Despite improving success rate of percutaneous coronary intervention (PCI) for chronic total occlusion (CTO) lesions, the clinical benefit of recanalization of CTO is still a matter of debate. Of 13,087 patients who underwent PCI in the CREDO-Kyoto registry cohort-2, 1,524 patients received PCI for CTO (CTO-PCI). Clinical outcomes were compared between 1,192 patients with successful CTO-PCI and 332 patients with failed CTO-PCI. In-hospital death tended to occur less frequently in the successful CTO-PCI group than in the failed CTO-PCI group (1.4% vs 3.0%, p = 0.053). Through 3-year follow-up, the cumulative incidence of all-cause death was not significantly different between the successful and failed CTO-PCI groups (9.0% vs 13.1%, p = 0.18), whereas the cumulative incidence of cardiac death was significantly less in the successful CTO-PCI group than in the failed CTO-PCI group (4.5% vs 8.4%, p = 0.03). However, after adjusting confounders, successful CTO-PCI was associated with lesser risk for neither all-cause death (hazard ratio 0.93, 95% confidence interval 0.64 to 1.37, p = 0.69) nor cardiac death (hazard ratio 0.71, 95% confidence interval 0.44 to 1.16, p = 0.16). The cumulative incidence of coronary artery bypass grafting (CABG) was remarkably less in patients with successful PCI compared with those with failed PCI (1.8% vs 19.6%, p <0.0001). In conclusion, successful CTO-PCI compared with failed PCI was not associated with lesser risk for 3-year mortality. However, successful CTO-PCI was associated with significantly less subsequent CABG.
Percutaneous coronary intervention (PCI) for chronic total occlusion (CTO) has dramatically changed in recent years. The improvement of devices such as the guidewires, microcatheters, and low-profile balloon catheters and refinement of operator techniques such as parallel wire technique and retrograde approach have contributed to the improved success rate for PCI for CTO (CTO-PCI), although the penetration rates of parallel wire technique and retrograde approach might be different between Japan and outside Japan. Furthermore, introduction of drug-eluting stents has significantly reduced the restenosis and reocclusion rates in the CTO lesions. Successful CTO-PCI has been reported to be associated with less subsequent coronary artery bypass grafting (CABG), improvement of left ventricular function, and relief of symptoms. There are several reports that successful CTO-PCI improved the long-term survival outcomes after revascularization. Recently, Mehran et al and Jones et al also reported that successful CTO-PCI was independently associated with lesser cardiac mortality. However, many previous studies were associated with relatively low procedural success rates. Procedural success rate itself might have significant influence in analyzing the effect of successful CTO-PCI on survival outcome. Survival outcome after CTO-PCI should also be investigated in a population with relatively high procedural success rates. Therefore, we analyzed the impact of successful CTO-PCI on cardiovascular outcomes in a large Japanese observational database of patients who underwent first coronary revascularization.
Methods
The Coronary REvascularization Demonstrating Outcome study in Kyoto (CREDO-Kyoto) PCI/CABG registry cohort-2 is a multicenter registry enrolling consecutive patients undergoing first coronary revascularization procedures at 26 centers in Japan from January 2005 to December 2007 ( Supplementary Appendix A ). The relevant review boards or ethics committees in all participating centers approved the research protocol. Because of retrospective enrollment, written informed consents from the patients were waived. However, we excluded those patients who refused participation in the study when contacted for follow-up. This strategy is concordant with the guidelines for epidemiologic studies issued by the Ministry of Health, Labor and Welfare of Japan.
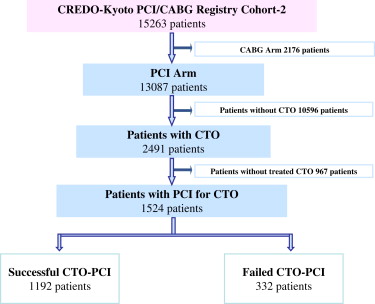
The design and patient enrollment of the CREDO-Kyoto PCI/CABG registry cohort-2 has been described previously. Of 15,263 patients, 13,087 patients underwent PCI as their first coronary revascularization procedure during the 3-year enrollment period. Of 2,491 patients (19%) with ≥1 CTO lesion, 1,524 patients underwent attempt of PCI for CTO lesions. PCI for ≥1 CTO lesion was successful in 1,192 patients (successful CTO-PCI group), whereas PCI for CTO lesions was unsuccessful in 332 patients (failed CTO-PCI group, 78% initial patient success rate for CTO; Figure 1 ). The number of cases and initial success rate of CTO-PCI in each participating center are illustrated in Supplemental Figure 1 . In the successful PCI group, 1,230 of 1,245 CTO lesions in 1,192 patients were successfully treated (1,154 patients had 1 treated CTO lesion and 38 patients had 2 treated CTO lesions). A total of 2,032 stents were used in the successful CTO-PCI group; 1,589 (78%) were drug-eluting stents and 443 (22%) were bare-metal stents. In the failed PCI group, no CTO lesion of the 339 CTO lesions in 332 patients was successfully treated, whereas 262 non-CTO lesions were successfully treated in 177 patients. In the present prespecified substudy of the CREDO-Kyoto PCI/CABG registry cohort-2, we compared the 3-year clinical outcome between the successful and failed CTO-PCI groups.
Definitions of baseline clinical characteristics were described previously. CTO was defined as complete obstruction of the vessel with Thrombolysis In Myocardial Infarction flow of 0 or 1 with an estimated duration of the occlusion >1 month or presence of collateral flow. The duration of occlusion was judged by the investigators in each participating center on the basis of the interval from the last episode of myocardial infarction (MI) in the target vessel territory, the previous coronary angiography, or changes in electrocardiographic findings. Procedural success was defined as a final diameter stenosis of <50% and a Thrombolysis In Myocardial Infarction flow of 2 or 3.
All-cause death was regarded as the primary outcome measure in the present analysis. Cardiac death, MI, stroke, stent thrombosis (ST), CABG, and any coronary revascularization were also assessed as end points. Death was regarded as cardiac in origin unless an obvious noncardiac cause could be identified. Any death during the index hospitalization was regarded as cardiac death. MI was defined according to the definition in the Arterial Revascularization Therapy Study. Within 1 week of the index procedure, only Q-wave MI was adjudicated as MI. Stroke was defined as ischemic or hemorrhagic stroke either occurring during the index hospitalization or requiring hospitalization with symptoms lasting >24 hours. ST was defined according to the Academic Research Consortium definition. Academic Research Consortium–definite ST was used as the end point for ST in the present study. The recommended antiplatelet regimen was aspirin (≥81 mg/day) indefinitely and thienopyridine (200 mg/day ticlopidine or 75 mg/day clopidogrel) for ≥3 months. Duration of antiplatelet therapy was left to the discretion of each attending physician.
Demographic, angiographic, and procedural data were collected from hospital charts or databases according to the prespecified definitions by the experienced clinical research coordinators in the independent clinical research organization (Research Institute for Production Development, Kyoto, Japan; Supplementary Appendix B ). Follow-up data were collected from hospital charts, by contacting patients, or by referring physicians. Death, MI, stroke, and ST were adjudicated against original source documents by a clinical event committee ( Supplementary Appendix C ). Median follow-up duration was 934 days (interquartile range [IQR] 669 to 1,243).
Categorical variables were compared with the chi-square test. Continuous variables were expressed as mean ± SD or median and IQR. Continuous variables were compared using the Student’s t test or Wilcoxon rank-sum test according to their distributions. Cumulative incidence was estimated by the Kaplan-Meier method, and differences were assessed with the log-rank test. We used Cox proportional hazard models to estimate the risk of the successful CTO-PCI group relative to the failed CTO-PCI group adjusting for the differences in patient characteristics, procedural factors, and medications. In consistent with our previous reports, we selected 34 clinically relevant factors listed in Table 1 as potential independent risk-adjusting variables. Independent correlates for all-cause death were identified by a backward elimination procedure ( Supplemental Table 1 ). The final model incorporated the successful CTO-PCI together with 8 variables remaining after the backward procedure. Adjusted analysis for the other end points was performed using the same 8 risk-adjusting variables as used in the analysis for all-cause death. The continuous variables were dichotomized by clinically meaningful reference values or median values. The effect of the successful CTO-PCI (the successful CTO-PCI group compared with the failed CTO-PCI group) was expressed as hazard ratios and their 95% confidence intervals. Posthoc subgroup analysis was also conducted for an exploratory purpose in several clinically relevant subgroups. Statistical analyses were conducted by 2 physicians (EY and MN) and by a statistician (TM) using JMP 10.0 (SAS Institute Inc., Cary, North Carolina) and SAS 9.2 (SAS Institute Inc., Cary, North Carolina) softwares. All the statistical analyses were 2-tailed. p Values <0.05 were considered statistically significant.
| Variable | Success (n = 1,192) | Failure (n = 332) | p |
|---|---|---|---|
| Clinical characteristics | |||
| Age (yrs) | 66.9 ± 10.8 | 66.2 ± 10.7 | 0.32 |
| Age ≥75 ∗ | 324 (27) | 80 (24) | 0.26 |
| Men ∗ | 926 (78) | 253 (76) | 0.57 |
| BMI (kg/m 2 ) | 24.2 ± 3.6 | 24.3 ± 3.6 | 0.82 |
| BMI <25.0 † | 762 (64) | 205 (62) | 0.47 |
| Acute MI ∗ | 101 (8.5) | 63 (19) | <0.0001 |
| Hypertension ∗ | 989 (83) | 290 (87) | 0.055 |
| Diabetes mellitus | 498 (42) | 141 (42) | 0.82 |
| On insulin therapy ∗ | 114 (9.6) | 32 (9.6) | 0.97 |
| Current smoker ∗ | 389 (33) | 118 (36) | 0.32 |
| Heart failure † | 258 (22) | 81 (24) | 0.29 |
| Shock at presentation ∗ | 25 (2.1) | 19 (5.7) | 0.001 |
| Multivessel coronary disease † | 853 (72) | 277 (83) | <0.0001 |
| Mitral regurgitation grade 3/4 ∗ | 65 (7.1) | 31 (13) | 0.005 |
| Ejection fraction (%) | 55.4 ± 13.4 | 54.3 ± 14.6 | 0.23 |
| Previous MI ∗ | 381 (32) | 80 (24) | 0.006 |
| Previous stroke ∗ | 178 (15) | 56 (17) | 0.39 |
| Peripheral vascular disease ∗ | 93 (7.8) | 27 (8.1) | 0.84 |
| eGFR <30, not on dialysis † | 45 (3.8) | 13 (3.9) | 0.91 |
| Dialysis † | 43 (3.6) | 27 (8.1) | 0.0005 |
| Atrial fibrillation ∗ | 99 (8.3) | 26 (7.8) | 0.78 |
| Anemia (hemoglobin <11 g/dl) † | 131 (11) | 40 (12) | 0.59 |
| Platelet <100 × 10 9 /L ∗ | 17 (1.4) | 4 (1.2) | 0.76 |
| Chronic obstructive pulmonary disease ∗ | 35 (2.9) | 11 (3.3) | 0.72 |
| Liver cirrhosis ∗ | 27 (2.3) | 8 (2.4) | 0.88 |
| Malignancy ∗ | 80 (6.7) | 26 (7.8) | 0.48 |
| Procedural characteristics | |||
| Number of target lesions | 1.8 ± 0.9 | 1.8 ± 0.9 | 0.96 |
| Number of target vessels | 1.6 ± 0.7 | 1.6 ± 0.7 | 0.88 |
| Number of CTO vessels | 1.1 ± 0.4 | 1.2 ± 0.4 | 0.4 |
| Number of target CTO vessels | 1.0 ± 0.2 | 1.0 ± 0.1 | 0.053 |
| Location of target CTO | |||
| Left anterior descending | 505 (42) | 121 (36) | 0.053 |
| Proximal left anterior descending ∗ | 458 (38) | 111 (33) | 0.1 |
| Left circumflex | 346 (29) | 88 (27) | 0.37 |
| Right | 507 (43) | 176 (53) | 0.0007 |
| Unprotected left main ∗ | 1 (0.1) | 0 | 0.6 |
| Contrast media volume | 211 (150–303) | 207 (146–300) | 0.26 |
| Baseline medication | |||
| Antiplatelet therapy | |||
| Thienopyridine | 1,172 (98) | 303 (91) | <0.0001 |
| Ticlopidine | 1,058 (91) | 279 (92) | 0.42 |
| Clopidogrel | 110 (9.4) | 24 (7.9) | |
| Aspirin | 1,181 (99) | 322 (97) | 0.004 |
| Cilostazol ∗ | 140 (12) | 48 (14) | 0.18 |
| Other medications | |||
| Statin † | 633 (53) | 160 (48) | 0.11 |
| β Blockers ∗ | 379 (32) | 124 (37) | 0.06 |
| ACE-I/ARB † | 678 (57) | 195 (59) | 0.55 |
| Nitrates ∗ | 475 (40) | 155 (47) | 0.03 |
| Calcium channel blockers ∗ | 488 (41) | 140 (42) | 0.69 |
| Nicorandil ∗ | 303 (25) | 93 (28) | 0.34 |
| Warfarin ∗ | 99 (8.3) | 28 (8.4) | 0.94 |
| Proton pump inhibitors ∗ | 278 (23) | 71 (21) | 0.46 |
| H 2 blockers ∗ | 267 (22) | 86 (26) | 0.18 |
∗ Potential independent variables selected for Cox proportional hazard models.
Results
At baseline, acute MI, shock at presentation, multivessel disease, moderate to severe mitral regurgitation, and dialysis were more prevalent in the failed CTO-PCI group than in the successful CTO-PCI group, whereas previous MI was more common in the successful CTO-PCI group. Regarding lesion and procedural characteristics, right coronary artery was more frequently targeted in the failed CTO-PCI group than in the successful PCI group. Aspirin and thienopyridine were more frequently used in the successful CTO-PCI group than in the failed CTO-PCI group, whereas nitrates were more frequently used in the failed CTO-PCI group ( Table 1 ).
Regarding the procedural complications, coronary perforation was significantly more common in the failed CTO-PCI group than in the successful CTO-PCI group. However, there was no significant difference in the incidences of coronary dissection, cardiac tamponade, and pericardial drainage between the 2 groups ( Table 2 ). Regarding the in-hospital adverse events, incidence of death and MI tended to be less in the successful CTO-PCI group. However, there was no significant difference in the incidence of stroke between the 2 groups ( Table 2 ).
| Variable | Success, n = 1,192 (%) | Failure, n = 332 (%) | p |
|---|---|---|---|
| Procedural complications | |||
| Coronary dissection | 12 (1.0) | 5 (1.5) | 0.44 |
| Coronary perforation | 7 (0.6) | 10 (3.0) | 0.0002 |
| Cardiac tamponade | 3 (0.3) | 2 (0.6) | 0.32 |
| Pericardial drainage | 0 | 1 (0.3) | 0.06 |
| In-hospital adverse events | |||
| Death | 17 (1.4) | 10 (3.0) | 0.053 |
| MI | 10 (0.8) | 7 (2.1) | 0.053 |
| Stroke | 5 (0.4) | 2 (0.6) | 0.66 |
| Coronary bypass | 0 | 1 (0.3) | 0.06 |
| Any coronary revascularization | 13 (1.1) | 8 (2.4) | 0.07 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


