Superficial vein thrombophlebitis (SVT) is a common diagnosis associated with an inflammatory–thrombotic process of the superficial veins, most commonly involving the legs. SVT typically manifests with a warm, tender, palpable “cord” affecting the involved venous segment. The surrounding soft tissue can be similarly erythematous, with associated edema. Constitutional symptoms, including a low-grade fever and malaise, may be present. The incidence of SVT is thought to be underreported, and it likely surpasses that of deep vein thrombosis (DVT). There is a slight female predominance; only 35% to 46% of patients are male. The average age at time of presentation is 54 to 58 years.
Underlying venous varicosities exist in 62% of patients, and up to 70% of patients have associated superficial venous insufficiency. Additional risk factors for SVT include inherited thrombophilia, immobilization or trauma, postoperative states, pregnancy, active malignancy, chemotherapy infusions, autoimmune disease, oral contraceptive and hormone replacement therapy, advanced age, obesity, central venous catheterization, and history of previous venous thromboembolism (VTE). Factors specifically associated with symptomatic thromboembolic events, including recurrence or extension of SVT, include male sex, history of DVT or pulmonary embolism (PE), and malignancy.
Although SVT is traditionally viewed as a benign process, the associated complications include scar, DVT, PE, and death. The site of origin of thrombus in the superficial vein that is most likely to propagate into the deep venous system is the greater saphenous vein in 70% to 90% of patients, although up to 16% of patients with SVT of the small saphenous vein suffer from PE or DVT. In fact, a prospective epidemiologic study including 844 patients with symptomatic SVT revealed that approximately 25% had concomitant DVT upon enrollment. Of the 600 patients without DVT followed for 3 months, 58 (10.2%) developed thromboembolic complications, including pulmonary embolism in three (0.5%), DVT in 15 (2.8%), SVT extension in 18 (3.3%), and SVT recurrence in 10 (1.9%). These events occurred despite the use of anticoagulant treatment with low-molecular-weight heparin (LMWH) at therapeutic dosing (374 patients, 62.9%) and prophylactic dosing (216 patients, 36.7%) for 10 to 17 days. These findings were consistent with previously published data regarding the prevalence of venous thromboembolism (6%–53%) and pulmonary embolism (0%–10%) in this patient population.
Diagnostic workup for first-time venous thrombosis necessitates lower extremity venous duplex to confirm the diagnosis, distribution, and extent of the thrombosis and to interrogate the deep venous system. Venous insufficiency can be identified in this manner as well. Venography is not recommended. Patients with recurrent SVT should be further assessed for a hypercoagulable disorder and malignancy. Treatment options in the literature range from conservative medical management that includes nonsteroidal antiinflammatory agents (NSAIDs), to anticoagulation and surgical vein ligation and/or phlebectomy.
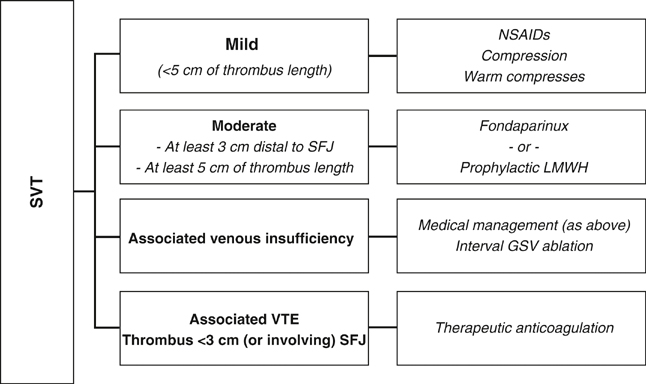
Treatment options for SVT should be individualized based on thrombus extent and location, the presence or absence of concomitant DVT, and any associated infectious process (Figure 1). A 2010 Cochrane review included 24 trials involving 2469 patients with SVT of the lower extremities. None of the studies evaluated the same treatment comparisons on the same study outcomes, limiting analysis. Traditionally, treatment for SVT in tributaries and the distal greater saphenous vein (GSV) include ambulation, warm soaks, elastic compression, and NSAIDs to alleviate the inflammatory reaction, which averages 7 to 21 days. NSAIDs have been shown to significantly reduce the risk of SVT extension and/or recurrence by 67% compared to placebo, but they offer no protection against the incidence of venous thromboembolism or resolution of local signs and/or symptoms.
Interestingly, topical agents (including heparin spray-gel) have been shown to reduce local signs and symptoms. The 2008 American College of Chest Physician guidelines suggest oral diclofenac or another NSAID (Grade 2B), topical diclofenac gel (Grade 2B), or heparin gel (Grade 2B) for patients with symptomatic infusion thrombophlebitis as a complication of IV infusion for up to 2 weeks, and they recommend against anticoagulation in this cohort of patients.
If a thrombus extends toward the level of the saphenofemoral junction (SFJ), or if a patient with SVT carries additional risk factors for DVT extension, more aggressive treatment options have been employed including surgical ligation or stripping and anticoagulation. Historically, thrombus within 3 cm of the SFJ was thought to warrant surgical ligation of the SFJ with or without simultaneous GSV stripping or ligation. Current data tends to support medical management with anticoagulation and elastic compression over surgical measures.
A 1999 prospective trial assessed 562 patients presenting with acute SVT. Thirty-eight patients (6.7%) were excluded secondary to the presence of concomitant DVT because they received appropriate therapeutic anticoagulation. An additional 15 patients (3.6%) with hypercoagulable disorders were excluded. The remaining 509 patients were allocated to six different treatment arms; SVT extension and development of DVT were assessed with duplex imaging at 3- and 6-month intervals. The incidence of SVT extension was higher in the control group (elastic compression only) and the saphenous ligation group when compared to the anticoagulant treatment groups, who received prophylactic unfractionated heparin, prophylactic LMWH, and therapeutic anticoagulation with warfarin. There was no statistically significant difference in DVT formation between treatment groups; however, a trend favored patients receiving anticoagulation. These authors did note that stripping of the affected veins was associated with the lowest incidence of thrombus extension. There were no major side effects noted in any arm, including bleeding, heparin-induced thrombocytopenia (HIT), or postsurgical complications.
A 2003 prospective randomized trial compared saphenofemoral disconnection to therapeutic anticoagulation for treating proximal GSV thrombophlebitis. Eighty-four consecutive patients with proximal thrombophlebitis alone were divided into two groups and treated with either saphenofemoral disconnection under local anesthesia (n = 45) or enoxaparin (1 mg/kg bid) on an outpatient basis for 4 weeks (n = 39). Thirty patients in each group completed the study, and follow-up occurred at 1, 3, and 6 months. In the surgical group, two patients (6.7%) had surgical wound complications, one patient (3.3%) developed recurrent thrombophlebitis, and two patients developed (6.7%) a nonfatal PE over 6 months. In the medical group there was no progression of the thrombosis to the deep venous system or PE, but two cases (6.7%) of minor bleeding and three cases (10%) of recurrent thrombophlebitis were reported. Even though the study found no statistically significant difference between the two groups, the LMWH group conferred a significant socioeconomic advantage and confirmed the efficacy of LMWH treatment.
A 2003 double-blind randomized trial randomly assigned 427 patients with documented acute symptomatic SVT to prophylactic enoxaparin 40 mg daily, therapeutic enoxaparin 1.5 mg/kg daily, oral tenoxicam, or placebo for 8 to 12 days. The incidence of deep and superficial venous thromboembolism by day 12 was significantly decreased in all treatment groups, from 30.6% in the placebo group to 8.3% in the prophylactic enoxaparin group, 6.9% in the therapeutic enoxaparin group, and 14.9% in the tenoxicam group. There were no episodes of major bleeding or HIT in any treatment group.
A 2010 international multicenter randomized, double-blind, placebo-controlled trial assessed the safety and efficacy of fondaparinux for SVT. The trial studied 3002 patients with acute symptomatic lower limb SVT involving a segment at least 5 cm in length located at least 3 cm distal to the saphenofemoral junction. Subjects were treated with either fondaparinux 2.5 mg subcutaneously daily or placebo for 45 days; patients were followed until day 77. Patients receiving fondaparinux demonstrated an 85% lower rate of PE or DVT than the placebo group and a significantly reduced rate of symptomatic SVT recurrence or SVT extension to the saphenofemoral junction without major bleeding or serious adverse event.
For patients with symptomatic SVT and evidence of venous insufficiency or reflux confirmed by duplex study, surgery remains the optimal treatment. Historically, saphenofemoral ligation with GSV stripping and/or phlebectomies were advocated, but GSV ablation (either radiofrequency ablation or laser ablation) has all but replaced saphenofemoral ligation and GSV stripping. In our practice, this surgical approach is staged on the order of weeks to allow for a decrease or resolution in the acute inflammation. These patients are managed medically until the time of surgery and receive treatment with 1 week of prophylactic LMWH postoperatively.
The 2008 American College of Chest Physicians guidelines suggest prophylactic or intermediate doses of LMWH (Grade 2B) or intermediate doses of heparin (Grade 2B) for patients with spontaneous SVT for a treatment course of at least 4 weeks. Alternatively, oral vitamin K antagonists (with a goal international normalized ratio [INR] of 2–3) overlapped with 5 days of heparin or LMWH for a treatment course of at least 4 weeks is given a Grade 2C recommendation. Concomitant used of NSAIDs is not advised (Grade 2B), and medical treatment is advocated over surgical treatment (Grade IB). Certainly any patient who develops concomitant or subsequent venous thromboembolism warrants appropriate therapeutic anticoagulation. One should consider a 45-day course of daily fondaparinux, 2.5 mg subcutaneously, for less-extensive, symptomatic SVT at least 5 cm in length and located at least 3 cm distal to the saphenofemoral junction.
SVT that manifests with an associated infection deserves special attention. It is almost exclusively coupled with intravenous catheterization. Local manifestations may be subtle or even absent, yet dramatic systemic sequelae (septic shock and multisystem organ failure) can result along the spectrum of nonsuppurative to suppurative septic thrombophlebitis. The incidence of septic thrombophlebitis increases when dwelling peripheral venous catheters remain in place for more than 2 to 3 days. Many advocate catheter replacement at intervals of 72 to 96 hours. Normal skin flora can simply migrate along the catheter to the vascular space; additional infectious sources include contaminated intravenous fluids or hematogenous spread from distant sources. Specifically, postsurgical patients can come to the hospital with septic thrombophlebitis secondary to infectious complications at the site of the surgical wound.
Historical treatment approaches remain relevant and include removing the offending catheter, applying warm compresses, and administering NSAIDs and broad-spectrum intravenous antibiotics, which can be tailored to the appropriate bacterial culprit and antibiotic sensitivities pending the return of quantitative and qualitative culture results. Surgery should be reserved for patients who fail conservative medical management and require true source control for ongoing sepsis. Surgical exploration with drainage of any identified abscess and full venous resection to the extent that brisk backbleeding is encountered remains prudent today.