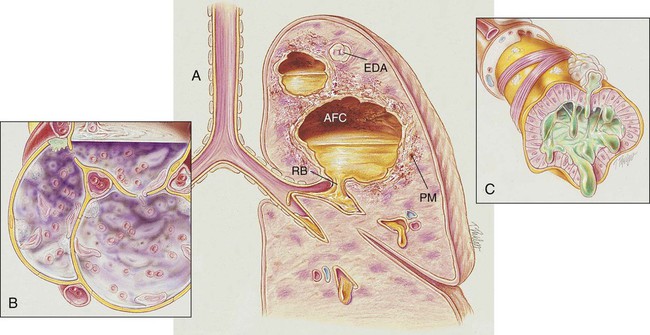
After reading this chapter, you will be able to: • List the anatomic alterations of the lungs associated with lung abscess. • Describe the causes of lung abscess. • List the cardiopulmonary clinical manifestations associated with lung abscess. • Describe the general management of lung abscess. • Describe the clinical strategies and rationales of the SOAPs presented in the case study. • Define key terms and complete self-assessment questions at the end of the chapter and on Evolve. During the early stages of a lung abscess, the pathology is indistinguishable from that of any acute pneumonia. Polymorphonuclear leukocytes and macrophages move into the infected area to engulf any invading organisms. This action causes the pulmonary capillaries to dilate, the interstitium to fill with fluid, and the alveolar epithelium to swell from the edema fluid. In response to this inflammatory reaction, the alveoli in the infected area become consolidated (see Figure 15-1). As the inflammatory process progresses, tissue necrosis involving all the lung structures occurs. In severe cases the tissue necrosis ruptures into a bronchus and allows a partial or total drainage of the liquefied contents into the cavity. An air- and fluid-filled cavity also may rupture into the intrapleural space via a bronchopleural fistula and cause pleural effusion and empyema (see Chapter 23, Pleural Diseases). This may lead to inflammation of the parietal pleura, chest pain, atelectasis, and decreased chest expansion. After a period of time, fibrosis and calcification of the tissues around the cavity encapsulate the abscess (see Figure 16-1). The major pathologic or structural changes associated with a lung abscess are as follows: A lung abscess is commonly associated with the aspiration of gastric and oral fluids. Aspiration can cause either (1) chemical pneumonia, (2) anaerobic bacterial pneumonia, or (3) a combination of both (see Chapter 15). The aspiration of acidic gastric fluids is associated with immediate injury to the tracheobronchial tree and lung parenchyma—often likened to a flash burn. Common anaerobic organisms found in the normal flora of the mouth, upper respiratory tract, and gastrointestinal tract include the following: Box 16-1 on p. 247 summarizes organisms known to cause lung abscess.
Lung Abscess
Anatomic Alterations of the Lungs
Etiology and Epidemiology