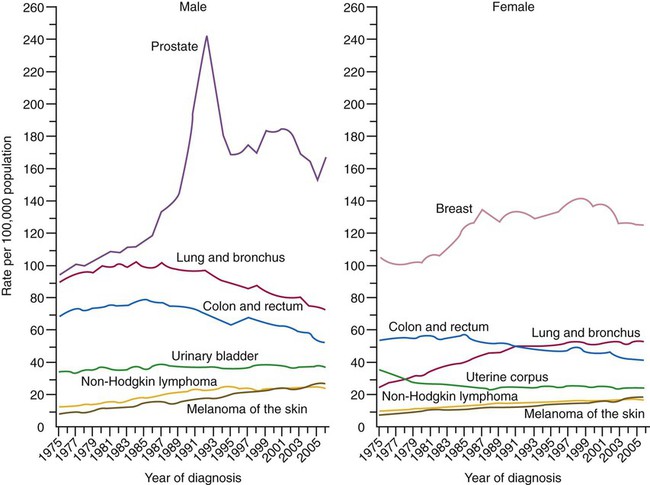
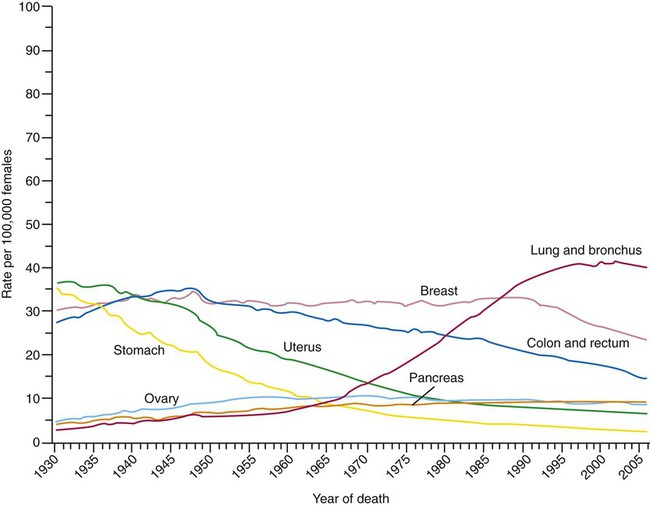
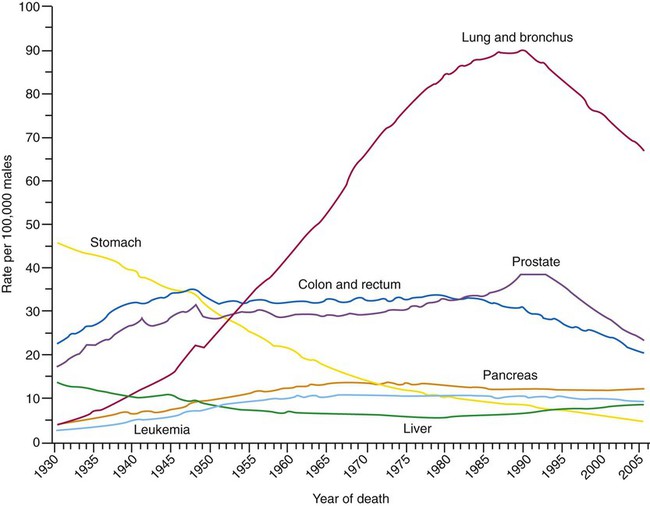
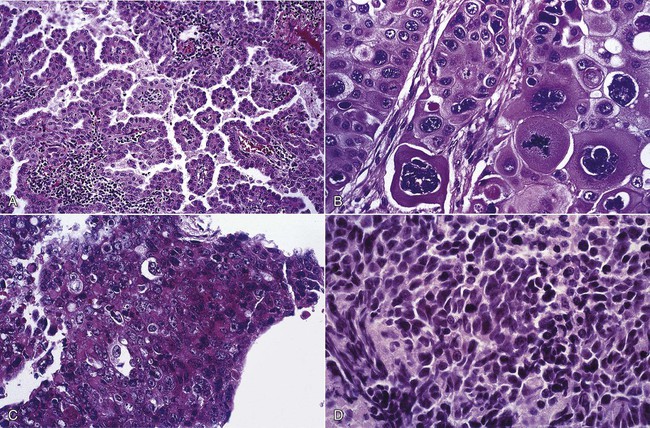
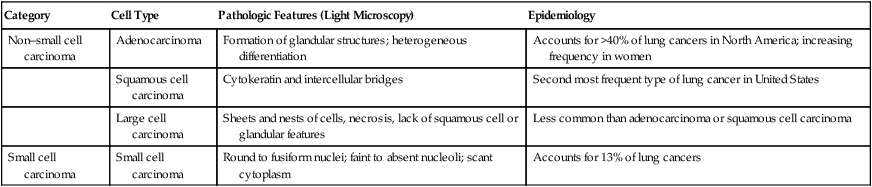
After reading this chapter you will be able to: Lung cancer is a major public health problem. In the United States, approximately 28% of cancer deaths are due to lung cancer.1 Most of these deaths could be avoided if people did not smoke tobacco-related products. Worldwide tobacco consumption has not been declining, however, suggesting lung cancer will remain an epidemic for years to come. Advances in early detection and treatment have been slow, leaving the overall prognosis very poor when lung cancer has been detected. Just over one in eight lung cancer patients is still living 5 years after diagnosis. This chapter provides an overview of lung cancer for the respiratory therapist (RT). In 2010, an estimated 222,520 new cases of lung cancer were diagnosed in the United States.1 Lung cancer is the second most frequently diagnosed cancer in men and women (prostate and breast cancers are most frequent in men and women) (Figure 28-1). The incidence of lung cancer peaked in men in 1984 (86.5 per 100,000 men) and has since been declining (69.1 per 100,000 in 1997). In women, the incidence increased during the 1990s, with a leveling off toward the end of the decade (43.1 per 100,000 women). These trends parallel the smoking patterns of men and women.1 The World Health Organization estimates that there are 2 million cases of lung cancer worldwide each year. Lung cancer is the leading cause of cancer-related mortality in men and women; it surpassed colon cancer in the early 1950s in men and breast cancer in the late 1980s in women. Mortality rates in men declined significantly in the 1990s, whereas a slow increase occurred in women. These rates parallel the smoking patterns of men and women (Figures 28-2 and 28-3). In 2010 in the United States, an estimated 157,300 deaths were due to lung cancer. In men, lung cancer is the leading cause of cancer-related mortality from age 40 on. In women, lung cancer surpasses breast cancer in the age group of 60 and older.1 There is evidence that nicotine, a chemical in tobacco, is highly addictive.2 Approximately one-fifth of all adults in the United States smoke cigarettes. Progress had been made in the fight against cigarette use; in the decades from 1970-1990, the percentage of women who smoked declined from 33% to 25%, and the rate of smoking among men decreased from 43% to 28%. The annual decline that had occurred since the early 1970s began to slow through the 1990s despite mounting evidence associating smoking with disease and death.3 In addition, a decrease in smoking has not been observed among adults 18 to 24 years old. Cigarette smoking among young people remains a major public health concern. Of young adults (18 to 24 years old), 33% have been reported to be current users of tobacco,4 and 3000 teenagers begin smoking each day.5 Approximately 13% of middle school children and 28% of high school students use tobacco products. In the context that a person who has not started smoking as a teenager is unlikely ever to become a smoker, the tobacco industry has focused on young people and developing countries as the primary sources of new customers.6,7 Other forms of exposure to tobacco-related products also pose risk of promoting lung cancer. Cigar smoking, which has increased considerably over the past several years, is known to be an independent risk factor for developing lung cancer.8 Exposure to sidestream smoke, or passive smoking, may also lead to an increased risk of lung cancer. The risk is generally much lower than active smoking but varies with the intensity of exposure.7 The risk of developing lung cancer has been reported to be 30% higher in individuals exposed to sidestream smoke. It has been estimated that 3000 to 5000 deaths in the United States and 21,400 deaths worldwide from lung cancer occur each year because of second-hand smoke exposure.9,10 Many other risk factors have been identified (Box 28-1). Occupational agents are known to act as lung cancer carcinogens. Arsenic, asbestos, and chromium confer the highest risk. Of lung cancers, 2% to 9% have been estimated to be related to occupational exposures. This risk is increased when there is concomitant exposure to tobacco products. Indoor radon exposure is also a risk factor for developing lung cancer.11 Radon is a product generated by the breakdown of uranium. Particulates in the atmosphere (i.e., pollution) can increase the risk of lung diseases including lung cancer. An inherited genetic predisposition has epidemiologic support as a risk factor, but the mechanisms are not proven. Family members of people who develop lung cancer have an increased risk.12,13 Women seem to have a higher baseline risk of developing lung cancer and a greater susceptibility to the effects of smoking. Differences in the metabolism of tobacco-related carcinogens and their metabolites, an effect of hormone differences, or both are thought to account for the increased susceptibility.14 Dietary factors can also modify risks. Higher consumption of fruits and vegetables is associated with a reduced lung cancer risk, and increased dietary fat intake may lead to a higher risk.15,16 Supplementation with vitamin A, vitamin E, or beta-carotene has not positively influenced risk.15 The presence of chronic obstructive pulmonary disease (COPD) is an independent risk factor.17 This risk increases as the forced expiratory volume in 1 second (FEV1) decreases.18,19 Lung cancers are divided into two major groups—small cell carcinoma and non–small cell carcinoma—based on pathologic features that are visible under light microscopy. The evaluation and management of a patient are guided by the category and stage (see later) of lung cancer. The non–small cell cancer category consists of adenocarcinoma, squamous cell carcinoma, large cell carcinoma, and variants (Figure 28-4). Table 28-1 presents the pathologic and epidemiologic features of the four most common types of lung cancer: adenocarcinoma, squamous cell carcinoma, large cell carcinoma, and small cell carcinoma. TABLE 28-1 Classification of Most Common Types of Lung Cancer The pathophysiology of lung cancer development is complex and incompletely understood. Damage to genetic material in lung cells is the result of exposure to chemical carcinogens such as the carcinogens contained in tobacco smoke.20 People who develop lung cancer may have a genetic predisposition to the effects of these carcinogens. The genes influenced in the pathogenesis of lung cancer produce proteins involved in cell growth and differentiation, cell cycle processes, apoptosis (programmed cell death), angiogenesis (production of new blood vessels), tumor progression, and immune regulation. If enough of these pathways have been affected, the uncontrolled growth of cells that defines cancer occurs. If the mechanisms that lead to genetic damage can be identified and the means by which the pathways involved are controlled, novel means of risk stratification, prevention, early detection, and therapy should be able to be developed. The clinical features of lung cancer result from the effects of local growth of the tumor, regional growth or spread through the lymphatic system, hematogenous (blood-borne) distant metastatic spread, and remote paraneoplastic effects from tumor products or immune cross reaction with tumor antigens (Box 28-2). Some manifestations occur more commonly with a particular cell type. Despite modern imaging advances, only approximately 15% of patients with a diagnosis of lung cancer do not have symptoms at the time of presentation. Some of the initial symptoms may be related to accompanying illnesses because these patients are at risk for other medical problems in addition to lung cancer (e.g., COPD, heart disease). When symptoms develop that are the result of the presence of cancer but are not related to the growth or spread of the cancer, these symptoms constitute a paraneoplastic syndrome. Paraneoplastic syndromes can result from the effects of proteins produced by the tumor that circulate through the body to have their effects on distant organs or result from the immune response of the body to a tumor antigen that is similar to antigens in other parts of the body, causing immune injury to the distant organ. Paraneoplastic syndromes may occur before the primary tumor appears and be the first sign of disease or an indication of tumor recurrence. Examples include production of excess glucocorticoids (ectopic Cushing syndrome), parathyroid hormone (hypercalcemia of malignancy), and antidiuretic hormone (syndrome of inappropriate antidiuretic hormone [SIADH]). Paraneoplastic neurologic syndromes can affect all parts of the neurologic system resulting in emotional lability (limbic encephalitis), loss of balance (cerebellar degeneration), and muscle weakness with a characteristic recruitment of strength on electrical stimulation (Lambert-Eaton syndrome). Other paraneoplastic syndromes include skeletal and connective tissue syndromes (clubbing, hypertrophic pulmonary osteoarthropathy), coagulation and hematologic disorders, cutaneous and renal manifestations, and systemic symptoms (anorexia, cachexia, and weight loss).21
Lung Cancer
 Describe the epidemiology of lung cancer in the United States, particularly current trends.
Describe the epidemiology of lung cancer in the United States, particularly current trends.
 Identify risk factors for lung cancer.
Identify risk factors for lung cancer.
 State the classification of lung cancer types and the cellular features of the four common types of lung cancer.
State the classification of lung cancer types and the cellular features of the four common types of lung cancer.
 Describe current understanding of the pathophysiology of lung cancer.
Describe current understanding of the pathophysiology of lung cancer.
 Identify the clinical features of the common types of lung cancer.
Identify the clinical features of the common types of lung cancer.
 Describe the diagnostic approach to lung cancer.
Describe the diagnostic approach to lung cancer.
 State the staging system for lung cancer.
State the staging system for lung cancer.
 Describe the treatment and outcomes for the common types of lung cancer by stage.
Describe the treatment and outcomes for the common types of lung cancer by stage.
 State the role of the respiratory therapist in managing patients with lung cancer.
State the role of the respiratory therapist in managing patients with lung cancer.
Epidemiology
New Cases
Deaths
Risk Factors
Tobacco-Related Products
Occupational Agents and Other Risks
Lung Cancer Classification
Category
Cell Type
Pathologic Features (Light Microscopy)
Epidemiology
Non–small cell carcinoma
Adenocarcinoma
Formation of glandular structures; heterogeneous differentiation
Accounts for >40% of lung cancers in North America; increasing frequency in women
Squamous cell carcinoma
Cytokeratin and intercellular bridges
Second most frequent type of lung cancer in United States
Large cell carcinoma
Sheets and nests of cells, necrosis, lack of squamous cell or glandular features
Less common than adenocarcinoma or squamous cell carcinoma
Small cell carcinoma
Small cell carcinoma
Round to fusiform nuclei; faint to absent nucleoli; scant cytoplasm
Accounts for 13% of lung cancers
Pathophysiology
Clinical Features
Lung Cancer