INTRODUCTION
Learning Objectives
The student will be able to describe the epidemiology and risk factors for lung cancer.
The student will be able to enumerate the major histologic types of lung cancer and differentiate how cell types affect tumor growth and behavior.
The student will be able to recognize the common symptoms and signs of thoracic and extrathoracic lung cancer, and the common paraneoplastic syndromes associated with lung cancer.
The student will be able to summarize the general principles of lung cancer staging and describe how tumor stages affect treatment options and outcomes.
EPIDEMIOLOGY AND RISK FACTORS
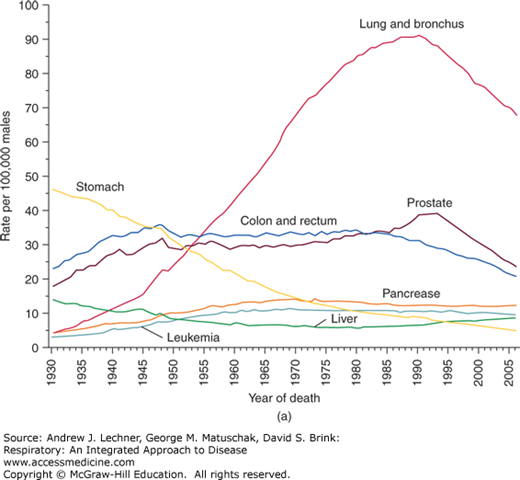
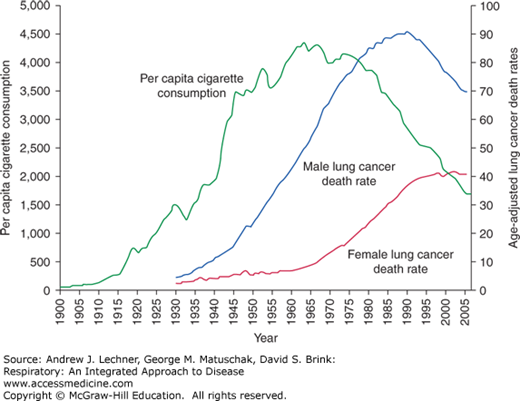
Lung cancer is the leading cause of cancer-related mortality in the United States. In 2009, over 200,000 new cases of lung cancer were diagnosed and, unfortunately, nearly 160,000 deaths occurred as a result of lung cancer (Fig. 32.1). In a sobering testament to its lethality, lung cancer accounts for only 15% of all cancers diagnosed (excluding non-melanomas of the skin), but accounts for 28% of those cancer deaths. Lung cancer has been the leading cause of cancer death in men in the United States since the mid-1950s, and in women since the late 1980s. This is especially striking given that lung cancer was a rare occurrence at the turn of the 20th century (Fig. 32.2).
The incidence of lung cancer increases steadily with age. Over a lifetime, 1 in 13 American men and 1 in 16 American women will be diagnosed with lung cancer. Thankfully, the lung cancer death rate has been declining in men and seems to have reached a plateau in women. African-American men are disproportionally affected compared to other races and ethnicities.
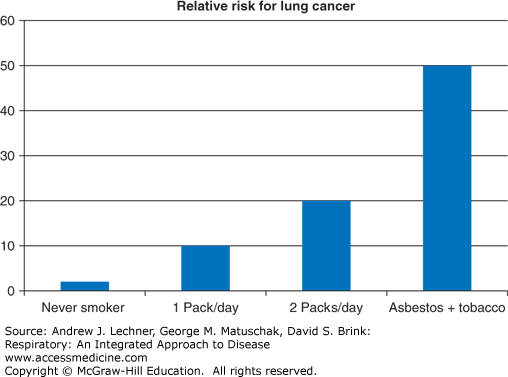
Exposure to tobacco smoke is by far the most substantial risk factor for development of lung cancer, and is at least partially avoidable. Approximately 80%-90% of all patients diagnosed with lung cancer are either current or former smokers. The association between tobacco smoke and lung cancer was postulated a century ago and clearly demonstrated by epidemiologic studies in the 1950s (Fig. 32.3). In the United States, the lifetime risk of lung cancer for a nonsmoker is <1% and increases to 15%-30% with long-term tobacco use. The risk of lung cancer increases with the amount and duration of tobacco exposure, and conversely the risk declines with abstinence. A decrease in risk can be demonstrated within 5 years of quitting smoking, and by 15 years there is an 80%-90% reduction in the risk of developing lung cancer, although that risk remains higher than for a never-smoker. Cigarettes seem to confer a higher risk of lung cancer than the use of pipes and cigars. Passive or “second-hand” exposure to tobacco smoke also increases the risk of lung cancer, but to a much lesser degree than active smoking. Never-smoking women married to husbands who smoke have up to a two-fold increase in the risk of lung cancer compared to never-smoking women with nonsmoking spouses.
Exposure to radon, a radioactive gas released by the decay of naturally occurring 238uranium, is the second leading cause of lung cancer in the United States and accounts for up to 10% of all lung cancer cases. Radon gas collects in poorly ventilated portions of some homes and buildings. Air pollution may account for 2% of lung cancer cases in the United States, but is a more significant factor worldwide, notably where biomass fuels are used for residential heating and cooking. Asbestos exposure alone modestly increases the risk of lung cancer, but when combined with tobacco use the risk increases dramatically by 50- to 60-fold (Fig. 32.4). Other risk factors for lung cancer include COPD, interstitial lung disease, and a family history of lung cancer. Finally, the risk of lung cancer is inversely proportional to intake of fruits and vegetables, although prospective trials involving such dietary supplementation have not shown a clear benefit.
PATHOGENESIS OF LUNG CANCERS
The pathogenesis of lung cancer involves a multistep process that is not completely understood. In most cases, lung cancer is initiated by adverse interactions between carcinogens and the respiratory epithelium that lead to genetic alterations. These alterations can be found in histologically normal tissue from smoker’s lungs. New DNA sequencing technologies have uncovered multiple and varied genetic abnormalities that reveal the heterogeneous nature of lung cancer even within a single cell type. Common genetic and molecular alterations include p53 tumor suppressor gene mutations, K-ras proto-oncogene mutations, and epidermal growth factor (EGF) and EGF receptor abnormalities. Genetic evidence of human papilloma virus (HPV) infection also suggests a role for viruses in lung cancer pathogenesis. The genetic and molecular characteristics of a cancer affect its promotion, progression, invasion, and metastasis. Although the heterogeneity of lung cancer might frustrate hopes of a single effective treatment, knowledge of the varied abnormalities allows for an individualized approach to treatment and prognostication. In some cases, certain genetic mutations suggest a likelihood of a dramatic response to very specific chemotherapeutic agents.
REVIEW OF LUNG CANCER HISTOPATHOLOGY
Classification of lung cancer by the World Health Organization in 2004 is based upon the appearance of the tumor cells by light microscopy (Table 32.1; see Chap. 31). Diagnostic immunohistochemical staining can corroborate and refine the classification based upon routine stains and light microscopy. In the aggregate, adenocarcinoma, squamous cell carcinoma, and small cell carcinoma account for ~85% of lung cancers.
| Squamous Cell Carcinoma | Variants: papillary, clear cell, small cell, basaloid |
| Small Cell Carcinoma | Variants: combined small cell carcinoma |
Adenocarcinoma
| Variants: mucinous, non-mucinous, mixed Variants: fetal, mucinous, mucinous cystadenocarcinoma, signet ring, clear cell |
| Large Cell Carcinoma | Variants: large cell neuroendocrine, combined, basiloid, lymphoepithelioma-like, clear cell, rhaboid |
| Adenosquamous Carcinoma | |
| Sarcomatoid Carcinoma | Variants: pleomorphic, spindle cell, giant cell, carcinosarcoma, pulmonary blastoma |
| Carcinoid Tumor | Variants: typical, atypical |
| Salivary Gland Tumors | Variants: mucoepidermoid, adenoid cystic, epithelial-myoepithelial |
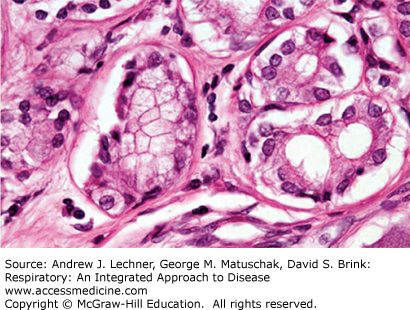
Adenocarcinoma is the most common histologic type of lung cancer accounting for up to 35% of all lung cancers, and this proportion seems to be increasing as compared to other cell types. It is more common in women and is the lung cancer type found in nearly all nonsmokers. Grossly, adenocarcinoma is irregularly lobulated, grey-white in color, and commonly shows entrapped anthracotic pigment. Histologically, adenocarcinomas are glandular in appearance and may show mucin in the cytoplasm (Fig. 32.5).
Clinically, adenocarcinomas tend to occur in the lung periphery (Fig. 32.6) either synchronously with more than one primary tumor at the same time, or metachronously with multiple primary tumors developing at different times. Bronchioloalveolar carcinoma is a subtype of adenocarcinoma requiring special attention as it can mimic pneumonia radiographically as a focal opacity or as more diffuse opacities. Histologically, bronchioloalveolar carcinoma is a well-differentiated tumor that grows along intact alveolar septa in a so-called lepidic pattern (Fig. 32.7).