophosphamide. Mellemkjaer69 and Ramsey-Goldman87 and their associates reported in 1997 and 1998, respectively, an increased incidence of the usual types of lung carcinomas in patients with systemic lupus erythematosus (SLE). Bin and colleagues9 in 2007 reviewed the association between lung carcinoma and SLE. They found an increased incidence of non-small-cell carcinomas with the same distribution as those in patients who did not have SLE. They could not identify a specific demographic factor responsible for the increased rate of carcinoma, although they considered smoking, genetic links, fibrotic lung disease, and oncogenic viruses.
Mellemkjaer and colleagues68 in 1996 also described a similar increase of lung carcinomas in patients with rheumatoid arthritis (RA). Chen and colleagues19 found in 2005 that lung carcinomas associated with RA did not shorten life expectancies. Further, they found no significant difference in age and histologic type between patients with and those without RA. Bernatsky and associates6 examined in 2008 a cohort of patients with RA looking to see if exposure to antirheumatic drugs increased the risk of lung carcinoma and found that they did not. Douglas and coworkers27 described in 2005 a patient with a long-standing history of RA who developed a mucosal-associated tissue (MALT) B-cell lymphoma of the lung with focal cells showing expression of Epstein–Barr virus latent membrane protein-1. Mackie and Pohlen64 in 2006 described a 70-year-old woman with RA who developed a large pulmonary B-cell lymphoma while taking methotrexate. After stopping the methotrexate and with no further treatment, the left-lower-lobe mass decreased in size and showed less activity on PET imaging. Ebeo and colleagues30 in 2008 described a similar case of a 54-year-old man with a 12-year history of RA who had received methotrexate for 5 years and developed a diffuse large B-cell lymphoma in the left upper lobe of the lung. The patient had positive serology for EBV, but in situ hybridization for EBV in the tumor cells was negative. Following resection, the patient declined further treatment. At 2 years’ follow-up, the patient was free of disease.
Quismorio86 reviewed in 1996 the subject of pulmonary complications in Sjögren’s syndrome. He found an increased risk for developing pulmonary lymphomas. In a study from the Mayo Clinic in 1989, Hansen and coworkers44 described 10 of 50 patients with Sjögren’s syndrome who had pulmonary lymphomas. These ranged from low to high grade, with the high-grade ones being associated with increased mortality. Nakamura and colleagues74 in 2002 described a 53-year-old woman with untreated Sjögren’s syndrome who developed a MALT lymphoma of the lung.
Nicholson and coworkers78 in 1996 described six cases of primary pulmonary B-cell lymphomas in patients with autoimmune diseases who were receiving immunosuppressive drugs. The patients had rheumatoid arthritis, polymyositis, cryptogenic fibrosing alveolitis, mixed connective tissue disease, and Sjögren’s syndrome. Only the patient with Sjögren’s syndrome who was not receiving immunosuppressive therapy developed a low-grade lymphoma. The other five patients were receiving immunosuppressive therapy, and they all developed high-grade lymphomas.
Table 127-4 Incidence of Non-AIDS—Defining Neoplasm in the Pre-HAART and HAART Era | ||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||
Human Immunodeficiency Virus–Related Malignancies
The archetypal infectious immunodeficiency is that caused by HIV. Three malignancies are considered AIDS-defining: Kaposi’s sarcoma, intermediate- or high-grade non-Hodgkin’s lymphoma, and uterine cervical cancer. However, it is now apparent that other malignancies occur in excessive amounts in HIV-infected patients. These include Hodgkin’s lymphoma as well as carcinomas of the lung, lip, brain, testicle, colorectum, and liver.
For the purposes of discussion of neoplasia, it is important to divide HIV infection into the era before 1996, preceding the highly active antiretroviral therapy (HAART) and the HAART era. In the pre-HAART era, there was a 6.5-fold increased incidence over the general U.S. population. Fraire and Awe38 in 1992 found in the literature 22 patients who were HIV-positive and had lung cancer. In 1995, Flores and associates37 reported another 19 patients and Vyzula and Remick110 reported another 16. Both reports agreed that HIV-positive patients with lung cancer tend to be younger and to have a higher percentage of adenocarcinomas than do other patients. Most have a history of smoking. They usually present at a higher stage and have a more rapidly progressive course than do control groups. Whether there is a true increased incidence of lung cancer in HIV-positive patients is not clear.
Herida and colleagues46 examined in 2005 the incidence of non–AIDS-defining cancers in the pre-HAART and HAART eras. They examined the French Hospital Database on HIV from 1992 to 1999 looking for the incidence of cancers in both men and women other than those that are AIDS-defining. They calculated a standardized incidence ratio (SIR) for each malignancy and found that the incidence of lung cancers was increased in both men and women over that of the general population in the pre-HAART era. In the HAART era, the incidence of lung cancer is still increased over that of the general population. One unexpected finding is that Hodgkin’s disease shows an increased incidence in the HAART era. The incidence of lung cancer appears increased in HIV/AIDS patients over the number of cases in the general population, as demonstrated in Table 127-4. Powles and colleagues85 examined in 2003 the outcome of patients with non-small-cell lung cancer in the HAART era. They matched HIV-positive lung cancer patients with HIV-negative patients who had lung cancer. In the pre-HAART era, HIV-positive patients had a worse prognosis than HIV-negative matched controls. In the HAART era, both groups had a median survival of 4 months and received a similar amount of chemotherapy. In the HIV-positive group, none of the patients died of an AIDS-defining illness or of HIV during treatment.
Proposed Causal Mechanisms of Human Immunodeficiency Virus–Related Malignancies
The HIV-infected patient is at increased risk for developing various malignancies, such as lymphoma and Kaposi’s sarcoma. The pathogenesis of Kaposi’s sarcoma is still uncertain, but several mechanisms are at work. The most important factor is an infection by human herpesvirus-8 (HHV-8). Feller and colleagues36 pointed out in 2007 that HHV-8 has been implicated in all forms of Kaposi’s sarcoma: classic, endemic, iatrogenic, and HIV-associated; the three lymphoproliferative disorders (effusion lymphoma, multicentric Castleman’s disease, and possibly plasmablastic lymphoma). They cite three key pieces of evidence. First, HHV-8 DNA sequences are found in all types of Kaposi’s sarcoma. Second, antibodies to HHV-8 are found in patients who are at high risk for developing Kaposi’s sarcoma, such as homosexuals, HIV-positive patients, and immunocompromised patients. Third, the diagnosis of Kaposi’s sarcoma is preceded by HHV-8 seroconversion and the detection of HHV-8 DNA in the serum. Dittmer and Krown25 emphasized in 2007 that even in the HAART era, the incidence of Kaposi’s sarcoma in HIV-positive patients remains much higher than the general population. The incidence of Kaposi’s sarcoma has decreased in HIV-positive patients since the advent of HAART.
Not all patients who are infected with HIV and HHV-8 develop Kaposi’s sarcoma. There are several factors or stimuli that come into play in a patient who develops Kaposi’s sarcoma. HHV-8 encodes many proteins that are functional analogs of human immunoregulators, growth factors, and cell receptors. Sullivan and associates99 believed in 2006 that the three most important factors in the development of Kaposi’s sarcoma in a patient infected with HHV-8 are viral G protein–coupled receptor (vGPCR), viral IL-6, and viral chemokine homologs. The vGPCR activates the phosphatidylinositol 3-kinase (PI3K) pathway as well as members of the mitogen-activated protein kinase (MAPK) family pathway. Both of these pathways promote growth and antiapoptotic pathways as well as regulating angiogenesis through a transcription factor known as hypoxia inducible factor (HIF)-1α. HIF is ultimately responsible for the production of many gene products involved in angiogenesis. PI3K is lipid kinase; it activates AKT, a kinase that activates the mammalian target of rapamycin (mTOR), which itself is a kinase that plays an important role in cell proliferation and survival. The importance of the mTOR pathway was emphasized in 2005 by Stallone and colleagues.97 They described 15 kidney transplant recipients who had biopsy-proven Kaposi’s sarcoma. Upon the diagnosis of Kaposi’s sarcoma, the cyclosporine was discontinued and they were treated with sirolimus (rapamycin), also an immunosuppressant. At the end of 6 months, the cutaneous lesions had disappeared and a repeat biopsy in the same area showed no residual Kaposi’s sarcoma. This finding suggests that shutting down the mTOR pathway may be a treatment for Kaposi’s sarcoma. In addition to these actions, vGPCR activates the Janus kinase (Jak)/signal transducer and activator of transcription (STAT) pathway. Activation of the Jak/STAT pathway plays a role in angiogenesis and the transformation in hematologic and solid malignancies. vGPCR activates the transcription of nuclear factor-κB, which plays an important role in the suppression of apoptosis and cell cycle regulation.
IL-6 is induced by HHV-8 and it has a variety of functions, including regulation of the immune system. It is a viral homolog that acts as a growth factor. HHV-8 also produces viral homolog of macrophage-inhibitory proteins (chemokines), which probably play a role in angiogenesis. Kaposi’s sarcoma also appears to pirate cellular growth and angiogenesis pathways such as vascular endothelial growth factor (VEGF), angiopoietins, insulin-like growth factor, platelet-derived growth factor (PDGF), and matrix metalloproteinases (MMPs).
Feller and associates36 also point out that HIV plays an important role in the development of Kaposi’s sarcoma. HIV transactivation (Tat) protein, mediated through IFN-γ, has the ability to induce endothelial cell proliferation and facilitate invasion of the extracellular matrix. HIV Tat may be involved in upregulating HHV-8 lytic genes, which have the potential to transform endothelial cells. HIV infection increases the expression of immunoregulatory cytokines, including tumor necrosis factor-alpha (TNF-α), IL-1β, IL-8, and IL-6. Some of these cytokines can induce HHV-8 gene expression and angiogenesis.
Besides the EBV theory of the etiology of lymphoma described previously, HIV itself exerts a strong influence on the lymphatic system. Knowles,51 in his 1997 review of HIV lymphomagenesis, concluded that HIV is not directly involved in the malignant transformation of B cells or, consequently, in the induction of B-cell lymphomas. Grogg and colleagues,42 in a 2007 review of HIV and lymphomas, believe that HIV contributes to the development of lymphoma both by indirect and direct mechanisms. They believe that the predominant contribution of HIV to lymphomagenesis is through indirect mechanisms including the degree of immunosuppression, induction of cytokines leading to B-cell proliferation, and infection with EBV and HHV-8. EBV is present in about 40% to 50% of HIV-associated lymphomas. The direct mechanisms involve certain HIV gene products, particularly Tat, which has been implicated as an activator of cellular genes such as IL-6 and IL-10. Tat can also interfere in cell cycle control through interaction with the regulatory protein Rb2/p130. Experiments performed in vitro show that HIV infection of B-cell lines derived from EBV seropositive individuals leads to B-cell immortalization, dysregulation of MYC (also known as c-myc), and activation of EBV. Laurence and Astrin58 showed in 1991 that HIV infection of immortalized B-cell lines results in the upregulation of c-myc. c-myc is a protooncogene that is involved in cell proliferation. In these ways, HIV can directly contribute to lymphomagenesis.
Second-Neoplasm Syndromes
During the 1970s, transplantation was offered to patients who had a history of a malignancy or were receiving chemotherapy for existing cancers. Penn81 found in 1976 that there was a 4% incidence of new malignancies in the group with a preexisting malignancy, which was not different from the 6% incidence of de novo cancer development in patients with no evidence of cancer before transplantation. However, he found that 166 new malignancies began in 160 patients receiving chemotherapy for 161 tumors. This striking occurrence was blamed directly on the combination of immunosuppression and anticancer chemotherapy. Today, strict criteria are used for selecting cancer patients for possible transplantation; cancers must be low-grade malignancies, and the patients must be disease-free for at least a year. In 2006, Ladowski and colleagues57 reviewed their experience with heart transplants in patients who had previously been treated for malignancies. These investigators found that the 10-year survival was very similar for patients with no previous malignancy (63%) and those with a previously treated malignancy (62%). They recommended at least a 1-year disease free interval prior to undergoing heart transplant. Koerner and associates53 agreed with this 1-year disease-free interval. They also cautioned about transplanted patients with myeloma, because three of their five patients died. The follow-up period for the two survivors was only 9 and 14 months.
A special group of patients is made up of those who survived aggressive chemotherapy 20 or more years previously only to develop second cancers. Patients who were treated for Hodgkin’s lymphoma fall into this group because they were young at the time of diagnosis, have a long life expectancy, and their diseases is treatable. The first second malignancy described for this group was leukemia, and the survival was generally less than a year. Ng and Travis77 in 2008 believed that the risk was due to the alkylating chemotherapy. Since the chemotherapy has shifted to Adriamycin, bleomycin, vinblastine and dacarbazine (ABVD), the risk for subsequent leukemia has decreased. These patients are also at greater risk for non-Hodgkin’s lymphoma, breast cancer, and lung cancer. Both the breast and lung cancers are associated with the radiation field as well as the dose of radiation. In the case of lung cancer, tobacco use may also play a
role. In 2008, Hodgson47 described the necessary screening for survivors of Hodgkin’s lymphoma. In addition to screening for lung and breast cancers, he pointed out that patients needed to be screened for colorectal cancer and, in the case of women, cervical cancer.
role. In 2008, Hodgson47 described the necessary screening for survivors of Hodgkin’s lymphoma. In addition to screening for lung and breast cancers, he pointed out that patients needed to be screened for colorectal cancer and, in the case of women, cervical cancer.
Analysis by van Leeuwen’s group108 in 1994 found that risk factors for the development of second cancers in Hodgkin’s disease included chemotherapy during the first year, follow-up chemotherapy, age >40 years at first diagnosis, splenectomy, and advanced stage. They also discovered a 3.5-fold increased rate of cancer among 1,939 Hodgkin’s patients over that expected in the general population and that the second cancers, in decreasing frequency, were leukemia, non-Hodgkin’s lymphoma, lung cancer, gastrointestinal cancers, urogenital cancers, melanoma, and soft tissue sarcoma. Women under 20 years of age who had been treated with mantle radiation had a 40-fold increase in breast cancer. Risk for developing lung cancer was strongly related to treatment with thoracic irradiation (Fig. 127-2). These patients usually have lesions in the apex of the lung, which may be bilateral in those who had mantle radiation.
Pulmonary Tumors in Immunosuppressed Patients
In addition to lung cancer, the neoplasms most likely to afflict the lungs in AIDS patients are non-Hodgkin’s lymphoma, Kaposi’s sarcoma, and Hodgkin’s lymphoma. In immunosuppressed transplant patients, Buell and colleagues12 pointed out that the malignancies can vary somewhat depending on the age of the patient (pediatric or adult) and the type of graft (heart, liver, kidney, or lung). In the pediatric transplant population, PTLD is the most common posttransplant neoplasm, including lymphomas. In the adult population, skin cancers are the most common neoplasm, followed by PTLD. Other neoplasms occurring in adults are Kaposi’s sarcoma and malignant melanoma. Roithmaier and colleagues92 in 2007 reviewed the incidence of malignancies in 907 patients who had received heart (424), single-lung (200), heart–lung (56), and double-lung (227) transplants. The mean age at transplantation was 46.4 years, with a median survival of 8.6 years. In their group, there were 102 cancers, which is a 7.1-fold increase over the nontransplant population. The most common cancers were PTLD, head and neck cancer, and lung cancer. This incidence translates into a 26.2-, 21-, and 9.3-fold increase over the nontransplant population. Wimmer and colleagues112 in 2007 reviewed the 25-year renal transplant experience of the Munich Transplantation Center. They found that after 25 years, their patients had a cumulative incidence of cancer of 49.3%. Excluding the nonmelanoma skin cancers, the incidence dropped to 39.7%. Their patients developed a variety of malignancies including PTLD, lung cancer, and Kaposi’s sarcoma.
Kaposi’s Sarcoma
Kaposi’s sarcoma is a low-grade vascular neoplasm that manifests itself as one of four variants: classic Kaposi’s sarcoma, endemic (African) Kaposi’s sarcoma, iatrogenic (organ-transplant) Kaposi’s sarcoma, and AIDS-related Kaposi’s sarcoma. The exact etiology of Kaposi’s sarcoma is unknown, but the view of Angeletti and colleagues2 in 2008 was that HHV-8, which is also known as Kaposi’s sarcoma-associated herpesvirus (KSHV), plays a major role in its development. Other factors, such as immunosuppression, are also necessary for the development of Kaposi’s sarcoma. The incidence of pulmonary Kaposi’s sarcoma (KS) is difficult to determine. Since the advent of HAART, the incidence of KS has clearly declined. Angeletti and colleagues2 point out that in a Swiss study, the standardized incidence ratio for KS for those patients taking HAART was 25, in contrast to 239 for those who were not receiving the treatment. In the pre-HAART era, Meduri and associates67 in an autopsy study in 1986 found KS in the lungs of 47% of patients with cutaneous lesions. In the pre-HAART era, patients with pulmonary KS survived about 4 months, but during the HAART era, in 2006, Palmeiri and associates80 found that these patients survive an average of 1.6 years.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree