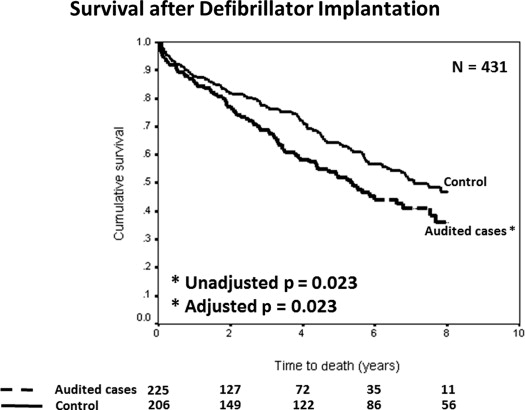
Institutions across the United States have been subjected to a federal audit for defibrillator implantable cardioverter defibrillator [ICD] implantations that violated the Centers for Medicare and Medicaid payment policy. We examined the long-term outcome of ICD recipients whose implantation procedures were audited by the Department of Justice (DOJ). Patients (n = 225) included in the DOJ audit at the University of Pittsburgh Medical Center between the years 2003 and 2010 were followed to the end point of all-cause mortality. A cohort of 206 consecutive and contemporary ICD recipients not included in the federal audit served as controls. Compared with the controls, the audited cases were older (p <0.001), had more preserved ejection fraction (p <0.001), and were less likely to be implanted for a primary prevention indication (p = 0.001). They also had significantly shorter time from myocardial infarction (p <0.001) or revascularization (p <0.001) to ICD implantation. Over a median follow-up of 3.6 years, 187 patients died and 71 received ICD therapy for ventricular arrhythmias. Patients whose cases were audited had worse survival compared with controls (hazard ratio 1.41, 95% confidence interval 1.05 to 1.90, p = 0.023) even after correcting for differences in baseline characteristics (hazard ratio 1.46, 95% confidence interval 1.05 to 2.02, p = 0.023). Rates of appropriate and inappropriate ICD therapies were similar between the audited cases and controls. In conclusion, patients whose ICD implantations were audited by the DOJ have worse long-term survival compared with nonaudited control patients. These data support compliance with the Centers for Medicare and Medicaid guidelines when the individual patient’s clinical condition allows it.
Implantable cardioverter defibrillators (ICDs) reduce all-cause mortality in survivors of sudden cardiac arrest and in patients with severe cardiomyopathy and improve morbidity and mortality in heart failure patients with wide QRS duration (≥120 ms). The beneficial effect of the ICD in reducing total mortality has resulted in expanding indications as detailed in the joint American College of Cardiology, American Heart Association, and Heart Rhythm Society published guidelines for device therapy and in revised Centers for Medicare and Medicaid (CMS) payment policy. Recently, a retrospective analysis of the National Cardiovascular Data Registry-ICD Registry demonstrated that about 22% of all ICDs implanted in the United States are nonevidence based. In addition, the Department of Justice (DOJ) has been conducting over the past 2 years a federal civil investigation auditing many institutions across the United States to determine whether claims submitted for payment for ICD implantation were compliant with the CMS payment policies. In response to this audit, the medical community has described the complexities of real-life practice of evidence-based medicine. In the light of these recent developments, we investigated the outcome of patients whose ICD implantation was subject to DOJ audit at our institution using as control a cohort of consecutive, contemporary patients who received an evidence-based ICD.
Methods
Patients implanted with an ICD device and followed at the hospitals of the University of Pittsburgh Medical Center and whose charts were included in the DOJ audit constituted our study cohort (n = 225). Contemporary and consecutive patients implanted with a new ICD at the same institution in the years 2004 and 2005 and who were not included in the DOJ audit served as controls (n = 206). Baseline demographic and clinical data were obtained on all patients from the electronic medical record. Indications for defibrillator implantation were ascertained in all patients. The time from last myocardial infarction or coronary revascularization to ICD implantation was recorded. Because the study group included overwhelmingly patients with ischemic cardiomyopathy (98%), the control cohort was selected to consist exclusively of ischemic cardiomyopathy patients.
Patients were followed to the end point of death or ICD therapy. Data were collected from scanned ICD records on appropriate and inappropriate ICD shocks or antitachycardia pacing. Appropriate ICD therapy was defined as any ICD therapy delivered in response to ventricular arrhythmia. Inappropriate ICD therapy was defined as all other causes of ICD therapy. Event adjudication was performed by a trained electrophysiologist and compared with the clinical determination of the nature of ICD event by the treating electrophysiologist (100% agreement). This study analysis was approved by the internal review board of the University of Pittsburgh.
All continuous variables are presented as mean ± SD and were compared using the analysis of variance test or t test. All categorical variables are presented as a number and percentage and were compared using the chi-square test. Kaplan-Meier curves were constructed for the time to death or ICD therapy and were compared using the log-rank test. Covariates that can affect the time to death were included in a multivariate Cox proportional hazard model. A 2-sided p value <0.05 was considered statistically significant. All statistical analyses were performed on SPSS, version 10.1 (SPSS, Chicago, IL).
Results
Between the years 2003 and 2010, 225 patients implanted with an ICD at one of the hospitals of the University of Pittsburgh Medical Center and followed at the same institution were included in the federal audit conducted by the DOJ. Of the patients included in the federal audit, the earliest date of ICD implantation was October 3, 2003, and the last one was May 3, 2010. Clinical characteristics of patients included in this cohort are listed in Table 1 . Briefly, the study cohort consisted primarily of white men, overwhelmingly with ischemic cardiomyopathy. Two-thirds of the patients were implanted for primary prevention of sudden cardiac death, and the majority received a dual-chamber ICD, whereas 31% received a cardiac resynchronization therapy ICD.
| Variable | Patients Included in DOJ Audit (N = 225) | Control Patients (N = 206) | p Value |
|---|---|---|---|
| Age (years) | 72 ± 11 | 68 ± 11 | <0.001 |
| Men | 76% | 74% | 0.60 |
| White | 90% | 96% | 0.026 |
| Atrial fibrillation | 25% | 30% | 0.23 |
| Primary prevention | 64% | 79% | 0.001 |
| Ejection fraction (%) | 28 ± 12 | 24 ± 8 | <0.001 |
| Plasma creatinine (mg/dL) | 1.6 ± 1.3 | 1.5 ± 1.3 | 0.36 |
| QRS duration (ms) | 124 ± 31 | 130 ± 31 | 0.048 |
| Type of ICD | 0.033 | ||
| • Single chamber | 13% | 8% | |
| • Dual chamber | 56% | 50% | |
| • Biventricular | 31% | 42% | |
| Prior myocardial infarction | 64% | 78% | 0.001 |
| Prior coronary revascularization | 77% | 65% | 0.006 |
| Time from MI to ICD implantation (days) | 10 ± 9 | 2641 ± 2429 | <0.001 |
| Time from coronary revascularization to ICD implantation (days) | 597 ± 1374 | 2168 ± 1930 | <0.001 |
| Length of hospital stay for ICD implantation (days) | 9.2 ± 6.6 | 3.4 ± 4.9 | <0.001 |
| Beta-blockers | 92.5% | 90.5% | 0.50 |
| Anti-arrhythmic drugs | 18.8% | 12.1% | 0.17 |
The charts of the 225 patients were audited by the DOJ because of a shorter than 40-day interval from a diagnosis of myocardial infarction (n = 97) or shorter than 90-day interval from coronary revascularization (n = 80) to ICD implantation or both (n = 48). The average interval from myocardial infarction to ICD implantation was 10 ± 9 days and from coronary revascularization to ICD implantation was 597 ± 1,374 days.
A cohort of 206 consecutive ICD recipients implanted in the years 2004 and 2005 at the hospitals of the University of Pittsburgh Medical center and not included in the federal audit was selected as controls. The baseline characteristics of the control group are listed in Table 1 . The audited cases and controls had significant differences in their baseline characteristics. As detailed in Table 1 , compared with the controls, the audited cases were older, had more preserved ejection fraction, and were less likely to be implanted for a primary prevention indication. They were also less likely to have had a myocardial infarction before their ICD implantation but more likely to have undergone surgical or percutaneous revascularization. As expected, audited cases had a significantly and profoundly shorter duration from myocardial infarction or coronary revascularization to ICD implantation.
Clinical events during follow-up are summarized in Table 2 . Over a mean follow-up of 3.96 ± 3.10 (median = 3.60, interquartile range = 1.02 to 6.65) years, 187 patients died and 71 received ICD therapy for ventricular arrhythmias. The rates of appropriate and inappropriate ICD therapies were balanced between the 2 groups ( Table 2 ). Patients whose cases were audited had worse survival compared with controls (hazard ratio 1.41, 95% confidence interval 1.05 to 1.90, p = 0.023, Figure 1 ). After correcting for differences in baseline characteristics including age, race, ejection fraction, QRS duration, primary prevention indication, and history of myocardial infarction or revascularization, patients whose ICD implantation was audited by the DOJ still had significantly worse survival compared with controls (hazard ratio 1.46, 95% confidence interval 1.05 to 2.02, p = 0.023, Table 3 ).
| Patients Included in DOJ Audit (N = 225) | Control Patients (N = 206) | p Value | |
|---|---|---|---|
| Death | 91 (40%) | 96 (47%) | 0.20 |
| Appropriate ICD shock | 24 (11%) | 15 (7%) | 0.22 |
| Appropriate ICD ATP | 25 (11%) | 16 (8%) | 0.23 |
| Appropriate ICD therapy | 43 (19%) | 28 (14%) | 0.12 |
| Inappropriate ICD therapy | 5 (2%) | 7 (3%) | 0.46 |