Refractory angina pectoris (RAP) represents a clinical condition characterized by frequent episodes of chest pain despite therapy optimization. According to myocardial stunning and myocardial hibernation definitions, RAP should represent the ideal condition for systolic dysfunction development. We aim to investigate the evolution of left ventricular (LV) function in patients with RAP. A retrospective study which encompasses 144 patients with RAP referred to our institution from 1999 to December 2014 was performed. Of them, 88 met the inclusion criteria, and LV function was assessed by echocardiography. All of them had persistent angina episodes on top of optimal medical therapy and evidence of significant inducible myocardial ischemia and no further revascularization options. Nitrates consumption rate, time of angina duration, and the number of angina attacks were evaluated. In the whole population, ejection fraction (EF) was 44% ± 2. EF was significantly lower in patients with previous myocardial infarction (41% ± 1.5 vs 51% ± 1.8, p <0.0001). The duration time and the number of angina attacks did not correlate with EF in the whole population and in patients without previous myocardial infarction. In patients with previous myocardial infarction, the number of anginal attacks did not correlate with EF, but EF appeared higher in patients with angina duration >5 years (<5 years EF 37% ± 1 [n = 26]; >5 years 44% ± 2 [n = 44]; p 0.02). Long-term LV function in patients with RAP is generally preserved. A previous history of myocardial infarction is the only determinant in the development of systolic dysfunction. In conclusion, frequent angina attacks and a long-term history of angina are not apparently associated to worse LV function.
The prevalence of refractory angina pectoris (RAP) is steadily increasing in parallel with life expectancy. At present, despite the wide range of available antianginal drugs, the treatment of RAP can still be a frustrating exercise, very often not providing a definitive solution to patients’ symptoms. Apart from symptoms, several studies have described the consequences on myocardial function of repetitive ischemic attacks which can lead, through stunning and hibernating myocardium, to the continuous loss of myocytes and consequent definitive loss of function. It is therefore conceivable that in RAP, in the long term, impaired systolic function could develop as a consequence of repetitive episodes of transient myocardial ischemia. The aim of the present study is to analyze the effects of RAP on long-term left ventricular (LV) systolic function.
Methods
This was a retrospective study encompassing all RAP referred to our institution from 1999 to December 2014 for neurostimulator implantation, external counterpulsation, myocardial staminal cell therapy, Reducer implantation, or myocardial shockwave therapy. The clinical history of all of them was analyzed. Inclusion criteria were: patients with angiographically proved coronary artery disease, already revascularized where feasible, with persistent angina episodes, despite the implementation of optimal medical therapy and evidence of significant inducible myocardial ischemia as assessed by single-photon emission computed tomography (SPECT). All patients reported an excellent compliance to medical therapy. Optimal medical therapy included β blockers, calcium channel blockers, long-acting nitrates, ivabradine, ranolazine and trimetazidine, mostly in association ranging from 2 to 4 of the previously mentioned drug categories in each patient. Prescribed drugs were uptitrated to the maximal tolerated dose. Nitrates consumption rate, the number of angina attacks, and the Canadian Cardiovascular Society grading score were evaluated at the reference outpatient visit by considering the week preceding study inclusion; time of angina duration was also evaluated.
Rest/stress SPECT studies were performed with either symptoms limited treadmill exercise testing or pharmacologic stress (dipyridamole 0.56 mg/kg/4 minutes). Only patients with evidence of inducible ischemia in ≥2 myocardial adjacent SPECT segments were included in the study.
Echocardiographic studies were performed and reported by different cardiologist consultants. All studies were performed before the procedure (i.e., eurostimulator implantation, external counterpulsation, and so on). All the reports included a detailed description of all the morphologic aspects and the analysis of the LV systolic function. The presence of any severe valve disease was considered as an exclusion criteria. Systolic function was defined according to the ejection fraction (EF) formula and was calculated manually with biplane Simpson method in 2-dimensional echocardiography.
Data were expressed as mean ± SD, percentage, or median (range). Continuous variables were compared using either the unpaired t test or McNemar test where appropriate. Statistical significance was considered at a p <0.05. Statistical analysis was performed using GraphPad Prism 6.
Results
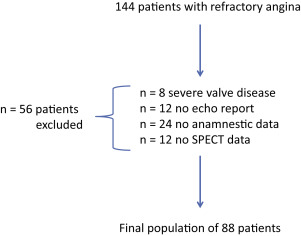
Of a total of 144 recruited patients with RAP, the final population encompassed 88 patients ( Figure 1 ). The baseline characteristics of the study population are reported in Table 1 . Twenty-four (27%) patients had had angina pectoris for >10 years, 20 (23%) for 5 to 10 years, 43 (49%) for 1 to 5 years, and 1 (1%) for <1 year. Seventeen patients (19%) reported >20 anginal attacks in the previous week, 32 (36%) from 10 to 20 attacks, whereas 45% referred up to 10 episodes. At the same time, >20 times/week nitrates tablets consumption was referred by 16 patients (18%), from 10 to 20 in 38% of patients (n = 33), or <10 times/week in 39 patients (44%).
| Characteristics | n (%) |
|---|---|
| Age (years) | 65±7.4 |
| Male | 69 (78%) |
| Comorbidities | |
| Diabetes Mellitus | 43 (49%) |
| Hypertension | 60 (68%) |
| Hyperlipidemia | 64 (73%) |
| Smokers | 40 (45%) |
| Medications | |
| Beta-blockers | 76 (87%) |
| ACEi | 58 (66%) |
| CCB | 50 (57%) |
| Nitrates | 62 (70%) |
| Statins | 73 (83%) |
| CCS class | |
| III | 18 (20%) |
| IV | 70 (80%) |
| Prior myocardial infarcstion | 32 (36%) |
| Number of narrowed coronary arteries | |
| 1 | 5 (6%) |
| 2 | 29 (33%) |
| 3 | 54 (61%) |
| Prior revascularization | |
| CABG | 37 (42%) |
| PCI | 31 (35%) |
| Both | 20 (23%) |
| Treatment for refractory angina pectoris | |
| Neurostimolator | 68 (77%) |
| Stem cell | 8 (9%) |
| Shockwave therapy | 10 (11%) |
| Reducer implantation | 2 (3%) |
In the whole population, EF was 44 ± 2%. EF was significantly lower in patients with a positive history of previous myocardial infarction (41 ± 1.5% vs 51 ± 1.8%, p <0.0001).
Angina duration time did not correlate with EF (42 ± 0.1% for <5 years; 46 ± 0.1% >5 years; 44 ± 0.1% for <10 years; 46 ± 0.1% >10 years; p = 0.4) and the number of angina attacks (41 ± 0.2% <10 attacks/week; 42 ± 0.3% >10 attacks/week; p = 0.13). In patients without previous myocardial infarction, EF was not influenced by the duration of angina (<5 years 50 ± 1% [n = 37]; >5 years 54 ± 2% [n = 12]; p = 0.07); (<10 years 51 ± 1% [n = 46]; >10 years 48 ± 1% [n = 3]; p = 0.2) and by the number of attacks (50 ± 0.1% <10 attacks [n = 38]; 54 ± 2% >10 attacks [n = 11]; p = 0.08).
Similarly, in patients with previous myocardial infarction, the number of anginal attacks did not correlate with EF (42 ± 2% <10 attacks [n = 30]; 41 ± 2% >10 attacks [n = 33]; p = 0.08). In the subpopulation of patients with previous myocardial infarction, EF appeared higher in patients with angina duration >5 years (<5 years EF 37 ± 1% [n = 26]; >5 years 44 ± 2% [n = 44]; p 0.02). This difference was not evident when comparing patients with previous myocardial infarction and >10 years of angina duration (<10 years 39 ± 1% [n = 37]; >10 years 44 ± 2% [n = 21]; p 0.14). The number of angina attacks did not correlate with EF (42 ± 2% <10 attacks [n = 33]; 41 ± 2% >10 attacks [n = 30]; p = 0.3).
Results
Of a total of 144 recruited patients with RAP, the final population encompassed 88 patients ( Figure 1 ). The baseline characteristics of the study population are reported in Table 1 . Twenty-four (27%) patients had had angina pectoris for >10 years, 20 (23%) for 5 to 10 years, 43 (49%) for 1 to 5 years, and 1 (1%) for <1 year. Seventeen patients (19%) reported >20 anginal attacks in the previous week, 32 (36%) from 10 to 20 attacks, whereas 45% referred up to 10 episodes. At the same time, >20 times/week nitrates tablets consumption was referred by 16 patients (18%), from 10 to 20 in 38% of patients (n = 33), or <10 times/week in 39 patients (44%).




