Fig 1 a–d.
A 53-year-old man who underwent chest radiography for pain in the right axilla. Posteroranterior (a) and lateral (b) radiographs were interpreted as normal. With hindsight bias from MDCT, the right apical mass is obvious. MDCT coronal and sagittal images with soft tissue (c) and bone (d) windows show a right apical mass with bone destruction
Radiological errors can be divided into two types [35]: cognitive, in which an abnormality is seen but its nature is misinterpreted and perceptual, or the “miss,” in which a radiological abnormality is not seen by the radiologist on initial interpretation. The perceptual type is estimated to account for approximately 80% of radiological errors [36].
Our second patient illustrates the complexity of the detection of a lung nodule located close to the hilum. A 77-year-old man with known prostate cancer underwent chest radiography for right upper quadrant abdominal pain (Fig. 2a, b). The radiographs were reported as normal. The coronal and sagittal reformats demonstrated the position of the nodule (Fig. 2c, d), which, with the benefit of hindsight, can be seen clearly on the posteroanterior and lateral chest radiographs.
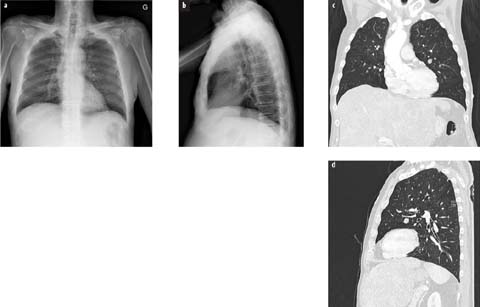
Fig 2 a–d.
A 77-year-old man with right upper quadrant pain. Posteroranterior (a) and lateral (b) radiographs were interpreted as normal. With hindsight, the 13-mm nodule in the superior segment of the lingula can be seen. Coronal (c) and sagittal (d) reformats (lung window) show the position of the lingular nodule, close to the hilum
Nodular Lesions: Infections
Nodular lesions attributed to pulmonary infections are most often seen in nosocomial pneumonias and in immunocompromised patients. They may be caused by bacteria such as Nocardia asteroides and Mycobacterium tuberculosis, septic emboli, and fungi. Nocardia asteroides causes single or nodular infiltrates with or without cavitation. Invasive pulmonary aspergillosis (IPA), mucor, and Cryptococcus neoformans may present with single or multiple nodular infiltrates, which often progress to wedge-shaped areas of consolidation. Cavitation is common later in the course of the infiltrate. In the appropriate clinical setting, CT may aid in the diagnosis of IPA by demonstrating the “halo sign.” Figure 3 shows the imaging results from a 43-year-old woman with fever after a bone marrow transplant. The posteroranterior radiograph was interpreted as normal (Fig. 3a). With hindsight, a subtle infiltrate can be seen at the left apex. Conspicuity is lessened by the overlying clavicle and 1st rib. The axial CT image (Fig. 3b) shows nodular consolidation with crescentic cavitation (the “crescent sign”) and a surrounding ground-glass infiltrate (the “halo sign”). These characteristic findings of IPA are best identified on CT.
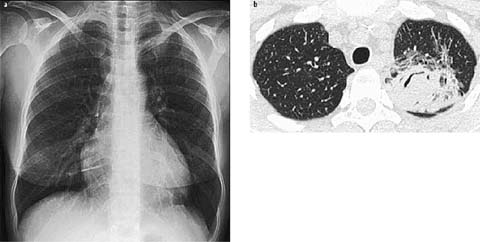
Fig 3 a, b.
A 43-year-old woman with fever after a bone marrow transplant. The posteroranterior radiograph was interpreted as normal (a). With hindsight, a subtle infiltrate can be seen at the left apex. Conspicuity is lessened by the overlying clavicle and 1 st rib. Also note the in-dwelling catheter from the left brachial vein to the superior vena cava. Axial CT image (lung window) shows nodular consolidation with crescentic cavitation (“air-crescent sign”) and a surrounding ground-glass infiltrate (“halo sign”) (b)
Missed Consolidations
Airspace Disease
Airspace disease is usually caused by bacterial infections. However, it can be seen in viral, protozoal, and fungal infections as well as malignancy, typically brochioloalveolar carcinoma [37]. Acute airspace pneumonia is characterized by a mostly homogeneous consolidation of lung parenchyma and well-defined borders; it does not typically respect segmental boundaries. An air bronchogram is very common. Progression to lobar consolidation may occur. As with lung nodules, whether consolidation is detected or missed on the plain chest radiograph may depend on a combination of the same factors of size, density, location, and overlying structures. Location is a significant factor for missed consolidations [38, 39]. Consolidations in the middle lobe and both lower lobes can be difficult to diagnose, especially when only the posterioranterior view is obtained [40]. Figure 4 shows the radiographs from a 46-year-old woman with cough and right-sided chest pain. The posteroanterior radiograph was interpreted as normal (Fig. 4a). Due to a clinical suspicion of pulmonary embolism, MDCT was requested, which showed consolidation in the anterior segment of the right lower lobe. The coronal and sagittal reformats demonstrated the extent of the consolidation (Fig. 4b, c). There were no signs of pulmonary embolism on the contrast medium study. A diagnosis of right lower lobe pneumonia was established and the patient was treated successfully with antibiotics.
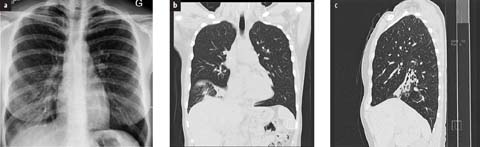
Fig 4 a–c.
A 46-year-old woman with cough and right-sided chest pain. The posteroranterior radiograph was interpreted as normal (a). Coronal (b) and sagittal (c) reformats showing consolidation in the anterior segment of the right lower lobe
Chest radiography is the most frequently performed diagnostic investigation requested by general practitioners in Europe [41]. Chest radiography is considered the gold standard for the diagnosis of pneumonia. It can be used to diagnose pneumonia when an infiltrate is present and to differentiate pneumonia from other conditions that may present with similar symptoms, such as acute bronchitis. The results of the chest radiograph may in some cases suggest a specific etiology (for example, a lung abscess) or reveal a complication (empyema) or coexisting abnormalities (bronchiectasis, bronchial obstruction, interstitial lung disease). Chest radiography remains a valuable diagnostic tool in primary-care patients with a clinical suspicion of pneumonia as it substantially reduces the number of misdiagnosed patients [42]. MDCT can help in differentiating infectious from non-infectious abnormalities and may detect empyema, cavitation, and lymphadenopathy when the chest radiograph cannot. MDCT imaging is useful in patients with community-acquired pneumonia when there is an unresolving or complicated chest radiograph and should be performed in immunocompromised patients with a clinical suspicion of pneumonia when the chest radiograph is normal. This is especially true when the early diagnosis of pneumonia is critical, as is the case with immunocompromised and severely ill patients [43].
Figure 5 shows the imaging studies from a 38-year-old immunocompromised man with fever. The posteroanterior and lateral radiographs (Fig. 5a, b) were interpreted as showing a peri-hilar reticular infiltrate with right upper lobe consolidation. MDCT was requested to further characterize the infiltrate and revealed ground-glass opacification with bilateral lung cysts (Fig. 5 c–e). Pneumocystis pneumonia was confirmed by bronchoalveolar lavage.
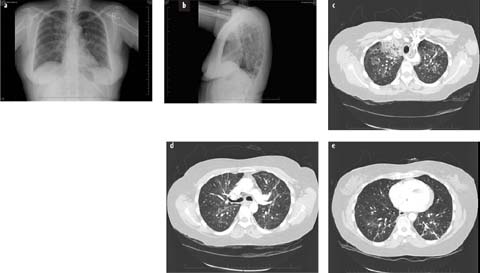
Fig 5 a–e.
A 38-year-old immunocompromised man with a fever. Posteroranterior (a) and lateral (b) radiographs show a perihilar reticular infiltrate with right upper lobe consolidation. c–e Axial CT images show bilateral lung cysts in addition to consolidation in the right upper lobe with patchy ground-glass opacification in both lungs. Pneumocystis pneumonia was confirmed by bronchoalveolar lavage. Note the retro-esophageal right subclavian artery
Missed Interstitial Lung Disease
Diffuse (Interstitial or Mixed Alveolar-Interstitial) Lung Disease
Diffuse lung disease presenting with widely distributed patchy infiltrates or interstitial reticular or nodular abnormalities can be produced by a number of disease entities. An attempt is usually made to separate the group of idiopathic interstitial pneumonias from known causes, such as infections, associated systemic disease, or drug-related. The most common infectious organisms are viruses and protozoa. In general, the etiology of an underlying pneumonia cannot be specifically diagnosed because the patterns overlap. It is beyond the aim of this chapter to discuss in detail the contribution of MDCT to the diagnosis of diffuse infiltrative lung disease. The development of HRCT has resulted in markedly improved diagnostic accuracy in acute and chronic diffuse infiltrative lung disease [44–47]. The chest radiograph remains the preliminary radiological investigation of patients with diffuse lung disease but is often non-specific. Pattern recognition in diffuse lung disease has been the subject of controversy for many years. Extensive disease may be required before an appreciable change in radiographic density or an abnormal radiographic pattern can be detected on the plain chest radiograph. At least 10% of patients who are ultimately found to have biopsy-proven diffuse lung disease have an apparently normal chest radiograph [48]. HRCT, and now MDCT, have become integral components of the clinical investigation of patients with suspected or established interstitial lung disease. These techniques have had a major impact on clinical practice [49, 50].
Key Signs for Reducing the Risk of Errors on Chest X-rays
Deep Sulcus Sign
The deep sulcus sign (Fig. 6) is seen on chest radiographs obtained with the patient in the supine position [51]. It represents lucency of the lateral costophrenic angle extending toward the abdomen. The abnormally deepened lateral costophrenic angle may have a sharp, angular appearance. In the supine patient, air in the pleural space (pneumothorax) collects anteriorly and basally within the nondependent portions of the pleural space; when the patient is upright, the air collects in the apicolateral location. If air collects laterally rather than medially, it deepens the lateral costophrenic angle and produces the deep sulcus sign. In Fig. 6, a deep sulcus sign is seen on the left, in addition to a continuous diaphragmatic sign, present when there is air between the diaphragm and the heart.
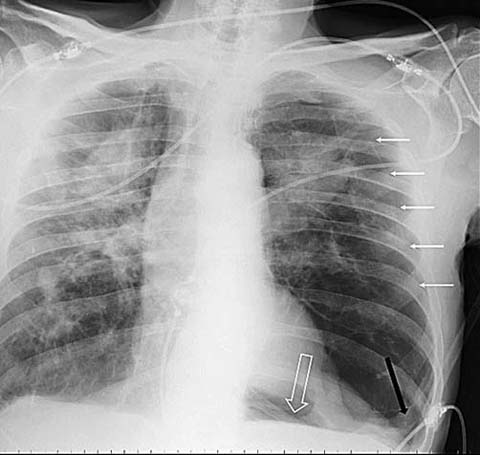
Fig 6.
A 78-year-old man with acute left chest pain and a previous history of pneumoconiosis. Bedside chest radiograph shows a thin white line near the left chest wall (white arrows), corresponding to the left lung visceral pleura, and indicating a pneumothorax. The deep lucency of the left lateral costophrenic angle extending towards the abdomen is an indirect sign of pneumothorax (black arrow). The continuous diaphragmatic sign is also seen as air separating the diaphragm from the heart (white hollow arrow)
Spine Sign
On the normal lateral chest radiograph, the attenuation decreases (the lucency increases) as one progresses down the thoracic vertebral bodies [52]. If the attenuation increases, locally or diffusely, there must be a posteriorly located lesion (Fig. 7). This lesion might not be seen on the frontal view, as it might be hidden by the heart or the hila.
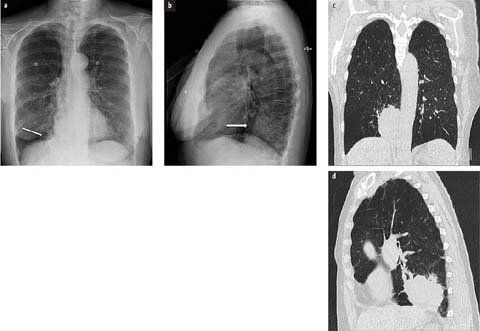
Fig 7 a–d.
A 69-year-old woman with chronic obstructive pulmonary disease and hemoptysis. The posteroanterior chest radiograph (a) shows an opacity next to the right border of the heart (arrow) and obliterating the right side of the spine. This “silhouette sign” of the right posterior mediastinal border indicates that the lesion is in a posterior location in the right lower lobe. Lateral view (b) shows an increased density (arrow) of the lower spine compared with the upper and middle thoracic spine (“spine sign”). This increased density is due to a large mass in the right lower lobe. Coronal CT image (c) shows the right lower lobe mass obliterating the border of the mediastinum. The sagittal CT image (d) shows the posterior location of the mass
Silhouette Sign
In a chest X-ray, non-visualization of the border of an anatomic structure that is normally visualized shows that the area neighboring this margin is filled with tissue or material of the same density [53]. The silhouette sign is an important indicator of the presence and localization of a lesion.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


