CHAPTER 20 Lung Cancer
Surgical Strategies for Tumors Invading the Chest Wall
Lung cancer continues to be the leading cause of cancer-related deaths in both men and women. More than 75% of non–small cell lung cancer (NSCLC) is advanced in stage at presentation, with extensive locoregional disease or distant metastasis. The majority of resectable lung cancers are confined to the pulmonary parenchyma, but 5% to 8% extend beyond the lungs and invade the pleura, soft tissues, or osseous structures of the chest wall.1,2 Chest wall invasion for surgical staging (T3) is defined as any tumor involvement into or beyond the parietal pleura. Pathologists can further describe these tumors by their depth of chest wall invasion, but this is infrequently reported in this subset of T3 patients.
HISTORICAL NOTE
Historically, chest wall invasion by a tumor of any histology was considered unresectable. Early surgical experience demonstrated that the surgical violation of the parietal pleura resulted in a sucking chest wound with immediate pulmonary collapse, often leading to the rapid demise of the patient. Dr. M. Michellau presented to the Institute of France in Paris in March of 1818 with a fungating mass protruding from his left chest wall. Dr. Richerand proposed a resection of the involved rib and pleura, an unprecedented operation at that time. On March 31, 1818, Dr. Richerand resected the left sixth and seventh ribs of Dr. Michellau, but acute respiratory distress occurred unexpectedly as the chest cavity was entered. The patient was saved bycovering the aperture with a linen cloth plastered with cerate. Despite a rocky postoperative course, Dr. Michellau survived and returned home 27 days postoperatively. The pathology of the lesion is not known, but a primary rib malignancy is suspected.3
In the summer of 1883, a brilliant young surgeon, H. M. Block, in what was then called Danzig, East Prussia (now Gdansk, Poland) carried out the first planned pulmonary resection. Dr. Block had performed successful open chest surgery on experimental animals and was eager to apply his experience to humans.4 He chose a young female relative with a diagnosis of bilateral pulmonary tuberculosis and performed a thoracotomy to resect her diseased lung. Although the details of the operation are not known, we do know that it had a tragic end. A few days later, the short, brilliant career of Dr. Block ended with a self-inflicted gunshot wound to the head.5
Murphy6 described his experiments and clinical experiences with open pneumothorax during his address to the American Medical Association in 1898. Parham,7 in 1899, was the first in the United States to report resection of a bony chest wall tumor involving three ribs. A controlled pneumothorax with soft tissue coverage was created. This patient survived, but many who followed did not.
Major surgical and anesthesia advances were introduced in 1904 at the German Surgical Congress in Berlin. Two techniques designed to surmount the open chest problem were proposed. Ferdinand Sauerbruch,8 from the surgical clinic of von Mickulykz at the University of Breslau, introduced his method of unterdruck (low-pressure) ventilation. Lung expansion was maintained after thoracotomy by keeping an experimental animal’s body inside a negative-pressure chamber (at −15 cm H2O) while the head remained outside the chamber with the anesthesiologist. Brauer9 described the benefits of uberdruck (high pressure) anesthesia, in which the lung was kept expanded by placing the patient’s head in a glass positive-pressure chamber.
In the late 1800s, two physicians from New York, Joseph O’Dwyer and George Fell, described intubation techniques and positive-pressure ventilation. Dr. O’Dwyer developed a practical method of endotracheal intubation for the treatment of diphtheria, which was applied in thousands of cases and resulted in a gratifying decrease in the mortality rate of that dreaded disease.10,11 Dr. Fell used a crude device to maintain ventilation in patients suffering from drug overdoses.12 In New Orleans, Parham and Matas used the combined Fell-O’Dwyer apparatus in 1898 to administer positive-pressure surgical anesthesia.13
The use of positive-pressure ventilation identified the need for cuffed endotracheal tubes for the reliable delivery of anesthesia to the lungs. Eisenmenger first described a cuffed endotracheal tube in 1893. Placement of such tubes was facilitated by Kirstein,14 who introduced direct laryngoscopy in 1895 for safe, reliable placement of endotracheal tubes in the trachea. In 1907, Chevalier Jackson improved the laryngoscope and produced the instrument that is still in use today and bears his name.15 A practical endotracheal tube design for general use was introduced by Guedel in 1928,16 and its use became widespread starting in the 1930s. In 1938, the first operative use of ventilators was made with the Freckner Spiropulsator, developed in Sweden. In 1942, Griffith, in Montreal, Canada, introduced curare to facilitate intraoperative controlled ventilation.17
In 1947, Coleman18 reported long-term survival after en bloc excision of the chest wall with pulmonary resection. Concurrently, significant strides in chest wall reconstructive techniques were occurring through the use of fascia lata grafts, autogenous rib grafts, large cutaneous flaps, and latissimus dorsi muscle flaps, as described by Campbell in 195019 and Grillo and colleagues in 1966.20 In the past 40 years, we have witnessed further refinements in surgical procedures, the use of prophylactic antibiotics, improved anesthesia delivery and monitoring, and the implementation and use of critical care units for postoperative ventilation. Today, these advances permit the safe and effective resection of locally advanced lung cancer with extensive chest wall involvement on a routine basis.
Pancoast tumors comprise a distinct surgical entity and are discussed separately (see Chapter 21).
DEMOGRAPHICS AND SYMPTOMS
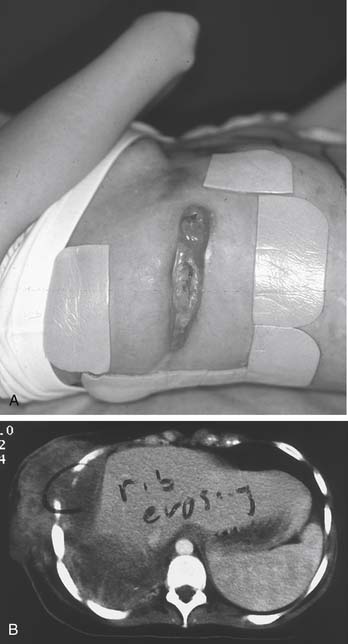
Patients with lung cancer are usually 50 to 70 years old. Lung cancer is rarely seen in patients younger than 30 years, although with the ongoing epidemic of children and young teenage smokers, advanced lung cancer can be seen even in younger age groups (Fig. 20-1). Lung cancer with chest wall invasion most typically presents in patients in their 7th decade, with a median age of 64 to 66 years (range, 38 to 93 years).21–23 Overall, lung cancer incidence and mortality continue to be disproportionately higher in men than in women, although the gap is narrowing. Lung cancer with chest wall invasion has an overwhelming predominance in men; women represent only 10% to 30% of patients in several recent studies.2,21–23 A current or previous smoking history is elicited in approximately two thirds of patients, with an average 50-pack-year history per patient.2,21
Patients whose lung cancer has invaded the chest wall have similar presenting symptoms, including chest pain (40% to 60%), cough (14%), recurrent lower respiratory tract infection (10% to 25%), weight loss (10% to 18%), hemoptysis (12%), and dyspnea (11%). However, as many as 25% of patients can be asymptomatic (Table 20-1).2,21,22
Table 20–1 Presenting Symptoms in Patients with Lung Cancer with Chest Wall Invasion
| Presenting Symptom | Occurrence(%) |
|---|---|
| Chest wall pain | 40-60 |
| Recurrent lower respiratory tract infection | 10-25 |
| Weight loss | 10-18 |
| Hemoptysis | 12 |
| Dyspnea | 11 |
| Cough | 11 |
| Asymptomatic | 25 |
The right lung has a slight predominance for the location of lung cancers, both in general and for those with chest wall invasion.2 Okada and coworkers described a marked predilection for the upper lobes in their series of lung cancers that invade the chest wall, although not all series confirm this finding.23 Lung cancers in general have a slight predilection for upper lobes rather than lower lobes, which theoretically may be related to the relative increase in ventilation (and associated carcinogens) to the upper portions of the lungs.
Squamous cell carcinoma is the classic smoking-related tumor, and for many years it was the most common histology. In recent years, however, adenocarcinoma has overtaken squamous cell carcinoma as the most common lung cancer worldwide. Several series of patients with lung cancer invading the chest wall have demonstrated that squamous cell carcinoma remains the most common, followed closely by adenocarcinoma; large cell carcinoma and adenosquamous carcinoma comprise fewer of these tumors.2,22,23 Average tumor diameter in these patients, by computed tomography (CT) measurements, was 6.5 cm; tumors ranged from 2 to 18 cm in maximum diameter.2
DIAGNOSIS
Peripheral lung lesions with the suggestion of chest wall involvement may require additional radiographic testing to confirm invasion. These radiographic techniques include CT scans, nuclear medicine (scintigraphic) bone scans, magnetic resonance imaging (MRI), and positron emission tomography (PET) scans. Although gross tumor involvement of the chest wall is easily diagnosed with these radiographic modalities, confirmation of isolated parietal or mediastinal pleural invasion is more difficult and often unreliable.24–27
The use of CT scans has greatly increased the precision of tumor localization, has allowed accurate evaluation of contiguous organ involvement, has improved assessment of lymph nodes, and has improved the identification of pulmonary metastasis. A CT scan is excellent for assessing rib destruction and intercostal muscle tumor extension, but it is relatively inaccurate for invasion limited to the parietal or mediastinal pleura.24,25,27 Helical three-dimensional reconstruction has been shown to be superior to standard two-dimensional images, but the latter technology is universally used.28 Shirakawa and associates29 identified patients who had parietal pleural invasion by using inspiratory and expiratory CT scans. They demonstrated that a respiratory phase shift of greater than one half of a vertebral body height in middle and lower lobe tumors reliably predicted the absence of parietal pleural invasion. The accuracy and negative predictive value were 90% and 86%, respectively, in tumors located in the lower and middle lobes. For upper lobe tumors, however, the respiratory phase shift did not correlate with operative findings regardless of whether invasion was present. This discrepancy results from the minimal normal respiratory phase shift of these lung fields when the patients were studied in the supine position.
MRI has the advantages of multiplanar reconstruction and high differential signal intensity, which are invaluable for determining vascular invasion and spinal involvement. Conventional MRI, unfortunately, is just as limited as CT for evaluation of parietal and mediastinal pleural invasion. Kodalli and associates26 used breath-hold inspiration and expiration MRI to assess parietal pleural invasion. Pleural invasion was excluded when tumor displacement exceeded 5 mm in reference to chest wall structures or relevant mediastinal structures (e.g., the aortic arch). This study identified 100% sensitivity and specificity for pleural invasion of tumors located in the middle lobe and basilar segments of the lower lobes. Studies of upper lobe tumors and those located in the apical segments of the lower lobes demonstrated a positive predictive value of only 40% but a negative predictive value of 100%. The superiority of MRI to CT lies in its ability to assess lung and diaphragm movement in a coronal plane. Insufficient respiratory motion is evident by a less-than-1-cm movement of the diaphragm on coronal images, and necessary scans could be repeated by asking the patient to take a deeper breath.
In a recent report, ultrasonography (US) was compared with CT for detection of chest wall involvement. In this series, 90 patients with suspected chest wall involvement were evaluated preoperatively with CT and US. Their ultrasound criteria for determining chest wall invasion were any two of the following: (1) tumor ingrowth seen into the chest wall, (2) interruption of the pleural reflection, (3) invasion of the ribs, and (4) impairment of movement with respiration. Using these criteria, US was deemed more sensitive than CT (89% versus 42%) with similar specificity (95% versus 100%).30 Perhaps the real-time imaging of ultrasound during respiration leads to more accurate imaging data.
More invasive methods have been used for detection of parietal pleural invasion, including the use of expiratory dynamic CT after the introduction of a diagnostic pneumothorax.31,32 Lack of invasion was diagnosed on the basis of an air space between the mass and adjacent structures. Sensitivity was 100% in both studies for chest wall invasion, although sensitivity dropped to 76% in cases of mediastinal invasion. Specificity for tumor involvement was 80% in the study by Watanabe and colleagues.31 Benign pleural adhesions caused false-positive results in both of these studies. Complications were reported as mild and included chest pain, shortness of breath, and subcutaneous emphysema.
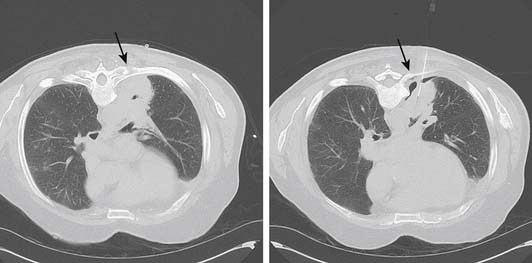
Despite these results from a variety of imaging techniques, we do not use these special imaging studies. We feel that these tests are not warranted because they may subject high-risk patients to a pneumothorax and ultimately are unlikely to alter the planned operative procedure. In some cases, reviewing the CT scans obtained during transthoracic needle biopsy reveals minimal pneumothoraces, incidentally obtained as a result of biopsy. Often, these images show clear separation from the chest wall (Fig. 20-2).
STAGING
Surgical-pathologic staging is performed according to the International Staging System for Lung Cancer, using information about the primary tumor (T), nodal status (N), and distant metastasis (M).33 T status denotes characteristics of the primary tumor, including size, location, and local aggressiveness. Chest wall involvement increases the T status to T3. Chest wall involvement, however, includes a wide pathologic spectrum, from invasion of the parietal pleura only, to full-thickness chest wall replacement by tumor. Other characteristics that denote T3 status include invasion of the diaphragm, mediastinal pleura, or parietal pericardium, or a tumor in a main-stem bronchus 2 cm or less from the carina but not involving the carina. Full-thickness invasion into the mediastinum, including the heart, great vessels, trachea, or vertebral bodies, denotes a T4 classification. Pancoast tumors by definition are at least T3 because of the chest wall invasion. Further invasion with involvement of the subclavian artery or vein or the brachial plexus is not specifically described in the staging system, although we consider them T4 because of their poorer prognosis. Satellite lesions located in the involved lobe also denote T4 classification, but they will be considered T3 under the International Association for the Study of Lung Cancer (IASLC) proposed changes to the staging system.34 Most T4 tumors are not considered suitable for surgical resection, although those patients in whom an R0 resection (microscopically negative margins) is possible may be treated surgically.
In 1997, an important change was made to the TNM staging system regarding tumors with chest wall involvement. NSCLC defined as T3N0M0 was classified as stage IIIA by the prior system described by Mountain in 1986.35 Survival data of patients with these tumors revealed that their clinical course with surgery alone was more favorable than that of other patients with stage IIIA disease (i.e., those with hilar or mediastinal lymph node involvement: T3N1, T3N2, T1N2, or T2N2). Subsequently, T3N0M0 tumors were down-staged to stage IIB with this revision.
Changes on the horizon for the TNM staging system are proposed but have not been implemented at this time.34 The proposed changes are included in the upcoming 17th edition of the IASLC staging manual. Same-lobe satellite lesions will be down-staged from T4 to T3, and there are new size criteria for the different T groupings. However, the proposed changes will not alter the management or staging of tumors with chest wall invasion, which will still be classified as T3. The staging of T3N0 will still be considered stage IIB, and T3N1 or T3N2 will still be considered stage IIIA.
Despite advances in imaging techniques, mediastinoscopy still remains the most sensitive and specific test for evaluating the mediastinal nodes and should be considered before any major chest wall resection. Another option for staging the mediastinum is endobronchial ultrasound (EBUS)-guided fine-needle aspiration. EBUS involves the use of a specially designed bronchoscope with an ultrasound transducer at the tip allowing real-time image guided biopsy of nodes adjacent to the airway, and it can access some nodes at levels 10, 11, and 12.36,37 Sensitivity and specificity of EBUS have been reported to be higher than those of CT or PET and comparable with those of mediastinoscopy, and it is less invasive.38 Because of the anatomic location, the preoperative assessment of N1 disease is more problematic via mediastinoscopy, but these nodes are easily reached with EBUS. Patients with T3N1 disease should still be considered for en bloc resections, and they have a better survival rate than those with N2 disease.
Although it is unlikely that peripheral lung tumors involving the chest wall extend into the airway, it is our practice to perform bronchoscopy immediately before resection to identify any unsuspected endobronchial disease and to assess the airway anatomy. Navigational bronchoscopy can access peripheral tumors out of the range of standard bronchoscopy to obtain tissue for diagnosis39; although this is not commonplace today, it may have a more widespread role for biopsying peripheral tumors in the future.
Extrathoracic metastases are found in up to 50% of patients with newly diagnosed lung cancer.40 Patients with symptoms suggestive of central nervous system involvement are evaluated with an MRI scan of the brain. Symptoms or laboratory findings suggestive of disseminated malignancy, such as weight loss, bone pain, or elevated alkaline phosphatase, are evaluated with bone scintigraphy scans.
Bone scintigraphy scans are used to detect occult bony metastases and confirm bony lesions in symptomatic patients. The vertebral column is the most commonly affected region for bone metastases. MRI is accepted as the most accurate imaging modality in detecting bone metastases in the vertebral column, and focal imaging can be guided by bone scan abnormalities or symptoms.41–43 Suspect uptake in bones other than the vertebral column also requires further investigation, although MRI scans become less useful. False positives are seen in the bony thorax when a history of rib fractures or trauma is noted. False negatives can be appreciated when bone scans are correlated with PET scans. Positive lesions on PET scans, which are not seen on bone scans, may represent soft tissue metastasis.44 Durski and associates44 recommend that all patients be staged with a PET scan, and that bone scans should be performed only if symptomatically indicated when PET scans are negative. In their series, the use of bone scans in addition to PET scans did not change the clinical stage of any of their patients, although it allowed more precise localization of skeletal abnormalities.
PET scans using [F18]fluorodeoxyglucose (FDG) are routinely used in addition to CT scans for both initial diagnosis and staging of NSCLC. One study suggests that obtaining both a PET and a CT scan is more cost-effective than performing a CT scan alone for staging.45 The reported sensitivity and specificity of PET for thoracic lymph node involvement are 70% to 100% and 81% to 100%, respectively. CT has a sensitivity and specificity of 25% to 81% and 56% to 94%, respectively.46–50 The American College of Surgeons Oncology Group trial ACOSOG Z0050 evaluated the usefulness of PET for staging NSCLC. The results support staging all NSCLC patients with PET to reduce the rate of nontherapeutic thoracotomy, but they recommend confirming PET-positive mediastinal nodes with mediastinoscopy. In addition, their recommendations include using PET to guide tissue biopsy in the cases of suspected single-site distant metastases.51 Integrated PET-CT was compared with PET alone in a prospective blinded trial in which the same radiologist read an integrated scan, and at a later date was asked to read the PET images only. Integrated PET-CT was shown to be more accurate at predicting T and N status of patients, and better at determining stage I and stage II disease.52 Integrated PET-CT scans have become standard for preoperative evaluation of all our patients with NSCLC.
TREATMENT
Patients with confirmed N2 disease who are devoid of distant metastatic disease are offered a treatment protocol with induction chemotherapy. Surgery is offered to those patients whose tumors show an objective response to chemotherapy and whose disease can be completely resected.22 Progression of disease while on chemotherapy is generally regarded as a contraindication to surgery, as is evidence of N3 disease. Preoperative radiation therapy has not been shown to increase survival in several studies, but it has demonstrated an increased operative mortality.1,22,53 Preoperative radiation therapy therefore is not used at our institution.