The Killip classification of acute heart failure was developed decades ago to predict short-term mortality in patients with acute myocardial infarction (AMI). The aim of this study was to determine the long-term prognosis of acute heart failure graded according to the Killip classification in 15,235 unselected patients hospitalized for AMI from 2000 to 2005. Vital status for each patient was ascertained, through to March 1, 2012, from linkage with national death records. A stepwise gradient in the adjusted hazard ratio (HR) for 12-year mortality was observed with increasing Killip class: class I (n = 10,123), HR 1.00 (reference group); class II (n = 2,913), HR 1.13 (95% confidence interval [CI] 1.06 to 1.21); class III (n = 1,217) HR 1.49 (95% CI 1.37 to 1.62); and class IV (n = 898), HR 2.80 (95% CI 2.53 to 3.10). Unexpectedly, in a landmark analysis excluding deaths <30 days after admission, patients in Killip class IV had lower adjusted long-term mortality than those in class III. The adjusted HR for 12-year mortality comparing Killip class IV with Killip class III in patients <60 years of age was 1.71 (95% CI 1.33 to 2.19, p <0.001) and in patients >60 years of age was 2.30 (95% CI 2.07 to 2.56, p <0.001). In conclusion, on the basis of simple clinical features, the Killip classification robustly predicted 12-year mortality after AMI. The heterogeneity in early versus late risk in patients with Killip class IV heart failure underscores the importance of appropriate early treatment in cardiogenic shock.
The Killip classification was first published in 1967 and was based on the prognostic evaluation of 250 patients admitted to an intensive care unit with acute myocardial infarction (AMI). The classification was developed for simple early risk stratification using only routine physical examination parameters and clinical sense, hence explaining its simplicity, popularity, and longevity. However, the relevance of the original small historical study to contemporary practice has been questioned. The original population studied had an exceedingly high in-hospital mortality rate (27%) and a high incidence of cardiogenic shock (19%) that is inconsistent with current outcomes of patients with AMI. The predictive accuracy of the Killip classification for coronary patency after reperfusion, in-hospital mortality, and 6-month outcomes has been ascertained in large cohort-based studies. Apart from being unable to assess the prognostic value of the Killip classification beyond a 6-month time frame, these studies had limited numbers of patients in Killip class IV, so they were unable to directly compare outcomes of patients in Killip class IV with outcomes of patients in other Killip classes. We therefore investigated the prognostic accuracy of the Killip classification in predicting outcomes out to 12 years after the index AMI. In view of published research suggesting risk heterogeneity in patients with cardiogenic shock (Killip class IV heart failure), we further profiled the subgroup of patients in Killip class IV surviving beyond 30 days.
Methods
We analyzed 15,235 patients hospitalized for AMI under the publicly funded health care system in Singapore from January 2000 to December 2005, with follow-up of vital status through to February 2012. As per health care legislation in Singapore, patients hospitalized for AMI at all 6 public hospitals are captured in the Singapore Myocardial Infarction Registry (SMIR) without the need for written informed consent. We excluded patients <21 years of age, nonresidents of Singapore, and those who died <24 hours after admission. The public health care system in Singapore provides universal health care access to all Singapore citizens and permanent residents through 3 interdependent government-led financing programs, Medisave, Medishield, and Medifund, thereby minimizing treatment disparities. Because >96.0% of patients with AMI in Singapore receive their initial care at public hospitals, the SMIR captures data on most AMI cases in Singapore.
The methods of the SMIR have been previously described. Briefly, trained staff members at the SMIR perform all data collection, site monitoring, and case adjudication. AMI cases are adjudicated using admission and discharge criteria in agreement with International Classification of Diseases, Ninth Revision, codes 410.00 to 414.19 or postmortem reports. Electrocardiograms are interpreted centrally at the Singapore Cardiac Databank and noted to record ST-segment elevation or ST-segment depression of ≥1 mm in 2 contiguous anterior, inferior, posterior, or lateral leads, Q waves 1/3 the height of the R wave or >0.04 seconds, or left bundle branch block. All clinical chemistry laboratories in Singapore submit a quarterly listing of patients with elevated cardiac troponin, creatine phosphokinase-MB, and creatinine phosphokinase results to SMIR. The attending physician in the emergency department ascertained the presence of heart failure in accordance with prespecified Killip class criteria ( Figure 1 ).
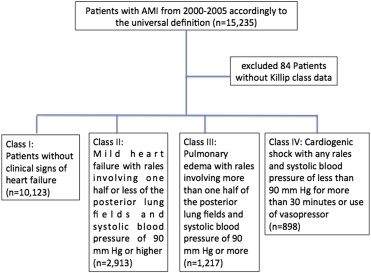
With the introduction of the universal definition of myocardial infarction in 2000, we reviewed the troponin and creatine kinase-MB results of all patients in our study population. A total of 87.31% of patients had troponin or creatine kinase-MB levels above the 99th percentile of each hospital laboratory’s reference population, and diagnoses of AMI were made in these patients if there was accompanying ischemia. The remaining 12.29% did not have sufficient cardiac biomarker data for diagnosis on the basis of the universal definition. These patients were diagnosed based on the original World Health Organization Monitoring Trends and Determinants of Cardiovascular Disease (WHO-MONICA) criteria. Sensitivity analyses in which we removed the 12.29% of cases did not change the directionality of our results. A total of 84 patients without Killip class data were excluded from the present analysis. Complete information was available for 89.8% of data elements recorded at the end of the study period.
Vital status after discharge was evaluated subsequently through record linkage with the National Registry of Births and Deaths to determine all-cause and cause-specific mortality, as previously described. It is a statutory requirement that death must be registered <24 hours after its occurrence in Singapore. The primary outcome analyzed was all-cause mortality from the time of hospital admission to the date of death or, for those alive, censored at March 1, 2012.
The study was conducted according to the Declaration of Helsinki, and the institutional review boards of all 6 publicly funded hospitals in Singapore approved the data collection and analysis.
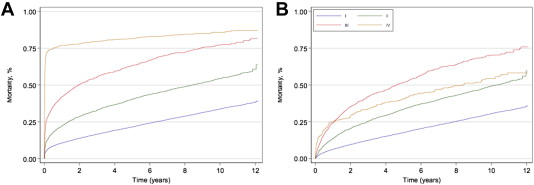
Baseline values, clinical characteristics, and mortality data are presented as percentages or means. Comparisons among Killip classes were made with Pearson’s chi-square test for categorical data and the Kruskal-Wallis test for continuous data. Kaplan-Meier mortality curves were constructed using the product-limit estimator to analyze all-cause death from the time of hospital admission till the end of the follow-up period. A 30-day landmark mortality analysis was also performed for subjects surviving beyond 30 days of admission for the index myocardial infarction.
The hazard ratio summarizing the differences among Killip Classes, and the corresponding 95% confidence interval, was estimated by Cox regression. On the basis of a literature review and clinical intuition, we selected potential confounders that were considered for inclusion in the multivariate analysis: age, gender, other co-morbidities such as diabetes mellitus and hypertension, reperfusion therapy, and in-hospital treatment. We further conducted stratified Cox regression analysis using age, gender, ethnicity, intra-aortic balloon pump (IABP) insertion, and performance of percutaneous coronary intervention (PCI) during the index hospitalization. Stata version 11.1 (StataCorp LP, College Station, Texas) was used for all analyses, and statistical significance was set at a 2-sided α value of 0.05.
Results
Among 15,151 patients hospitalized for AMI, 5,028 (33.2%) developed acute heart failure. During the index hospitalization, 10,123 patients (66.8%) remained in Killip class I (no heart failure), 2,913 patients (19.2%) developed Killip class II heart failure, 1,217 patients (8.0%) developed Killip class III heart failure, and 898 patients (5.9%) developed Killip class IV heart failure. There were progressive increases in age and the frequency of women with each increase in Killip class ( Table 1 ). Patients in Killip class I had the highest prevalence of a family history of coronary heart disease and current smoking. Otherwise, other co-morbidities, such as diabetes, hypertension, previous AMI, previous stroke, and peripheral artery disease, were most commonly observed in patients in Killip class III, even more so than in those in Killip class IV.
| Variable | Killip Classification | P-Value | |||
|---|---|---|---|---|---|
| I (N=10,123) | II (N=2,913) | III (N=1,217) | IV (N=898) | ||
| Mean age (Years) | 60.4 | 65.9 | 69.4 | 69.0 | <0.001 |
| Women | 23.3 (%) | 34.3 (%) | 38.9 (%) | 40.3 (%) | <0.001 |
| Diabetes Mellitus | 33.9 (%) | 44.1 (%) | 55.7 (%) | 45.0 (%) | <0.001 |
| Hypertension | 56.2 (%) | 61.6 (%) | 70.0 (%) | 61.7 (%) | <0.001 |
| Smoker | 56.2 (%) | 52.5 (%) | 43.2 (%) | 44.5 (%) | <0.001 |
| Chronic Renal Failure | 4.5 (%) | 7.3 (%) | 14.5 (%) | 11.4 (%) | <0.001 |
| Family History of premature coronary heart disease | 15.4 (%) | 9.8 (%) | 6.4 (%) | 6.6 (%) | <0.001 |
| Previous Myocardial Infarction | 9.6 (%) | 13.0 (%) | 17.4 (%) | 15.0 (%) | <0.001 |
| Previous cerebrovascular disease | 7.2 (%) | 10.7 (%) | 17.5 (%) | 15.7 (%) | <0.001 |
| Previous Peripheral vascular disease | 1.7 (%) | 3.4 (%) | 6.0 (%) | 3.6 (%) | <0.001 |
| Previous Percutaneous Coronary Intervention | 4.8 (%) | 4.1 (%) | 4.6 (%) | 3.9 (%) | 0.280 |
| Previous Coronary Artery bypass grafting | 2.7 (%) | 3.1 (%) | 3.3 (%) | 2.8 (%) | 0.479 |
| Clinical Presentation: | |||||
| NSTEMI | 51.8 (%) | 54.9 (%) | 60.5 (%) | 53.7 (%) | <0.001 |
| STEMI | 48.2 (%) | 45.1 (%) | 39.5 (%) | 46.3 (%) | <0.001 |
| ECG classification of STEMI patients only: | |||||
| Isolated Anterior STEMI | 27.3 (%) | 32.0 (%) | 27.9 (%) | 38.9 (%) | <0.001 |
| Isolated Inferior STEMI | 32.2 (%) | 25.1 (%) | 16.5 (%) | 28.4 (%) | <0.001 |
| Other ECG morphology ∗ | 40.5 (%) | 42.9 (%) | 55.6 (%) | 33.0 (%) | <0.001 |
| Aspirin | 89.8 (%) | 86.7 (%) | 79.4 (%) | 71.6 (%) | <0.001 |
| In-Hospital Treatment: | |||||
| Thienopyridine | 59.4 (%) | 43.1 (%) | 36.0 (%) | 28.8 (%) | <0.001 |
| β-Blockers | 79.4 (%) | 65.0 (%) | 47.3 (%) | 37.0 (%) | <0.001 |
| Angiotensin-Converting-Enzyme Inhibitors | 61.9 (%) | 70.1 (%) | 64.2 (%) | 38.0 (%) | <0.001 |
| Glycoprotein IIb/IIIa Inhibitors | 6.9 (%) | 7.1 (%) | 6.8 (%) | 6.4 (%) | 0.905 |
| Lipid Lowering Therapy | 79.2 (%) | 71.1 (%) | 61.7 (%) | 39.9 (%) | <0.001 |
| Digoxin | 3.9 (%) | 11.5 (%) | 21.2 (%) | 14.6 (%) | <0.001 |
| Inotropes | 8.3 (%) | 16.6 (%) | 32.2 (%) | 68.3 (%) | <0.001 |
| Intra-Aortic Balloon Pump | 1.7 (%) | 3.9 (%) | 8.0 (%) | 22.1 (%) | <0.001 |
| Temporary Pacing | 1.7 (%) | 3.5 (%) | 3.9 (%) | 10.2 (%) | <0.001 |
| Permanent Pacemaker Implantation | 0.3 (%) | 0.9 (%) | 2.7 (%) | 8.0 (%) | <0.001 |
| Treatment with Fibrinolytics | 20.4 (%) | 22.3 (%) | 12.5 (%) | 17.0 (%) | <0.001 |
| Primary and Salvage PCI or Emergency | 42.0 (%) | 33.6 (%) | 21.1 (%) | 27.2 (%) | <0.001 |
| Elective Percutaneous Coronary Intervention | 13.3 (%) | 5.7 (%) | 3.0 (%) | 1.7 (%) | <0.001 |
| Coronary Bypass | 1.9 (%) | 2.7 (%) | 3.4 (%) | 5.5 (%) | <0.001 |
∗ New onset LBBB, combined anterior and inferior STEMI, isolated lateral or posterior wall STEMI (%).
ST-segment elevation myocardial infarction (STEMI) was less commonly observed than non-STEMI (NSTEMI) among all Killip classes. Among patients with STEMI, patients in Killip class I had the highest frequency of inferior STEMI, whereas those in Killip class IV had the highest frequency of anterior STEMI ( Table 2 ).
| Variable | Killip Classification | P-Value | |||
|---|---|---|---|---|---|
| I (N=10,123) | II (N=2,913) | III (N=1,217) | IV (N=898) | ||
| Ventricular Septal Rupture | 0.4 (%) | 0.3 (%) | 0.1 (%) | 1.2 (%) | <0.001 |
| Mitral Regurgitation | 29.9 (%) | 14.6 (%) | 10.0 (%) | 7.7 (%) | <0.001 |
| Cardiac Rupture | 0.7 (%) | 0.4 (%) | 0.1 (%) | 1.0 (%) | <0.001 |
| Supraventricular | 33.7(%) | 49.0 (%) | 59.4 (%) | 47.0 (%) | <0.001 |
| Ventricular | 44.8 (%) | 43.9 (%) | 40.7 (%) | 63.6 (%) | <0.001 |
| Mobitz Type II | 1.8 (%) | 1.9 (%) | 4.5 (%) | 2.1 (%) | 0.167 |
| Complete Heart Block | 15.1 (%) | 19.0 (%) | 24.7 (%) | 30.5 (%) | <0.001 |
| Sepsis | 17.6 (%) | 28.6 (%) | 35.3 (%) | 37.2 (%) | <0.001 |
| Anoxic Brain Damage | 1.1 (%) | 1.4 (%) | 2.4 (%) | 9.4 (%) | <0.001 |
| Acute Renal Failure | 2.2 (%) | 4.3 (%) | 9.2 (%) | 17.7 (%) | <0.001 |
| Mortality | NSTEMI /STEMI | NSTEMI /STEMI | NSTEMI /STEMI | NSTEMI/STEMI | |
|---|---|---|---|---|---|
| 30 days Mortality | 5.8/4.0 (%) | 11.9/9.2 (%) | 25.3/22.4 (%) | 72.2/65.7 (%) | <0.001 |
| 1-Year Mortality | 12.7/8.4 (%) | 26.3/16.8 (%) | 44.6/37.9 (%) | 82.1/70.4 (%) | <0.001 |
| 12-Years Mortality | 43.3/32.8 (%) | 65.3/55.0 (%) | 84.2/78.5 (%) | 91.9/81.1 (%) | <0.001 |
| Unadjusted 12-Year Mortality HR (95% CI) | 1.0 (reference group) | 1.95 (1.84 to 2.08) | 3.80 (3.53 to 4.08) | 7.92 (7.31 to 8.58) | <0.001 |
| ∗ Adjusted 12-Year Mortality HR (95% CI) | 1.0 (reference group) | 1.13 (1.06, 1.21) | 1.49 (1.37, 1.62) | 2.80 (2.53, 3.10) | <0.001 |
∗ All comorbidities and in-hospital treatment variables were included in the multivariate model.
Patients in Killip class IV were more susceptible to ventricular arrhythmias and mechanical complications, including ventricular septal rupture and cardiac free wall rupture. Patients in Killip class IV were also more likely to undergo cardiopulmonary resuscitation and had more anoxic brain injury and sepsis compared with patients in other Killip classes ( Table 2 ).
Guideline-recommended medications were less prescribed with each progressive increase in Killip class, including angiotensin-converting enzyme inhibitors or angiotensin receptor blockers, β blockers, antiplatelet agents and anticoagulant drugs ( Table 1 ). In contrast, there were progressive increases in digoxin use, inotropic support, IABP implantation, temporary transvenous pacing, and permanent pacemaker implantation with each increase in Killip class. Expectedly, in-hospital revascularization was performed less frequently in patients in Killip classes III and IV compared with those in Killip classes I and II. Curiously, in comparing revascularization use between Killip class III and IV patients, those in Killip class IV were more likely to undergo in-hospital revascularization than those in Killip class III.
The mean follow-up duration was 7.3 years (maximum 12 years) among all Killip classes. There was a stepwise increase in 12-year mortality with each increase in Killip class in uni- and multivariate analyses ( Table 2 ). In the unadjusted analysis, patients in Killip class IV were at an eightfold greater risk for 12-year mortality compared with those in Killip class I. Among patients in Killip class IV, mortality was very high during the first 30 days of follow-up ( Figure 2 ). However, patients in Killip class IV who survived beyond 30 days had a cumulative late mortality rate (55.0%) that was lower than that of patients in Killip class III who survived beyond 30 days (68.6%), as shown in the 30-day landmark analysis ( Figure 2 ).