Obesity is pandemic in the Western Hemisphere, especially in the United States (US) and is associated with morbidity and mortality. Recent data show that a large proportion of the US population is at least overweight and almost 2 in 5 Americans are obese. This ongoing trend of increasing obesity rates has led to a thriving market for anorexigens. Despite the health benefits of weight loss, several anorexigens had devastating side effects including pulmonary vascular disease which manifests as the clinical syndrome of pulmonary arterial hypertension (PAH). PAH is an incurable and fatal disease and is characterized by vascular constriction, hypertrophy, and proliferation that over time lead to right-sided cardiac failure. Over the past few decades, several weight loss medications have been associated with the development of PAH, possibly caused by an increase in systemic serotonin levels, resulting in vasoconstriction of the pulmonary arteries and initiating a cascade of pathologic vascular remodeling leading to vascular fibrosis. Once sufficient evidence for the association of these drugs with PAH or other related pathologies was found, many were removed from the market. However, there are other appetite suppressants still currently on the market (whether Food and Drug Administration–approved or “dietary supplements”) that have to some extent similar mechanisms of action to those associated with PAH but lack robust enough data to prove or disprove an association. The serotonin pathway seems to be repeatedly implicated. In conclusion, given that PAH is a progressive and debilitating disease, it is important to highlight possible risk factors that could be avoided.
Obesity is a rising global epidemic associated with many fatal conditions, with high rates in North America. The worldwide prevalence of obesity has nearly doubled from 1980 to 2013. Mortality rates increase as body mass index increases. Pharmacotherapy may be recommended as an adjunct weight loss intervention. However, some of the efficacious weight loss medications were later found to cause devastating side effects and were taken off the market, which led to an ongoing controversy about the long-term safety of many currently available anorexigens. The serotonin (5-hydroxytryptamine, 5-HT) pathway has been repeatedly implicated in anorexigens-associated pulmonary vascular disease (PVD). We will briefly review in this study the pathophysiology of PVD and focus on the serotonin pathway. We do this as we tie together the potential for anorexigen-induced heart valvulopathy with PVD; both share similar serotonin mechanisms (including having both the receptors and the transmembrane transporters), and both are known side effects of anorexigens.
Pulmonary Arterial Hypertension
Pulmonary hypertension (PH) is a hemodynamic state associated with progressive and fatal diseases. The World Health Organization (WHO) has classified PH into 5 major categories based on etiologic and pathophysiological groupings. The first group is pulmonary arterial hypertension (PAH), known as WHO group 1 PH (idiopathic, heritable, drug/toxin induced, or associated with conditions such as connective tissue diseases, portal hypertension, or human immunodeficiency virus). The other 4 WHO groups of PH are left heart-, lung-, chronic thromboembolic-, and “miscellaneous” disease–associated PH.
There was a surge of drug-associated PAH in the 1960s related to the anorexigen aminorex fumarate, which prompted the first World Symposium on PH in 1973. Current guidelines classify drug-associated PAH into 4 categories ( Table 1 ).
| Likelihood of Association | Drugs |
|---|---|
| Definite | Aminorex Fenfluramine Dexfenfluramine Benfluorex In-utero exposure to SSRI’s |
| Likely | Amphetamines/methamphetamines L-tryptophan Dasatinib |
| Possible | Cocaine Phenylpropanolamine St. John’s wort Other chemotherapeutic agents Interferon alpha and beta |
| Unlikely | Cigarette smoking, oral contraceptives, estrogens |
The pathophysiology of PAH is complex but is known to at least involve endothelial cells, smooth muscle cells, and fibroblast dysfunction although many other cell types have also been implicated. The involved molecular derangements impair production of vasodilators including nitric oxide and prostacyclin and increase the production of vasoconstrictors and proinflammatory molecules such as endothelin-1, serotonin, and thromboxane-A. Systemic increase of serotonin in PAH is believed to be in the pathobiologic pathway of developing PAH that may act as a growth factor for pulmonary artery smooth muscle cells (PASMCs). These aberrant changes increase vascular tone and promote pathologic vascular remodeling, hypertrophy, in-situ thrombosis, platelets aggregation, and disruptive proliferation of the pulmonary arteries.
Despite significant advances in the therapeutic options for PAH, PAH continues to be an incurable and devastating disease. The estimated median survival of PAH without specific pulmonary vasodilators is about 2.8 years, and even with currently available therapies, patients with PAH still have a shortened life span.
Implicated Pathways Associated With PVD: The Serotonin System “Common Denominator”
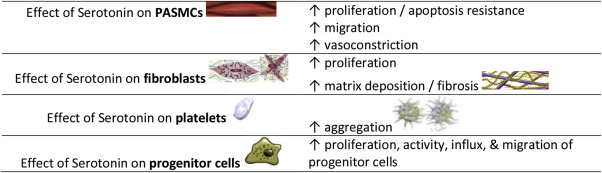
Serotonin is a potent vasoconstrictor. It mediates proliferation of the PASMCs and fibroblasts, migration of the PASMC, aggregation of platelets, and matrix deposition by fibroblasts ( Figure 1 ). Although the association with PAH has been well established (including in animal data), none of the currently approved medications to treat PAH directly target the serotonin pathway. Despite this established association, the serotonin pathway is complex and its full association with PVD is not fully understood.
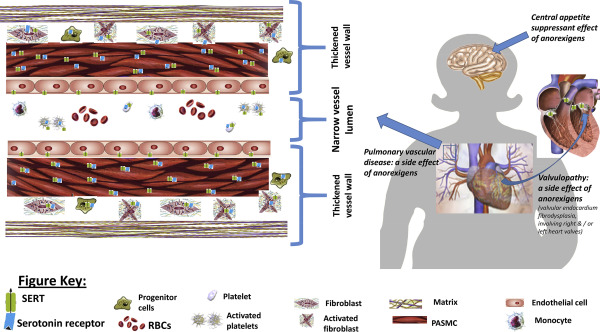
The serotonin system has 4 main components: membrane receptor, serotonin transporter (SERT), synthesis of serotonin (through tryptophan hydroxylase-1), and downstream effector molecules. SERTs are Na+/Cl− membrane transporters, which belong to the same transporter family as noradrenaline receptors. SERTs are present in neural, endothelial, and smooth muscle cells, which tie together the major effect (appetite suppression) and side effects of anorexigens (PVD and cardiac valvular disease; Figure 2 ). SERT gene polymorphism is associated with idiopathic PAH.
Receptors 5-HT 2A , 5-HT 2B , and 5-HT 2C are the 3 subtypes of the 5-HT 2 receptors that mediate the physiological functions of serotonin. The 5-HT 2B receptors have the strongest association with valvular heart disease and PH. The 5-HT 2C receptors are located in the central nervous system and have similar amino acid sequence homology to 5-HT 2A .
Some of the downstream effector molecules and signaling pathways involve reactive oxygen species, Rho Kinase, and many other kinases and growth factors. There seems to be a synergistic effect of serotonin with other vasoconstrictors such as endothelin-1, noradrenaline, and thromboxane-A which are known PAH pathologic molecules. Abnormalities in the homeostasis of the serotonin system are believed to be “second hits” that patients with bone morphogenetic protein receptor type-2 mutation for example require for the development of PAH.
Implicated Pathways Associated With PVD: The Serotonin System “Common Denominator”
Serotonin is a potent vasoconstrictor. It mediates proliferation of the PASMCs and fibroblasts, migration of the PASMC, aggregation of platelets, and matrix deposition by fibroblasts ( Figure 1 ). Although the association with PAH has been well established (including in animal data), none of the currently approved medications to treat PAH directly target the serotonin pathway. Despite this established association, the serotonin pathway is complex and its full association with PVD is not fully understood.
The serotonin system has 4 main components: membrane receptor, serotonin transporter (SERT), synthesis of serotonin (through tryptophan hydroxylase-1), and downstream effector molecules. SERTs are Na+/Cl− membrane transporters, which belong to the same transporter family as noradrenaline receptors. SERTs are present in neural, endothelial, and smooth muscle cells, which tie together the major effect (appetite suppression) and side effects of anorexigens (PVD and cardiac valvular disease; Figure 2 ). SERT gene polymorphism is associated with idiopathic PAH.
Receptors 5-HT 2A , 5-HT 2B , and 5-HT 2C are the 3 subtypes of the 5-HT 2 receptors that mediate the physiological functions of serotonin. The 5-HT 2B receptors have the strongest association with valvular heart disease and PH. The 5-HT 2C receptors are located in the central nervous system and have similar amino acid sequence homology to 5-HT 2A .
Some of the downstream effector molecules and signaling pathways involve reactive oxygen species, Rho Kinase, and many other kinases and growth factors. There seems to be a synergistic effect of serotonin with other vasoconstrictors such as endothelin-1, noradrenaline, and thromboxane-A which are known PAH pathologic molecules. Abnormalities in the homeostasis of the serotonin system are believed to be “second hits” that patients with bone morphogenetic protein receptor type-2 mutation for example require for the development of PAH.
Anorexigens
Although many anorexigens believed to cause PAH have been withdrawn from the market ( Table 2 ), a strong causal relation with PAH was never conclusively established. Several other weight loss medications are still currently approved by the US Food and Drug Administration (FDA; Table 3 ).
| Generic drug name | Mechanism of Action | Years on the market | Year removed from market |
|---|---|---|---|
| Fenfluramine | Serotonin-reuptake inhibitor | 24 | 1997 |
| Sibutramine | Serotonin-reuptake inhibitor | 13 | 2010 |
| Dexfenfluramine | Serotonin-reuptake inhibitor | 1 | 1997 |
| Aminorex fumarate | Central stimulant, indirect serotonin agonist (24) | 10 | 1972 |
| Benfluorex | Serotonin-reuptake inhibitor | 33 | 2009 |
| Chlorphentermine | Adrenergic agent, serotonin-reuptake inhibitor | 7 | 1969 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


