Myocardial perfusion single-photon emission computed tomography is a routine technique for the evaluation of coronary artery disease. However, information on the very long term prognostic value of dobutamine stress single-photon emission computed tomographic myocardial perfusion imaging (MPI) in patients with limited exercise capacity is scarce. The aim of this study was to assess the long-term prognostic value of dobutamine stress technetium-99m ( 99m Tc)–sestamibi MPI in these patients. The study population consisted of a high-risk cohort of 531 consecutive patients with limited exercise capacity who underwent dobutamine stress 99m Tc-sestamibi MPI for the assessment of known or suspected coronary artery disease. Follow-up was successful in 528 patients. Because of early revascularization, 55 patients were excluded. The present data are based on 473 patients. The end points were all-cause mortality, cardiac death, nonfatal myocardial infarction, and late (>60 days) coronary revascularization. Kaplan-Meier survival curves were performed and univariate and multivariate analyses were performed to identify predictors of very long term outcome. The mean age of the patients was 61 ± 12 years, and 58% were men. Abnormal results (defined as the presence of reversible or fixed defects) were observed in 312 patients (66%). During a mean follow-up period of 11.3 ± 6.7 years, 287 patients (61%) died (all-cause mortality), of whom 125 (26%) died due to cardiac causes. Nonfatal myocardial infarction occurred in 59 patients (12%). Late coronary revascularization was performed in 61 patients (13%). Univariate predictors of major cardiac events included age, male gender, previous infarction, diabetes mellitus, history of angina, heart failure, ST-segment changes, abnormal results on 99m Tc-sestamibi scan, reversible defect, fixed defect, summed rest score, and summed stress score. Multivariate analysis identified abnormal results on MPI as a strong independent predictor of major adverse cardiac events. In conclusion, in patients with limited exercise capacity, dobutamine stress 99m Tc-sestamibi single-photon emission computed tomography provides incremental prognostic information in addition to clinical and stress test parameters for the prediction of very long term outcomes.
Globally, coronary artery disease (CAD) remains a major cause of morbidity and mortality. Myocardial perfusion imaging with single-photon emission computed tomography (SPECT) is a routine technique for the diagnosis and risk stratification of patients with known or suspected CAD. Technetium-99m ( 99m Tc)–sestamibi is a widely used tracer in conjunction with SPECT. In patients with limited exercise capacity because of disease complications such as stroke, neuropathy, or peripheral vascular disease, dobutamine stress testing represents an achievable alternative to vasodilator stress. The prognostic value of dobutamine stress 99m Tc-sestamibi myocardial perfusion imaging (MPI) for detecting CAD has been well documented in various patient groups for short- and medium-term follow-up. However, very long term prognostic data on dobutamine stress 99m Tc-sestamibi MPI are lacking. Accordingly, the aim of this study was to determine the long-term prognostic value of dobutamine stress 99m Tc-sestamibi MPI for the prediction of adverse events in a high-risk cohort of patients with limited exercise capacity.
Methods
The study population consisted of a high-risk cohort of 531 consecutive patients with limited exercise capacity, as previously described. These patients were referred from 1990 to 1995 for dobutamine stress 99m Tc-sestamibi SPECT for the evaluation of suspected or known CAD. Follow-up was successful in 528 of 531 patients (99.4%). All patients gave informed consent before testing, and the local ethics committee approved the study protocol. Fifty-five patients underwent early coronary revascularization 60 days after MPI and were excluded from analysis (35 with coronary arterial bypass graft placement and 20 with percutaneous transluminal coronary angioplasty). This exclusion was based on previously published data indicating that referral to coronary revascularization in the first 60 days after nuclear testing tends to be based on the results of the scan and that referral to revascularization >60 days after nuclear testing tends to be based on the worsening of the patient’s clinical status. In September 2012, follow-up was performed. As a result, the present data are based on 473 patients with complete follow-up. A structured interview and clinical history were obtained, including assessment of cardiac risk factors, before dobutamine stress testing. Blood pressure ≥140/90 mm Hg or treatment with antihypertensive medication was considered as hypertension. A fasting glucose level ≥7.8 mmol/L or the need for insulin or oral hypoglycemic agents was considered as diabetes mellitus. Hypercholesterolemia was defined as a total cholesterol level ≥6.4 mmol/L or treatment with lipid-lowering medication.
The stress-testing protocol after dobutamine administration has been described previously. Dobutamine was injected intravenously up to a maximum dose of 40 μg/kg/min. If the test end point was not reached at a maximum dose of dobutamine, up to 1 mg of atropine was administered intravenously. During stress testing, blood pressure, heart rate, and electrocardiographic leads were continuously monitored. Test end points were achievement of target heart rate (85% of maximum age- and gender-predicted heart rate); horizontal or downsloping ST-segment depression of >2 mm at an interval of 80 ms after the J point, compared with the baseline measurement; ST-segment elevation >1 mm in patients without previous myocardial infarction; severe angina; systolic blood pressure decrease >40 mm Hg, compared with the baseline measurement; blood pressure >240/120 mm Hg; or clinically important cardiac arrhythmias. To overcome the side effects of dobutamine, metoprolol was intravenously administered, and atropine was used if the effects did not revert spontaneously after the termination of dobutamine infusion.
A dose of 370 MBq of 99m Tc-sestamibi (Cardiolite; Bristol-Myers Squibb Pharma Belgium, Brussels, Belgium) was administered intravenously approximately 1 minute before the cessation of the stress test. For studies performed with the patient at rest, 370 MBq of sestamibi was injected ≥24 hours after stress testing. Images were acquired with a Gammasonics single-head Rota camera (Orbiter; Siemens, Iselin, New Jersey) without attenuation or scatter correction, by using a low-energy all-purpose collimator. Thirty-two projections were obtained over a 180° arc, from left posterior oblique to right anterior oblique, with an acquisition time of 45 seconds per projection. Data were collected in a 64 × 64 matrix (word mode), and images were reconstructed by using a filtered back-projection algorithm and a ramp reconstruction filter. Transverse images were reconstructed by using a software package (SPETS; Nuclear Diagnostics, Hägersten, Sweden). From the 3-dimensional data, oblique (short-axis) and sagittal (vertical long-axis) images obtained perpendicular and parallel to the long axis, respectively, were reconstructed. The scan interpretation were semiquantitatively performed by using visual analysis assisted by circumferential profile analysis. Profile curves 2.5 SDs below normal perfusion were considered abnormal. Images obtained at stress and rest were reviewed side by side at a computer display with consensus reading by 2 experienced observers who were blinded to the patients’ clinical data. A third observer was consulted in case of disagreement of a decision. In this study, the original interpretations of the images were used. A reversible perfusion defect was defined as a perfusion defect on stress images that partially or completely resolved at rest on ≥2 contiguous segments or sections. A fixed perfusion defect was defined as a perfusion defect on stress images on ≥2 contiguous segments or sections that persist on rest images. The presence of a fixed and/or reversible perfusion defect was considered an abnormal result. Each myocardial segment was assigned a score from 0 to 3 (0 = normal, 1 = slightly reduced, 2 = moderately reduced, 3 = severely induced or absent uptake). Summed stress score and summed rest score were calculated by the summation of the scores at stress and rest, respectively. The summed difference score was considered representative of the extent and severity of myocardial ischemia. Standard 17-segment-based scores were calculated and converted into percentage per myocardium by dividing the summed scores by the maximum potential score and multiplying by 100.
Clinical outcome data were obtained by contacting the patient, the patient’s general practitioner, and civil registries and reviewing hospital records. End points were cardiac death, nonfatal myocardial infarction, and late coronary revascularization. Cardiac death included death caused by acute myocardial infarction, significant arrhythmias, or refractory congestive heart failure and sudden death occurring without another explanation. Using the participants’ civil registration numbers, we linked individual-level information to differentiate cardiac death from noncardiac death. Hard cardiac events were defined as the occurrence of cardiac death or nonfatal myocardial infarction. The combined end point of cardiac death, nonfatal myocardial infarction, or coronary revascularization was considered as major adverse cardiac events.
SPSS version 22 (IBM, Armonk, New York) was used to analyze data. Variables are expressed as mean ± SD or as numbers. Continuous data were compared by using Student’s t test. Chi-square tests were used to compare categorical variables. Univariate and multivariable Cox proportional-hazards regression models were used to identify independent predictors of late cardiac events. Variables were selected in a stepwise forward selection manner, with entry and retention set at a p value of 0.05. A variable’s risk was expressed as a hazard ratio with a corresponding 95% confidence interval. The incremental value of abnormal results on myocardial perfusion scintigraphy over the clinical variables was determined using a multivariate analysis according to 3 models. In model 1, a scan with abnormal results was entered as a scanning variable. In model 2, the scanning variables, the presence of a fixed and reversible defect, were entered. In model 3, summed rest score and summed difference score were entered. The probability of survival was calculated by using the Kaplan-Meier method, and survival curves were compared by using the log-rank test. A p value <0.05 was considered to indicate statistical significance.
Results
The clinical data of the 473 patients are presented in Table 1 . During dobutamine stress testing, there were significant increases in heart rate (from 70 ± 14 to 136 ± 17 beats/min, p <0.001) and systolic blood pressure (from 140 ± 23 to 146 ± 31 mm Hg, p <0.001). The highest dobutamine dose was 10 μg/kg/min in 3 patients (1%), 20 μg/kg/min in 15 (3%), 30 μg/kg/min in 66 (14%), and 40 μg/kg/min in 389 (82%). Atropine was added in 196 patients (41%). Patients who received β blockers (120 of 185 [65%]) more frequently received atropine compared with those who did not receive β blockers (76 of 288 [26%]) (p <0.001). Test findings were inconclusive (failure to achieve target heart rate in the absence of perfusion abnormalities) in 43 patients (9%). These patients were not excluded from the prognostic data reported. No patients experienced myocardial infarction or ventricular fibrillation. Side effects were atrial fibrillation in 5 patients (1%), short ventricular tachycardia (<10 complexes) in 19 patients (4%), severe hypotension (decrease in systolic pressure >40 mm Hg), and severe hypertension (blood pressure >240/130 mm Hg) in 3 patients (0.6%). As minor side effects, nausea occurred in 18 patients (4%), chills in 22 (5%), and headache in 29 (6%).
| n = 473 | Number (%) |
|---|---|
| Age (years) | 61 ± 12 |
| Men | 273 (58%) |
| Hypertension | 214 (45%) |
| Diabetes mellitus | 69 (15%) |
| Smoker | 122 (26%) |
| Hypercholesterolemia | 116 (25%) |
| Congestive heart failure | 84 (18%) |
| Beta blocker therapy | 185 (39%) |
| Prior myocardial infarction | 210 (44%) |
| Previous coronary artery bypass graft | 92 (19%) |
| Previous percutaneous coronary intervention | 75 (16%) |
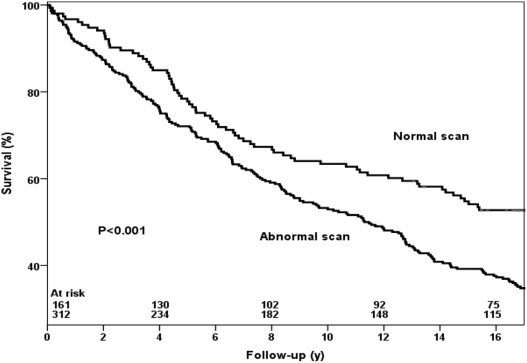
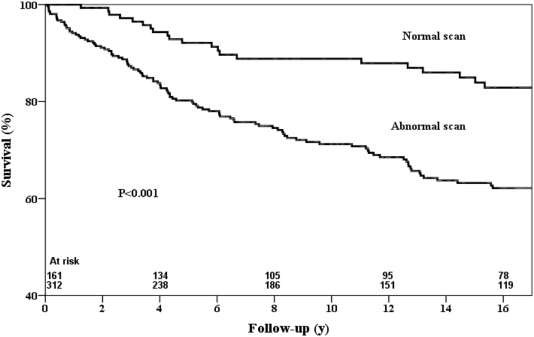
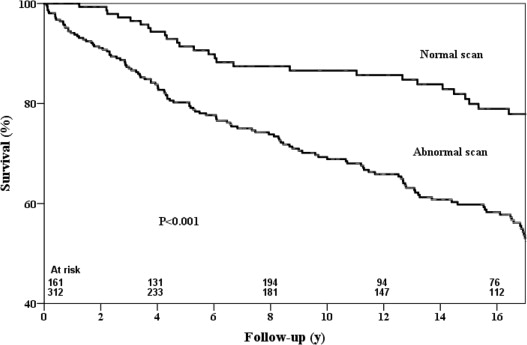
The results of SPECT were abnormal in 312 patients (66%). Perfusion abnormalities were reversible defects in 72 patients (15%). Most of the patients had fixed defects (126 patients [27%]), suggesting that they had myocardial damage. One hundred fourteen patients (24%) had fixed and reversible (or partially reversible) defects. During a mean follow-up period of 11.3 ± 6.7 years, 287 patients (61%) died (all-cause mortality), of whom 125 (26%) died due to cardiac causes. Nonfatal myocardial infarction occurred in 59 patients (12%). Late (>60 days) coronary revascularization was performed in 61 patients (13%). Kaplan-Meier curves in relation to all-cause mortality, cardiac death, hard cardiac events, and major adverse cardiac events are presented in Figures 1 to 4 . The survival curves demonstrate that patients with normal results on SPECT had a relatively low risk for all-cause mortality, cardiac death, hard cardiac events, and major cardiac events compared with those with abnormal findings. The annualized event rates for cardiac death for patients with normal results on SPECT were significantly lower than for those with abnormal findings (1.2% vs 2.5%, p <0.001). The annualized hard cardiac event rate for patients with normal results on SPECT was also significantly lower (3.4%) compared with patients with abnormal findings ([4.3%] p <0.001). The annualized rates for major adverse cardiac events were 2.2% in patients with normal results on SPECT and 4.4% in those with abnormal findings (p <0.001).

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


